Introduction
Esophageal carcinoma is one of the most fatal types
of cancer with highly aggressive potency. Due to its poor prognosis
and high incidence rate, which exceeds 100 cases per 100,000
individuals per year in China (1).
it is important to investigate the initiation and progression of
esophageal squamous cell carcinoma (ESCC) and to study the
associated prognostic factors. Numerous genes and proteins with
abnormal expression and function have been investigated in the
pathogenesis of ESCC, such as epidermal growth factor receptor,
survivin and cyclooxygenase-2 (2–4).
However, the molecular mechanisms involved in the pathogenesis of
ESCC are not fully understood. CD146, a member of the
immunoglobulin gene superfamily, was first identified as a cell
adhesion molecule and a marker of melanoma progression and
metastasis (5). It has been
demonstrated that CD146 is expressed on vascular endothelium,
smooth muscle and other cells in normal tissue, and mediates
cation-independent adhesion through interactions with an
unidentified ligand on the surface of various cells (6).
Overexpression of CD146 has been identified in a
number of types of cancer, including melanoma, prostate cancer,
epithelial ovarian cancer and breast cancer (7–10). Its
expression levels have been found to correlate with tumor
progression and metastatic potential, thus establishing CD146 as an
important candidate molecule involved in tumor growth and
metastasis. However, at present, studies that report CD146
expression in ESCC patients are rare. Therefore, we evaluated the
expression of CD146 in ESCC and its association with
clinicopathological parameters, such as clinical stage of the
disease, in the present study.
Materials and methods
Patients and specimens
The expression of CD146 in 63 surgically resected
ESCC specimens and in 63 normal esophageal mucosa samples obtained
from ESCC patients was analyzed by immunohistochemistry. In total,
63 patients with ESCC underwent surgery at Linyi People’s Hospital
(Linyi, China), from August 2010 to February 2012. All patients
underwent total esophagectomy and radical lymph node dissection.
Normal esophageal mucosal samples were taken from a region >5 cm
distant from the cancer, as non-tumor control samples. There were
63 cases in the control group. Histopathological specimens were
fixed in 10% buffered formalin, processed routinely and embedded in
paraffin. All specimens were obtained from patients who had not
received chemotherapy and radiotherapy prior to surgery. Following
hematoxylin and eosin staining, all sections were reviewed and
reexamined. The grade of tumor differentiation was determined
according to the classification of the World Health Organization
2011 (11), and the clinical stage
was according to the tumor-node-metastasis classification system of
the International Union Against Cancer 2002 (12). The invasion depth was determined
according to the criteria of the International Union Against Cancer
2002 (12). The study was approved
by the ethics committee of Shandong Cancer Hospital of Shandong
University (Shandong, China). Patients provided written informed
consent.
Immunohistochemical staining
The specimens of ESCC and non-cancerous esophageal
mucosa were cut into 4- to 5-μm-thick sections and mounted onto
slides, deparaffinized with xylene, and rehydrated with graded
concentrations of ethanol. Endogenous peroxidase activity was
blocked with 3% hydrogen peroxide (H2O2) in
deionized water for 10 min. The slides were then washed three times
with phosphate-buffered saline (PBS, pH 7.2–7.4) buffer for 2 min.
An antigen retrieval technique was used before application of the
primary antibody (10 mmol/l sodium citrate solution, pH 6.0 in a
pressure cooker for 2–2.5 min). After three washes with PBS, an
aliquot of 50 μl of primary antibody (rabbit anti-human CD146
monoclonal antibody; ncl-cd146; Leica Biosystems, Newcastle Upon
Tyne, United Kingdom) was applied to each section and incubated at
37°C for 60 min. This was followed by washing three times with PBS,
and the antibodies were detected using the secondary antibody
detection kit Polink-1 PV-6000 (Zhongshan Goldenbridge
Biotechnology Co., Ltd., Beijing, China). Sections were stained
with 3,3′-diaminobenzidine (DAB) followed by distilled water. The
sections were lightly counterstained in Haris hematoxylin solution
(Zhongshan Goldenbridge Biotechnology Co., Ltd.) for microscopic
examination (BX53, Olympus Corporation, Tokyo, Japan). The section
were dehydration in an alcohol gradient, cleared with xylene and
mounted using neutral gum.
Simultaneously, each section was incubated with PBS
instead of the primary antibody as an internal negative control.
The immunostained specimens were analyzed by two independent
pathologists who were blinded to the patients’ clinicopathological
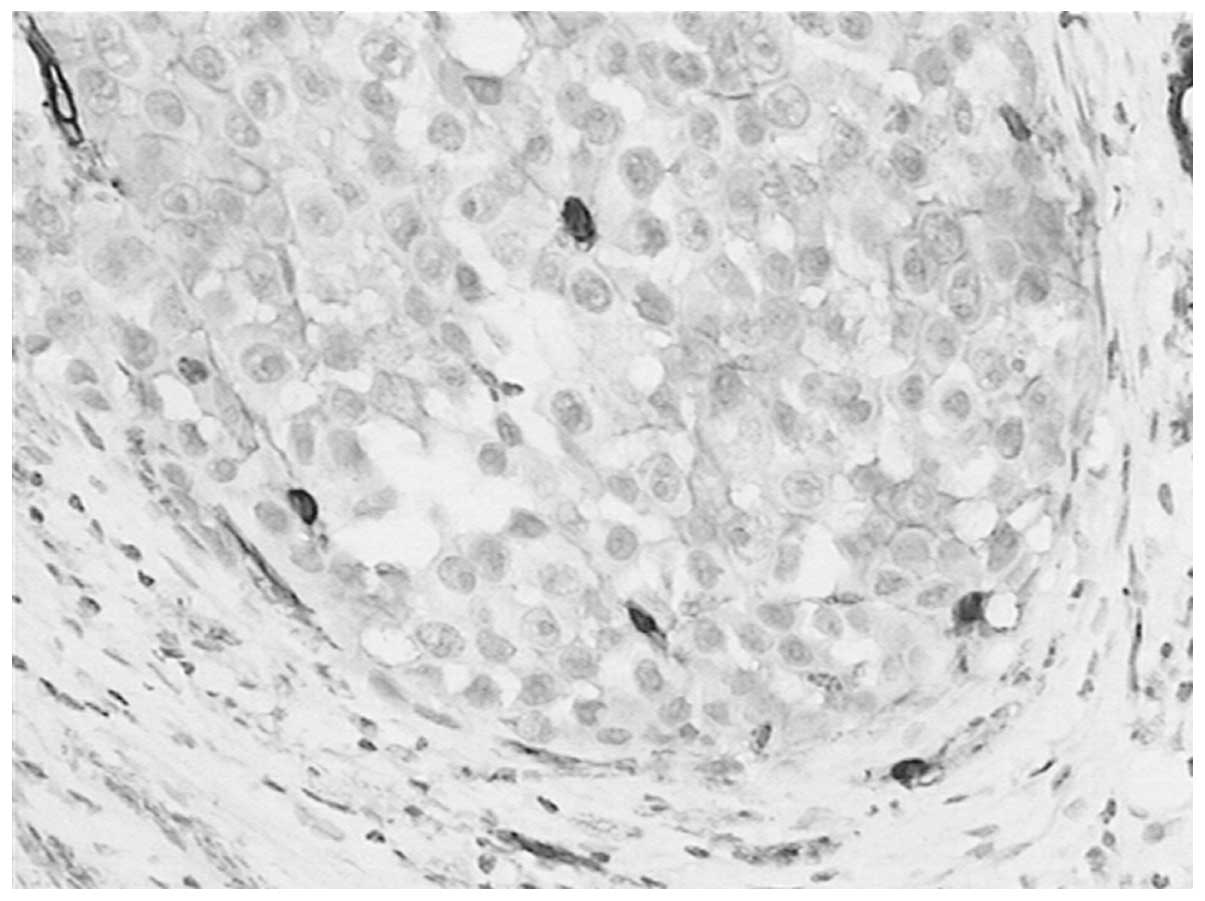
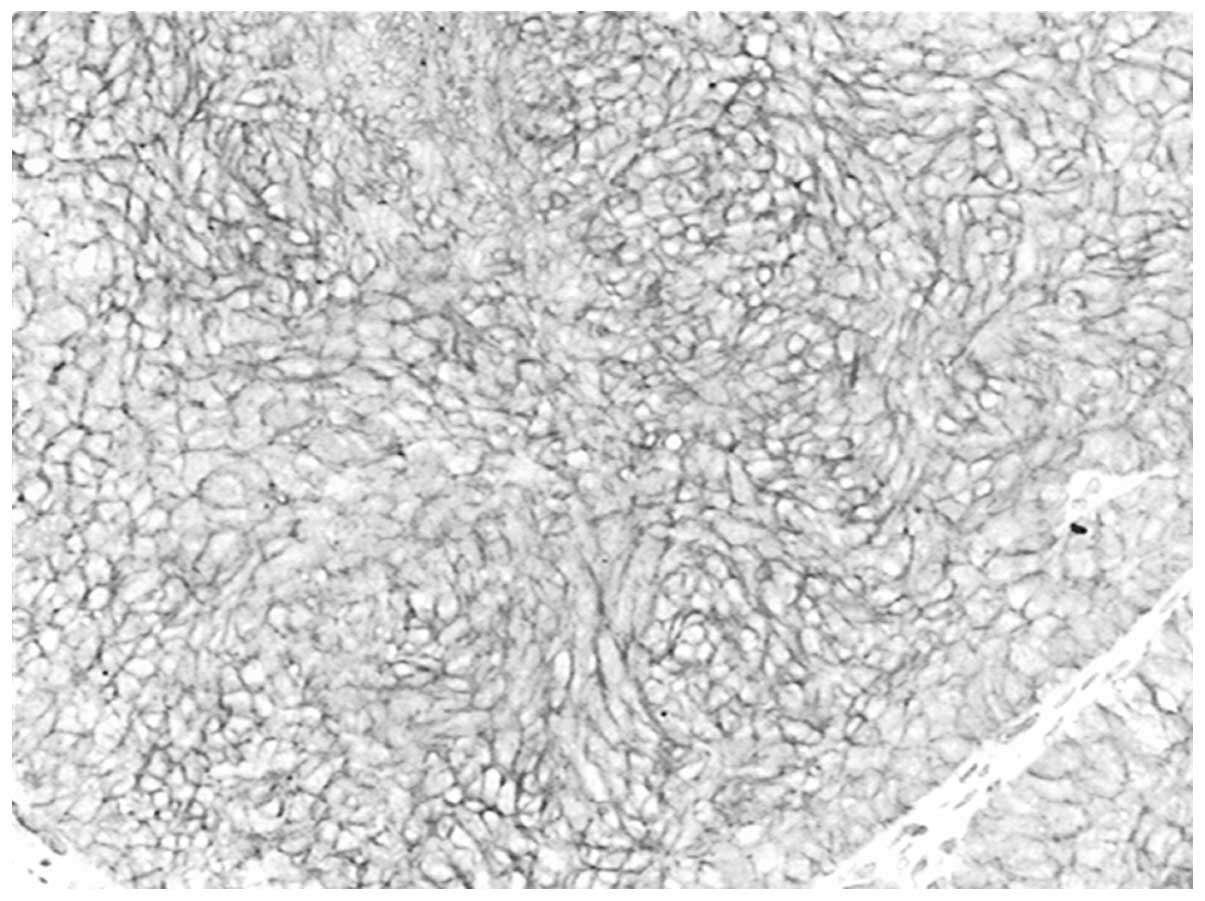
characteristics. Cytoplasm and membrane staining (brown reaction
product) was regarded as a positive staining result for CD146. Five
fields in each cancer and non-cancer section were evaluated at high
power (×400) to determine the proportion of immunostained tumor
cells and the staining intensity of the cytoplasm and membrane in
the entire sections. The staining strength was graded from 1 to 3:
1, no positive staining or a weak staining (Figs. 1 and 2); 2, weak to moderate staining (Fig 3); 3, moderate to strong staining
(Fig. 4). The case with positive
cells ≥25% and/or scores ≥2 was considered to be positive (13). At least five fields were observed,
the average score in each tumor and non-tumor sections served as
the result. All sections were scored twice to confirm the
reproducibility of the results, and the highest score from the two
observers was reported.
Follow-up
The patients were followed up every 3 months for the
first year and then every 6 months for the next 2 years. The total
follow-up period was defined as the time from diagnosis to the date
of death or the last follow-up appointment if patients remained
alive. All 63 patients were included in survival data analysis. The
last follow-up appointment was carried out in May 2013, with a mean
observation period of 17.6 months (range, 3–35 months).
Statistical analysis
All calculations were performed using SPSS software,
version 16.0 (SPSS, Inc., Chicago, IL, USA). The associations
between CD146 expression and clinicopathological variables were
assessed using the χ2 and Fisher’s exact tests. The
association between CD146 expression and survival time was assessed
using the Cox regression model. P<0.05 was considered to
indicate a statistically significant difference.
Results
Immunohistochemistry
Immunohistochemistry revealed that CD146-positive
staining was localized in the membrane and cytoplasm of tumor cells
in the tumor tissues. CD146 expression was identified in 46.0%
(29/63) of the ESCC samples, and no positive (weak to moderate or
moderate to strong)expression was found in the 63 normal squamous
epithelium samples (Fig. 5)
(χ2=27.248 P<0.0001). The negative control group was
underwent the same steps as previously described, with the
exception that the CD146 antibody was replaced with PBS (Fig. 6).
Associations between CD146 expression and
clinicopathological variables
The associations between CD146 expression and
clinicopathological variables were investigated. Positive
expression of CD146 was found in 46.0% (29/63) of the ESCC samples,
which was significantly higher than that in the normal esophageal
epithelium samples which demonstrated no immunostaining
(χ2=27.248; P<0.0001). CD146 expression was
associated with lymph node metastasis (χ2=5.117;
P=0.024) and advanced clinical stage (χ2=4.661;
P=0.031). No correlation was found with tumor size
(χ2=2.346; P=0.309), invasion depth
(χ2=0.962; P=0.327) or tumor differentiation status
(χ2=1.977; P=0.372) (Table
I).
 | Table ICorrelation between CD146 expression
and the clinicopathoclinical parameters in the ESCC group. |
Table I
Correlation between CD146 expression
and the clinicopathoclinical parameters in the ESCC group.
| Parameters |
CD146+ |
CD146− | P-value |
|---|
| Age, years |
| Range | 41–77 | |
| Mean | 62.4 | |
| Gender, n |
| Male | 60 | |
| Female | 3 | |
| Tumor size, n | | | 0.309 |
| ≤3 cm | 5 | 10 | |
| 3.1–6 cm | 17 | 20 | |
| >6 cm | 7 | 4 | |
| Invasion
deptha, n | | | 0.327 |
| T2 | 4 | 8 | |
| T3 | 25 | 26 | |
| Differentiation
statusb, n | | | 0.372 |
| Low | 5 | 4 | |
| Moderate | 19 | 19 | |
| High | 5 | 11 | |
| Lymph node
metastasis, n | | | 0.024 |
| No | 8 | 19 | |
| Yes | 21 | 15 | |
| Clinical
stagec, n | | | 0.031 |
| II | 10 | 21 | |
| III | 19 | 13 | |
Association between CD146 expression and
survival time
The mean survival time of patients with positive
CD146 expression was 15 months while that of patients with negative
CD146 expression was 25 months. In the multivariate analysis, the
association between CD146 expression and survival time was
statistically significant (HR, 2.838; 95% CI: 1.102–7.305; P=0.031)
(Fig. 7).
Discussion
CD146 is a cell-cell or cell-matrix adhesion
molecule that was first described in melanoma (5). Previous studies have indicated that
CD146 expression correlates with the malignant progression and
metastatic potential of human melanoma cells (14–18).
Expression of CD146 has been observed in certain normal human
tissues and numerous malignancies, such as non-small cell lung
cancer, gallbladder adenocarcinoma and gastric cancer (13,19,20).
The current study demonstrated that CD146 expression was
significantly higher in ESCC than in the normal esophageal mucosal
tissue. Additionally, it was identified that CD146 expression was
associated with lymph node metastasis (P=0.024) and advanced
clinical stage (P=0.031) in ESCC. However, no correlations between
CD146 expression and tumor size (P=0.309), invasion depth (P=0.327)
and differentiation grading (P=0.372) were identified. The results
shown in Table I demonstrate that
five of the nine low differentiation patients, 19 of the 38
moderate differentiation patients and five of the 16 high
differentiation patients were positive for immunohistochemical
expression. In addition, the results showed that in tumors with low
and intermediate differentiation, the expression of CD146 was
higher than that in highly differentiated tumors (55.6, 50.0 and
31.3% respectively), although the differences were not
statistically significant. Similarly, 4 of the 12 T2 patients and
25 of the 51 T3 patients were positive for immunohistochemical
expression, while five of the 15 patients with tumor sizes of ≤3
cm, 17 of the 37 patients with tumor sizes of 3.1–6 cm and 7 of the
11 patients with tumor sizes of >6 cm were positive for
immunohistochemical expression. CD146 expression in T3 tumors
(49.0%) was higher than that in T2 tumors (33.3%), and the levels
of expression increased with an increase in tumor size (33.3, 45.9,
63.6%), although the results were not statistically significant.
The results of the present study demonstrated that CD146 may have a
role in malignant progression in esophageal squamous cell carcinoma
and may be associated with a more aggressive tumor phenotype. Liu
et al (20) reported that
CD146 expression correlated positively with lymph node involvement
in gastric cancer patients. The results of the present study are
consistent with this finding in gastric cancer.
CD146 expression has been found to be correlated
with aggressiveness and development of metastasis, and is a
predictor of worse prognosis in certain cancer types (21). Advanced tumor stage is an important
prognostic factor for solid tumors. CD146 is associated with an
advanced tumor stage in melanoma, prostate cancer, ovarian cancer
and triple-negative breast cancer (7–9,22). In
the present study, CD146 was demonstrated to be associated with an
advanced tumor stage in ESCC. Metastasis occurs through a series of
steps, including local invasion, intravasation, transport,
extravasation and colonization (23). Epithelial to mesenchymal transition
is a process in which the epithelial cells lose polarity and
develop a mesenchymal phenotype and has been implicated in the
initiation of metastasis (22).
CD146 is a component of the inter-endothelial junction (24), and is now recognized as a marker of
mesenchymal cells (25). CD146 may
directly or indirectly contribute to tumor aggressiveness by
promoting malignant cell motility (10). The presence of lymph node metastasis
is an important factor in the clinical evaluation of esophageal
cancer patients (26).
Lymphangiogenesis is a significant step in the lymphatic metastasis
of tumors. Neonatal lymph vessels finally cause metastasis to
regional lymph nodes. A previous study has found that lymph vessel
density has a close association with progression, metastasis and
prognosis of malignant tumors (13). A study by Sundar and Ganesan
indicated that tumor-induced lymphangiogenesis was a predictive
indicator of metastasis to lymph nodes (27). Tumor-secreted cytokines, such as
vascular endothelial growth factors (VEGF)-C and -D, bind to VEGF
receptors on lymphatic endothelial cells and induce proliferation
and growth of new lymphatic capillaries. This process is similar to
the well known mechanism of angiogenesis; the proliferation of new
blood vessel capillaries (28). Luo
et al (14) reported that
CD146 directly interacts with actin-linking ezrin-radixin-moesin
(ERM) proteins and recruits ERM proteins to cell protrusions,
promoting the formation and elongation of microvilli and leading to
cytoskeleton remodeling and finally cell migration. However, the
exact molecular mechanism whereby CD146 is involved in lymph node
metastasis remains unknown. Further studies are required to
investigate this issue.
It is well acknowledged that advanced stage and
lymph node metastasis are important prognostic factors for ESCC.
The current study demonstrated that CD146 expression was associated
with advanced clinical stage and lymph node metastasis in ESCC
patients, and was therefore an indicator of poor prognosis in these
patients. Overexpression of the CD146 gene was one of the important
phenotypes and characteristics in ESCC carcinomatous change. This
study suggests an important role for CD146 in the development of
ESCC. CD146 may present as a potential therapeutic target for the
individualized treatment of ESCC.
References
|
1
|
Li JS, Ying JM, Wang XM, et al: Promoter
methylation of tumor suppressor genes in esophageal squamous cell
carcinoma. Chin J Cancer. 32:3–11. 2013.
|
|
2
|
Sarbia M, Ott N, Pühringer-Oppermann F and
Brucher BL: The predictive value of molecular markers (p53, EGFR,
ATM, CHK2) in multimodally treated squamous cell carcinoma of the
oesophagus. Br J Cancer. 97:1404–1408. 2007.
|
|
3
|
Li C, Li Z, Zhu M, et al:
Clinicopathological and prognostic significance of survivin
over-expression in patients with esophageal squamous cell
carcinoma: a meta-analysis. PLoS One. 7:e447642012.
|
|
4
|
Kuo KT, Chow KC, Wu YC, et al:
Clinicopathologic significance of cyclooxygenase-2 overexpression
in esophageal squamous cell carcinoma. Ann Thorac Surg. 76:909–914.
2003.
|
|
5
|
Lehmann JM, Riethmuller G and Johnson JP:
MUC18, a marker of tumor progression in human melanoma, shows
sequence similarity to the neural cell adhesion molecules of the
immunoglobulin superfamily. Proc Natl Acad Sci USA. 86:9891–9895.
1989.
|
|
6
|
Ouhtit A, Gaur RL, Abd Elmageed ZY, et al:
Towards understanding the mode of action of the multifaceted cell
adhesion receptor CD146. Biochim Biophys Acta. 1795:130–136.
2009.
|
|
7
|
Melnikova VO, Balasubramanian K, Villares
GJ, et al: Crosstalk between protease-activated receptor 1 and
platelet-activating factor receptor regulates melanoma cell
adhesion molecule (MCAM/MUC18) expression and melanoma metastasis.
J Biol Chem. 284:28845–28855. 2009.
|
|
8
|
Wu GJ, Peng Q, Fu P, et al: Ectopical
expression of human MUC18 increases metastasis of human prostate
cancer cells. Gene. 327:201–213. 2004.
|
|
9
|
Aldovini D, Demichelis F, Doglioni C, et
al: M- CAM expression as marker of poor prognosis in epithelial
ovarian cancer. Int J Cancer. 119:1920–1926. 2006.
|
|
10
|
Zabouo G, Imbert AM, Jacquemier J, et al:
CD146 expression is associated with a poor prognosis in human
breast tumors and with enhanced motility in breast cancer cell
lines. Breast Cancer Res. 11:R12009.
|
|
11
|
Gabbert HZ, Shimoda T, Hainaut P, et al:
Tumours of the oesophagus. World Health Organization Classification
of Tumours: Pathology and Genetics of Tumours of the Digestive
System. Hamilton SR and Alaltonen LA: IARC Press; Lyon: pp. 10–16.
2000
|
|
12
|
TNM Classification of the Esophagus.
International Union Against Cancer; 6th edition. J Willy &
Sons; New York, NY: pp. 2–25. 2002
|
|
13
|
Wang W, Yang ZL, Liu JQ, Jiang S and Miao
XY: Identification of CD146 expression, angiogenesis, and
lymphangiogenesis as progression, metastasis, and poor prognosis
related markers for gallbladder adenocarcinoma. Tumour Biol.
33:173–182. 2012.
|
|
14
|
Luo Y, Zheng C, Zhang J, et al:
Recognition of CD146 as an ERM-binding protein offers novel
mechanisms for melanoma cell migration. Oncogene. 31:306–321.
2012.
|
|
15
|
Luca M, Hunt B, Bucana CD, et al: Direct
correlation between MUC18 expression and metastatic potential of
human melanoma cells. Melanoma Res. 3:35–41. 1993.
|
|
16
|
Johnson JP: Cell adhesion molecules in the
development and progression of malignant melanoma. 18:345–357.
1999.
|
|
17
|
Xie S, Luca M, Huang S, et al: Expression
of MCAM/MUC18 by human melanoma cells leads to increased tumor
growth and metastasis. Cancer Res. 57:2295–2303. 1997.
|
|
18
|
Zabouo G, Imbert AM, Jacquemier J, et al:
CD146 expression is associated with a poor prognosis in human
breast tumors and with enhanced motility in breast cancer cell
lines. Breast Cancer Res. 11:R12009.
|
|
19
|
Kristiansen G, Yu Y, Schluns K, et al:
Expression of the cell adhesion molecule CD146/MCAM in non-small
cell lung cancer. Anal Cell Pathol. 25:77–81. 2003.
|
|
20
|
Liu WF, Ji SR, Sun JJ, et al: CD146
Expression correlates with epithelial-mesenchymal transition
markers and a poor prognosis in gastric cancer. Int J Mol Sci.
13:6399–6406. 2012.
|
|
21
|
Shih I-M, Nesbit M, Herlyn M and Kurman
RJ: A new Mel-CAM (CD146)-specific monoclonal antibody, MN-4, on
paraffin-embedded tissue. Mod Pathol. 11:1098–1106. 1998.
|
|
22
|
Zeng Q, Li W, Lu D, et al: CD146, an
epithelial-mesenchymal transition inducer, is associated with
triple-negative breast cancer. Proc Natl Acad Sci USA.
109:1127–1132. 2012.
|
|
23
|
Tsai JH and Yang J: Epithelial-mesenchymal
plasticity in carcinoma metastasis. Genes Dev. 27:2192–2206.
2013.
|
|
24
|
Bardin N, Anfosso F, Masse JM, et al:
Identification of CD146 as a component of the endothelial junction
involved in the control of cell-cell cohesion. Blood. 98:3677–3684.
2001.
|
|
25
|
Delorme B, Ringe J, Gallay N, et al:
Specific plasma membrane protein phenotype of culture-amplified and
native human bone marrow mesenchymal stem cells. Blood.
111:2631–2635. 2008.
|
|
26
|
Tanaka T, Ishiguro H, Kuwabara Y, et al:
Vascular endothelial growth factor C (VEGF-C) in esophageal cancer
correlates with lymph node metastasis and poor patient prognosis. J
Exp Clin Cancer Res. 29:832010.
|
|
27
|
Sundar SS and Ganesan TS: Role of
lymphangiogenesis in cancer. J Clin Oncol. 25:4298–4207. 2007.
|
|
28
|
Nathanson SD: Insights into the mechanisms
of lymph node metastasis. Cancer. 98:413–423. 2003.
|