Introduction
Bartholin gland carcinomas (BGCs) are extremely rare
tumors, accounting for <1% of all female genital malignancies.
BGCs commonly occur in postmenopausal female with a median age of
50 years at presentation (1). The
pathogenesis of BGC remains unknown; however, it may be associated
with infections of the vulva and Bartholin glands. Previous studies
have reported that BGC is associated with the etiologically of the
human papillomavirus (HPV) infection, particularly with HPV type 16
(2,3). Due to the deep location of Bartholin
glands and the lack of early clinical symptoms, BGC is commonly
misdiagnosed. Bilateral primary BGC is extremely rare. Furthermore,
BGC is classified into various histological types, including
adenocarcinoma, squamous, adenoid cystic, keratosis gland,
transitional cell and undifferentiated carcinomas, among which
adenocarcinoma and squamous carcinoma are the most common (3). The major transfer pathways include
local invasion, lymph node metastasis and hematogenous metastasis.
The diagnosis of BGC is dependent on pathological analysis and BGC
is predominantly treated by surgery, and integrated applications of
chemotherapy and radiotherapy are adopted for mid-term or advanced
cases. Although the traditional management of BGC is surgery,
clinical studies have demonstrated that multimodal therapy may be a
more effective strategy (4–6). The prognosis of BGC patients is poor
due to delayed treatment that results from misdiagnosis. Therefore,
the aim of the present study was demonstrate the importance of
early diagnosis and treatment of BGC, thus, improving the prognosis
of patients with BGCs.
Case report
A 49-year-old postmenopausal female was referred to
the Affiliated Hospital of Luzhou Medical College (Luzhou, China)
with an eight-year history of BGC. Written informed consent was
obtained from the participant. This study was conducted in
accordance with the Declaration of Helsinki and with approval from
the Ethics Committee of the Affiliated Hospital of Luzhou Medical
College.
Eight years ago, the patient presented with a hard,
fixed, ill-defined nodule (measuring 3×3×2 cm3), which
was identified unintentionally in the vulva. A left Bartholin cyst
was diagnosed at the Luzhou Natural Gas Chemical Plant Worker
Hospital (Luzhou, China) and the patient underwent left Bartholin
cyst fenestration. After two years, the patient presented to the
Affiliated Hospital of Luzhou Medical College with a new mass in
the same location and underwent an excisional biopsy. The biopsy
specimen was sent to the Department of Pathology, Affiliated
Hospital of Luzhou Medical College, and pathologically diagnosed as
left Bartholin adenoid cystic carcinoma (ACC). The patient
subsequently underwent a bilateral inguinal lymphadenectomy in the
Department of Gynaecology and Obstetrics, Affiliated Hospital of
Luzhou Medical College to cure the vulvar cancer. The pathological
examinations were consistent with the previous examination and
revealed that the lymph node exhibited reactive hyperplasia;
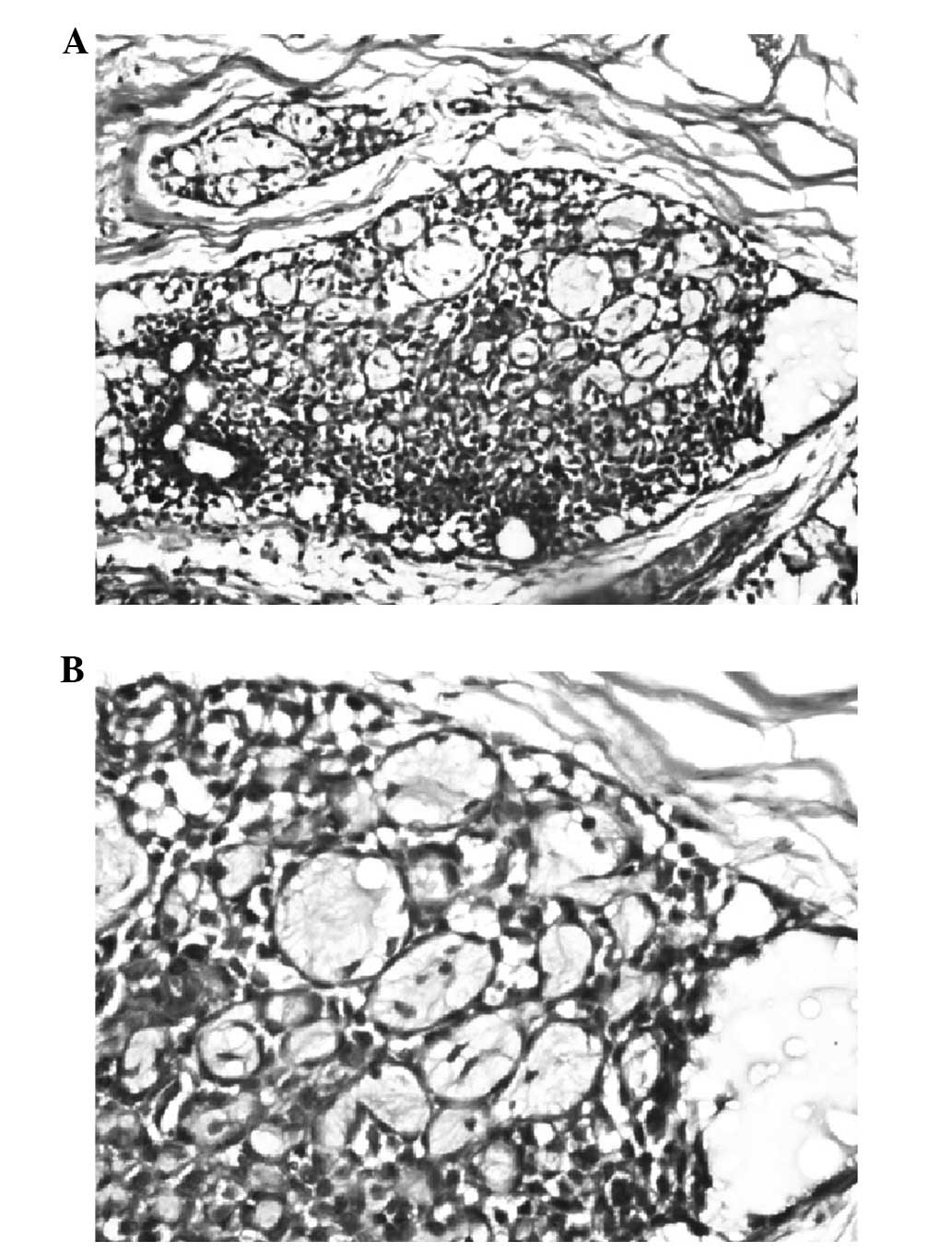
however, no cancer cells were found (Fig. 1). Postoperative magnetic resonance
imaging of the pelvis did not indicate any disease. The patient
received local radiation therapy (dose, 5,000 cGY/25F/5W) and
immunotherapy. Notably, three years subsequently, a palpable mass
measuring 1×1×1 cm3 was identified at the right side of
the perineum and cancer cells were detected via cytology. The
patient underwent simple mass excision. Pathological analysis
revealed an ACC of Bartholin’s gland. Chemotherapy and biological
therapy were performed. Positron emission tomography-computed
tomography revealed small nodules in the left upper lobe and lower
left abdominal subcutaneous nodules with increased glucose
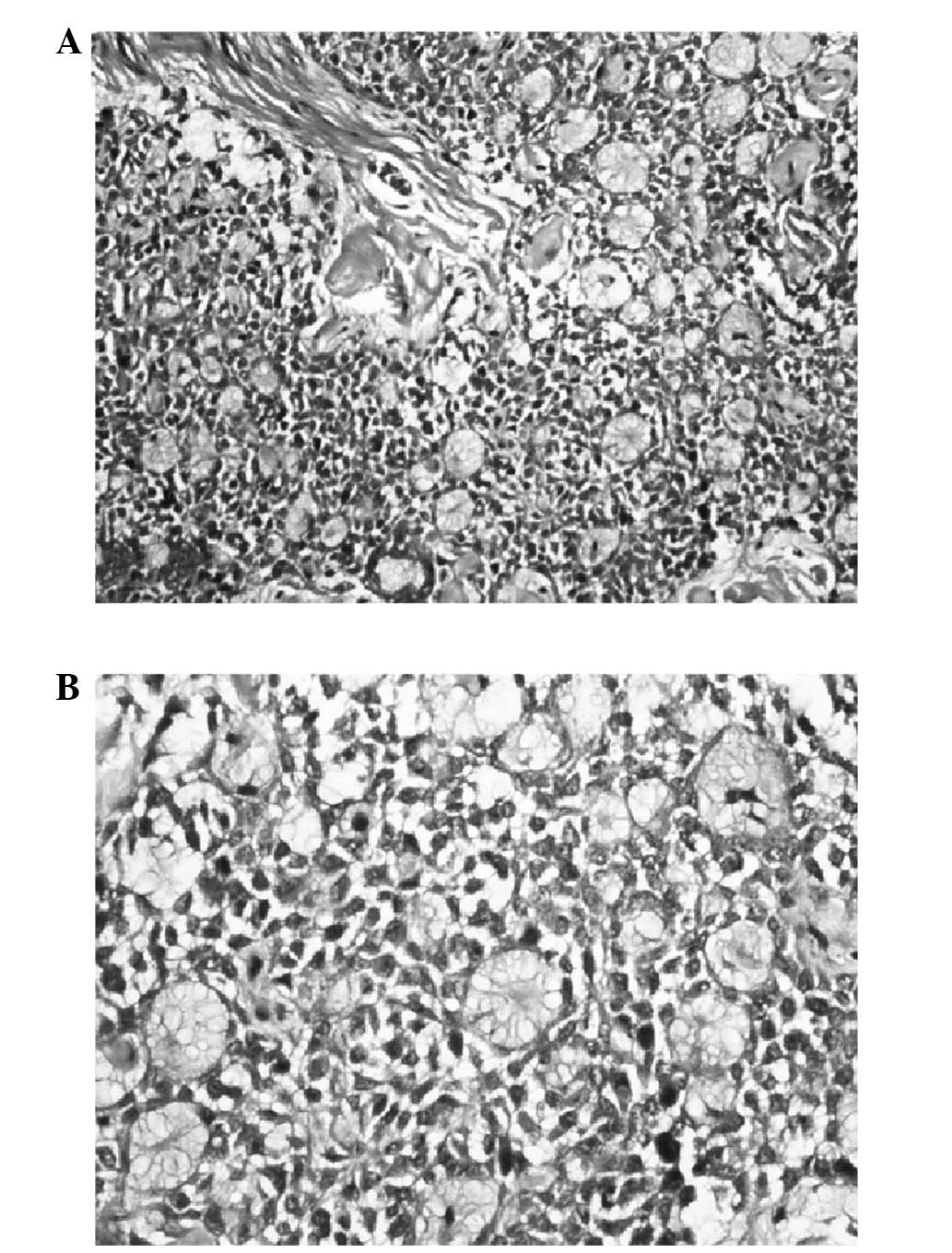
metabolism after six months. An abdominal wall mass excision biopsy
showed left lower abdominal metastatic ACC four months later
(Fig. 2). The patient underwent
four cycles of paclitaxel, cisplatin and fluorouracil chemotherapy;
however, chemotherapy was terminated as a result of severe
side-effects. The patient then underwent six cycles of biotherapy
at intervals of two to 12 months. Currently, and more than five
years after initial diagnosis, the patient continues to
survive.
Discussion
According to the literature, >300 cases of BGC
have been reported. The major histological types of BGC include
squamous cell and adenocarcinoma, and the other types include
adenoid-cystic, transitional or undifferentiated carcinomas; ACC
accounts for ~25% of all BGCs (6).
An extensive search of the currently available cases revealed that
only 62 were ACC of Bartholin’s gland (7). BGCs are slow-growing tumors associated
with frequent recurrences that exhibit local invasion, and
metastasis to tissues and/or organs. Bones and the lungs are the
most common sites of distant recurrence. Unilateral BGC is common,
while bilateral BGC is extremely rare. In the present study, the
patient was diagnosed with, and treated for, left Bartholin ACC.
However, three years later, right Bartholin ACC was diagnosed with
metastases to the abdominal wall and lungs. As a pathological
analysis was not initially performed, whether the right Bartholin
ACC was a primary cancer or metastatic carcinoma remains unknown.
This locally aggressive malignant neoplasm is commonly found in
postmenopausal females and occurs occasionally in women aged <40
years (8). Treatment following
initial recurrence extends the survival of patients, and overall
survival may reach 75 and 58% at five and 10 years, respectively
(3). As a result of numerous
treatment modalities, the patient in the present case has survived
for more than five years after the initial diagnosis of BGC.
BGCs are treated with various modalities, either
alone or in combination, including surgery, chemotherapy and
radiotherapy. Due to the lack of previous cases, no consensus
regarding the optimal treatment of BGC has been established.
The majority of authors recommend surgery as the
primary treatment when tumor invasion is limited. Major surgical
treatment methods include radical vulvectomy and inguinal and
pelvic lymph node dissection. However, the benefits of performing
either unilateral or bilateral inguinal-femoral lymphadenectomy
remain controversial. Leuchter et al (1) support bilateral dissection and
demonstrated that the inguinal-femoral lymph node status markedly
affects survival. Copeland et al (9) indicated that unilateral dissection and
postoperative adjuvant radiation are adequate to treat negative
nodes in the clinical setting. In the present study, bilateral
dissection was the preferred treatment method. In addition, our
patient was treated with adjuvant postoperative radiation,
chemotherapy, immunotherapy and biological therapy. However, the
benefits of performing aggressive surgical procedures alone and the
advantages of surgery compared with other treatment modalities for
BGC were not investigated. A wide range of surgical procedures are
available, however, surgery is extensive and often the incisions do
not heal well, which severly affect patient’s quality of life.
Radiotherapy is widely used for the treatment of
tumors, and the benefits of radiotherapy in the treatment of BGC
are significant. López-Varela et al (6) found that overall survival with primary
radiation or chemoradiation therapy was similar to the surgical
series reported by Leuchter et al (1) (71%) and Cardosi et al (67%)
(5), while it was inferior to
Copeland et al (84%) (9).
This phenomenon may be associated with the age and clinical stage
of the populations. The aim of primary radiation therapy is to
achieve the same outcome as surgery, reduce morbidity and optimally
preserve normal function (6).
Postoperative adjuvant radiotherapy has been shown to be effective
in controlling ACC in patients with positive margins and local
recurrences (10). However, certain
short-term secondary effects of radiation therapy remain, including
moist desquamation, erythema/dermatitis, bowel symptoms (including
diarrhea, constipation and temporary incontinence) and dry
desquamation (6). Fortunately,
these symptoms are easily cured.
Chemotherapeutic agents, such as cisplatin and
5-fluorouracil are commonly used to treat BGC in combination with
radiation therapy in clinics. Various cytostatic agents have been
assessed, however, the results were poor (11). Chemotherapeutic agents enhance the
effects of radiation via radiosensitization and direct
cytotoxicity; however, chemoradiation destroys the tumor and the
gland. Previous studies have achieved marked effects by treating
advanced cancers of the vulva with radiation and sensitizing
chemotherapy (12,13). Although surgery appears to be
superior to radiation alone in eliminating occult metastases among
vulvar cancer patients without clinically apparent metastasis
(14); chemoradiation may sterilize
occult metastases near the primary site, thus reducing the
requirement for wide resection margins.
Currently, the optimum treatment method for BGC has
not been determined, and the efficacy of radiation and chemotherapy
has not been clearly established. However, certain investigators
hypothesize that radiation therapy or chemoradiation offer
effective alternative strategies to surgery for the treatment of
BGC, whilst preserving genital function and maintaining low levels
of morbidity (4,6). In addition, early diagnosis combined
with a radical vulvectomy and bilateral inguinal femoral lymph node
dissection may optimize the patient’s likelihood of survival
(10). Patients that do not exhibit
metastatic lesions at early diagnosis should undergo cancer lesion
exeresis to reduce the tumor payload and increase the efficacy of
radiotherapy. When the cancer lesion is removed during surgery,
cancer cells may fall off and result in implantation metastasis. In
conclusion, multimodality therapy may be a particularly effective
treatment option, as indicated by the present study. However, by
increasing the number of reported cases of BGC, the optimal
treatment strategy for this type of carcinoma may be
determined.
References
|
1
|
Leuchter RS, Hacker NF, Voet RL, Berek JS,
Townsend DE and Lagasse LD: Primary carcinoma of the Bartholin
gland: a report of 14 cases and review of the literature. Obstet
Gynecol. 60:361–368. 1982.
|
|
2
|
Felix JC, Cote RJ, Kramer EE, Saigo P and
Goldman GH: Carcinomas of Bartholin’s gland. Histogenesis and the
etiological role of human papillomavirus. Am J Pathol. 142:925–933.
1993.
|
|
3
|
Hill DS and Butterfield A: Bartholin’s
gland squamous cell carcinoma, a rare vulvar neoplasm. Journal of
Diagnostic Medical Sonography. 26:296–298. 2010.
|
|
4
|
Massad LS and De Geest K: Multimodality
therapy for carcinoma of the Bartholin gland. Gynecol Oncol.
75:305–307. 1999.
|
|
5
|
Cardosi RJ, Speights A, Fiorica JV,
Grendys EC Jr, Hakam A and Hoffman MS: Bartholin’s gland carcinoma:
a 15-year experience. Gynecol Oncol. 82:247–251. 2001.
|
|
6
|
López-Varela E, Oliva E, McIntyre JF and
Fuller AF Jr: Primary treatment of Bartholin’s gland carcinoma with
radiation and chemoradiation: a report on ten consecutive cases.
Int J Gynecol Cancer. 17:661–667. 2007.
|
|
7
|
Yang SY, Lee JW, Kim WS, et al: Adenoid
cystic carcinoma of the Bartholin’s gland: report of two cases and
review of the literature. Gynecol Oncol. 100:422–425. 2006.
|
|
8
|
Kumar R, Singhal M, Acharya R and Chawla
N: Adenoid cystic carcinoma of Bartholin’s gland - A rare entity
likely to be misdiagnosed. Rev Esp Patol. 44:213–215. 2011.(In
Spanish).
|
|
9
|
Copeland LJ, Sneige N, Gershenson DM,
McGuffee VB, Abdul-Karim F and Rutledge FN: Bartholin gland
carcinoma. Obstet Gynecol. 67:794–801. 1986.
|
|
10
|
Hwang TL, Hung YC and Chang HW: Adenoid
cystic carcinoma of Bartholin’s gland. Taiwan J Obstet Gynecol.
51:119–120. 2012.
|
|
11
|
Haddley K: Trastuzumab emtansine for the
treatment of HER2-positive metastatic breast cancer. Drugs Today
(Barc). 49:701–715. 2013.
|
|
12
|
Wahlen SA, Slater JD, Wagner RJ, et al:
Concurrent radiation therapy and chemotherapy in the treatment of
primary squamous cell carcinoma of the vulva. Cancer. 75:2289–2294.
1995.
|
|
13
|
Cunningham MJ, Goyer RP, Gibbons SK,
Kredentser DC, Malfetano JH and Keys H: Primary radiation,
cisplatin, and 5-fluorouracil for advanced squamous carcinoma of
the vulva. Gynecol Oncol. 66:258–261. 1997.
|
|
14
|
Stehman FB, Bundy BN, Thomas G, et al:
Groin dissection versus groin radiation in carcinoma of the vulva:
a Gynecologic Oncology Group study. Int J Radiat Oncol Biol Phys.
24:389–396. 1992.
|