Introduction
Lumbar disc herniation is the most common cause of
lumbar radiculopathy (1). The
majority of patients with lumbar disc herniation respond to
conservative treatment, but for those with persistent or
progressive symptoms of nerve root compression, surgical treatment
must be considered (2,3). Schwannomas are slow-growing, benign,
encapsulated tumors that originate from the Schwann cells in the
myelin sheath of nerve fibers (4).
Schwannomas are generally single tumors and account for 26% of all
intraspinal tumors that involve the lumbar spinal nerves. In
addition, they are usually benign, but can be locally aggressive
and cause neurological compromise (5). At present, no studies have reported
the co-existence of these pathologies and thus may confuse
physicians. This report presents a rare case of the co-existence of
two significant pathologies contributing to intradural and
extradural compression. The patient provided written informed
consent.
Case report
A 75-year-old female had been experiencing lower
back and right lower extremity pain since May 2011, which led them
to seek help from local medical clinics. The patient’s symptoms
were occasionally alleviated by medication and physiotherapy.
In January 2013, the patient visited an orthopedist.
Plain films of the lumbar spine revealed lumbar spondylosis, which
did not improve with pharmacotherapy. The patient then underwent a
magnetic resonance imaging (MRI) scan of the lumbar region,
confirming the diagnosis of spinal stenosis and intradural tumor.
An incidental intradural structure, which following gadolinium
injection became increasingly distinct, was noted and diagnosed as
a schwannoma (Fig. 1). The patient
then visited the Department of Orthopaedic Surgery, Busan Korea
Hospital (Busan, Korea) to be evaluated for surgical management. As
the patient exhibited improvement with medication and
physiotherapy, it was recommended that conservative treatment would
remain as the first-line treatment and surgery would only be
considered when the former was no longer effective.
In May 2013, the patient’s lower back pain worsened
suddenly and the patient experienced numbness and motor weakness of
the right lower extremities. Neurological examination revealed
weakness of the extensor hallucis longus and the gluteus medius.
The patient reported abnormal sensations in the right buttock and
lateral leg, however, bladder and bowel function were normal, and
no reduction in deep tendon reflex was identified. The results of
the straight leg-raising test were 40°/70° and the Patrick’s test
results were normal. These observations led to a suspected
diagnosis of a rapidly growing tumor with right L5
radiculopathy.
However, follow-up MRI scan revealed lumbar disc
herniation compressing the thecal sac and right neural foramen at
L4/5, and an intradural structure at the same level (Fig. 2). To remove the mass, the patient
underwent total L4 laminectomy. Microscopically, the intradural
tumor was successfully removed. The dura mater of the L4/5 was
opened microsurgically, allowing the nerve fibers involved in the
tumor to be identified. The involved fibers surrounding the tumor
were cut, and the lesion was resected, preserving the intact nerve
fibers. An upward migrated lumbar disc herniation at L4/5 was also
successfully removed.
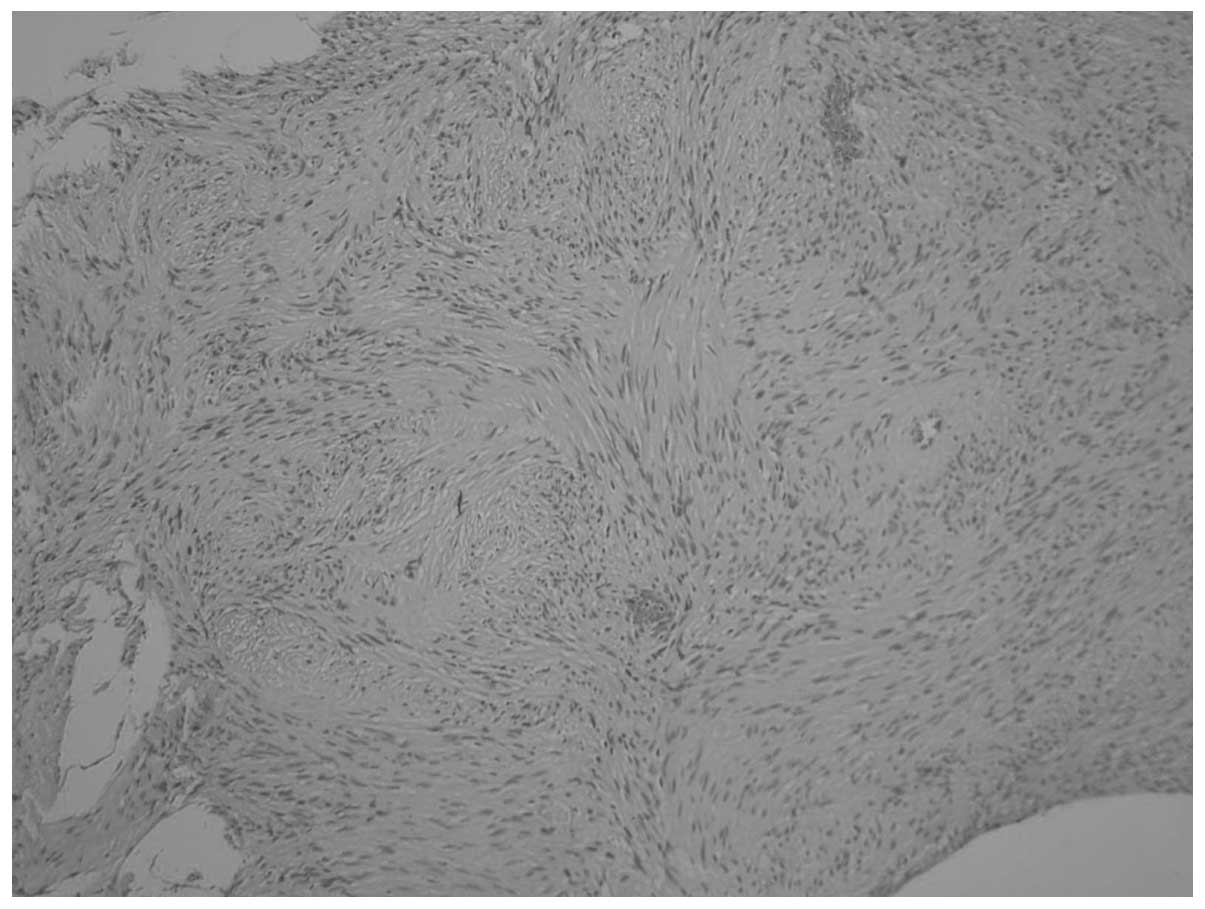
The pathological report confirmed the tumor to be a
schwannoma (Fig. 3). The
neurological status improved by the sixth postoperative week. At
the postoperative eighth month, the patient’s symptoms improved
significantly, with only a residual abnormal sensation on the skin
of the left buttock, which did not affect the patient’s normal
active life style.
Discussion
The present case report describes a patient with
intradural schwannoma whose symptoms initially improved with
conservative treatment, but later worsened with neurological
deficit. Further investigation using contrast-enhanced MRI
incidentally revealed disc herniation at the site of the intradural
tumor, which was exacerbating the pre-existing symptoms.
Coexistence of a lumbar disc herniation and a
proximal dorsal or cervical intradural tumor has not been reported
in cancer patients (6). The
simultaneous presence of upper and lower motor neuron symptoms in
the extremities validate the diagnosis. In the case of lumbar
intradural tumors, it is not uncommon for these lesions to simulate
symptoms of a prolapsed intervertebral disc (7). In the present case, the two lesions
compressed the cauda equina at the same level. Therefore, the
intradural tumor and herniated intervertebral discs were
removed.
The majority of intradural tumors follow a slow
progressive, indolent course and, thus, there may be lag period of
several months prior to the symptoms becoming evident (8,9). Lower
back pain and cauda equina syndrome generally result from larger
tumors, which impinge on multiple spinal root levels (10,11),
and tumors in the cauda equina often reach a considerable size
without painful symptoms, due to the mobility of the roots and the
wide intradural space (12).
However, the neurological impairment of the patient presented in
this case resulted from intradural and extradural compression.
Therefore, the possibility of tumor growth or increased disc
herniation must be ruled out to prevent delayed diagnosis and
treatment in cases where symptoms worsen, and in patients
undergoing conservative treatment for lumbar herniated
intervertebral disk (HIVD). Additionally, if symptoms acutely
worsen, the possibility of an intraspinal tumor must be
considered.
The detection of small and slow-growing schwannoma
accompanied by lumbar HIVD requires the use of MRI with contrast
enhancement. Although schwannoma and herniated IVD appeared bright
on T2-weighted MRI, only the schwannoma was shown by gadolinium
and, thus, the use of different contrast enhancement may be used to
distinguish between the two (13).
The preoperative detection of a schwannoma exhibits
a significantly positive impact on the outcome of surgery and
postoperative recovery. Spinal nerve compression due to tumors or
HIVD cannot be easily distinguished clinically. Therefore, a
complete history must be obtained and physical examination in
conjunction with investigative measures, such as MRI with contrast,
must be performed to ensure early diagnosis and implementation of
adequate treatment. Furthermore, physicians must not confirm the
diagnosis without performing full adequate studies.
References
|
1
|
Frymoyer JW: Back pain and sciatica. N
Engl J Med. 318:291–300. 1988.
|
|
2
|
Ellenberg MR, Ross ML, Honet JC, et al:
Prospective evaluation of the course of disc herniation in patients
with proven radiculopathy. Arch Phys Med Rehabil. 74:3–8. 1993.
|
|
3
|
Shapiro S: Medical realities of cauda
equina syndrome secondary to lumbar disc herniation. Spine.
25:348–351. 2000.
|
|
4
|
McCormick PC, Post KD and Stein BM:
Intradural extramedullary tumors in adults. Neurosurg Clin N Am.
1:591–608. 1990.
|
|
5
|
Sloof JL, Kernohan JW and MacCarty CS:
Primary Intramedullary Tumours of the Spinal Cord and Filum
Terminale. WB Saunders; Philadelphia: pp. 31–61. 1964
|
|
6
|
Takeuchi A, Miyamoto K, Hosoe H and
Shimizu K: Thoracic paraplegia due to missed thoracic compressive
lesions after lumbar spinal decompression surgery: report of three
cases. J Neurosurg. 100:71–74. 2004.
|
|
7
|
Wiesel SW, Ignatius P, Marvel JP Jr and
Rothman RH: Intradural neurofibroma simulating lumbar-disc disease.
Report of six cases. J Bone Joint Surg Am. 58:1040–1042. 1976.
|
|
8
|
Van Goethem JW, van den Hauwe L, Ozsarlak
O, De Schepper AM and Parizel PM: Spinal tumors. Eur J Radiol.
50:159–176. 2004.
|
|
9
|
Sevick RJ: Cervical spine tumors.
Neuroimaging Clin N Am. 5:385–400. 1995.
|
|
10
|
Caputo LA and Cusimano MD: Schwannoma of
the cauda equina. J Manipulative Physiol Ther. 20:124–129.
1997.
|
|
11
|
Crnalic S, Hildingsson C, Wikström P,
Bergh A, Löfvenberg R and Widmark A: Outcome after surgery for
metastatic spinal cord compression in 54 patients with prostate
cancer. Acta Orthop. 83:80–86. 2012.
|
|
12
|
Kagaya H, Abe E, Sato K, Shimada Y and
Kimura A: Giant cauda equina schwannoma. A case report. Spine
(Phila Pa 1976). 25:268–272. 2000.
|
|
13
|
Bradley WG: Use of contrast in MR imaging
of the lumbar spine. Magn Reson Imaging Clin N Am. 7:439–457.
vii1999.
|