Introduction
Desmoplastic fibroma is a benign bone tumor, which
is composed of spindle cells with minimal cytological atypia and
abundant collagen production (1)
that was initially described by Jaffe in 1958 (2). It is a particularly rare tumor with
~200 cases reported in the English literature to date (3,4).
Desmoplastic fibromas are often locally progressive and aggressive
(1). In cases where the tumors are
located in the extremities, the recurrence rates following
multi-modality treatments have been reported to be ≤55% (3). Although a standard treatment protocol
for desmoplastic fibroma has not been established owing to the
rarity of the disease, marginal or wide excision of tumors
occurring in large bones is often advocated for the initial
treatment due to the high recurrence rates following curettage. A
recurrence rate of 55–72% has been reported following non-resection
procedures, whereas tumor recurrence has been noted in only 17% of
resection cases (1,3). Based on this data, previous case
studies have indicated that, despite the greater functional loss,
surgeons primarily opted for en-bloc or wide resection of the
tumors followed by reconstruction, rather than curettage (4–7). In
the present report, the case of a 26-year-old male athlete with
desmoplastic fibroma of the distal femur is described. The tumor
was treated by extended curettage with a high-speed burr, followed
by heat ablation using a standard electrosurgical knife and
reconstruction of the bony defect using artificial bone grafting.
The patient was tumor free at the 12-year follow-up examination and
exhibited excellent functional outcomes. These results indicate
that desmoplastic fibromas occurring in the femur do not always
require resection and that extended curettage with heat ablation
may be an appropriate primary procedure for disease treatment.
Case report
A previously healthy 26-year-old male visited
Kurauchi Orthopaedic Hospital (Miyazaki, Japan) for increasing pain
in the left femur that began one year previously. Despite being a
marathon runner, the patient had no history of trauma to this area.
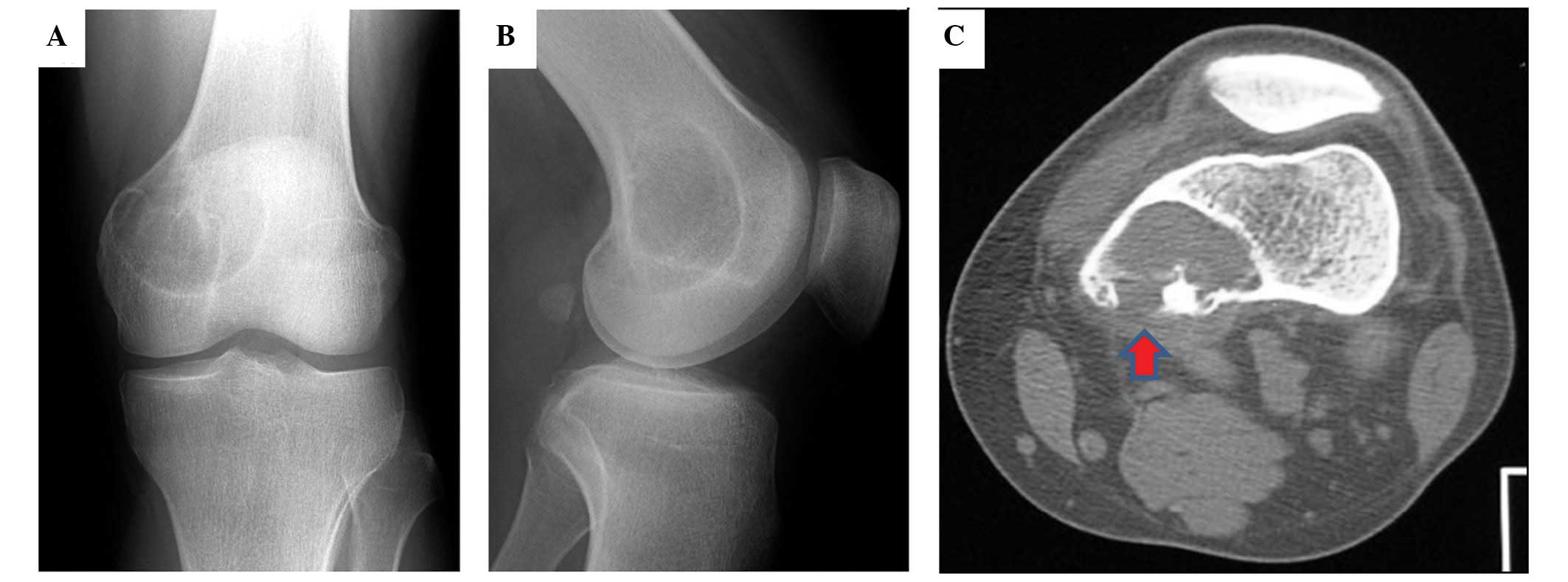
Results of a roentgenogram of the distal femur revealed an
eccentric osteolytic lesion in the medial condyle. The patient was
diagnosed with a benign bone tumor and was subsequently referred to
the Department of Orthopaedic Surgery, Graduate School of Medical
and Dental Sciences, Kagoshima University (Kagoshima, Japan) on May
21, 2001. During the first visit to our hospital, mild swelling
with tenderness in the distal part of the thigh was observed.
Results of laboratory examinations indicated that the white blood
cell count, C-reactive protein level and erythrocyte sedimentation
rate were normal. Physical examination revealed a normal range of
motion in the knee joint. Radiographs demonstrated an eccentric
osteolytic lesion with marginal sclerosis in the medial condyle. No
periosteal reaction was observed (Figs.
1A and B). Computed tomography revealed a distinct lesion (mass
size, 48×45×30 mm) and destruction of the posterior cortex
(Fig. 1C). An open biopsy of the
mass was performed and a pathological diagnosis indicated the
presence of a desmoplastic fibroma. The patient did not consent to
radical surgical treatment, such as en-bloc resection due to the
potential extensive functional loss following surgery. Therefore,
extended curettage with a high-speed burr, heat ablation with a
standard electrosurgical knife and artificial bone grafting, using
hydroxyapatite to fill the cavity, were performed. Macroscopic
observation of the specimen revealed a yellow-white mass with a
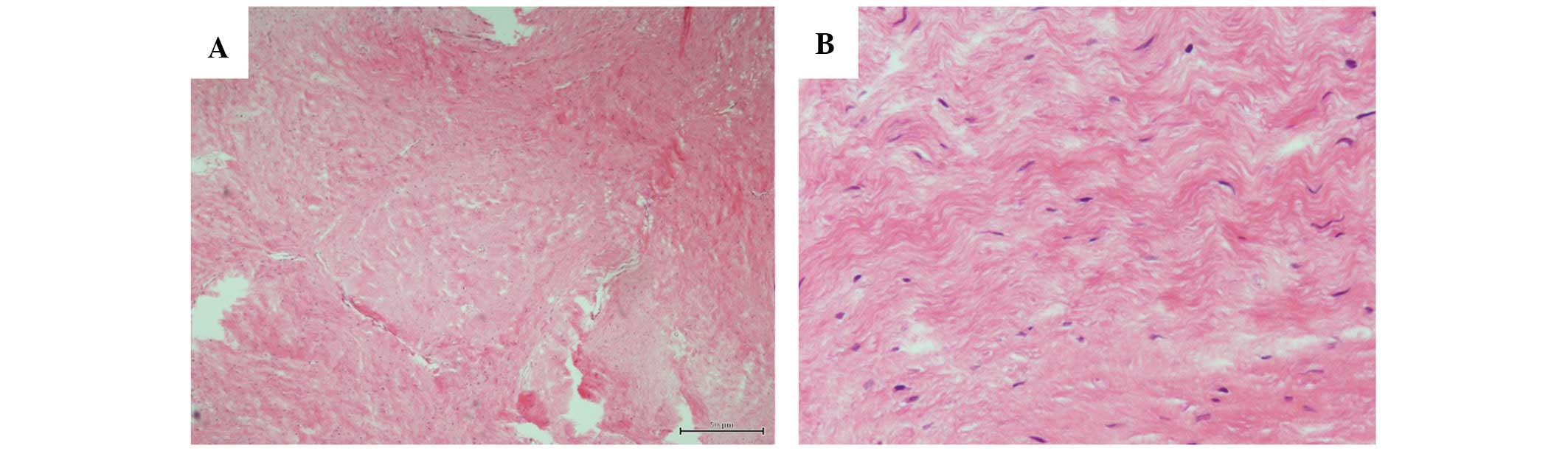
hard and rubber-like consistency. Histopathological analysis of the
resected specimen verified the diagnosis of desmoplastic fibroma,
which had been indicated by a previous biopsy (Fig. 2). The postoperative course was
uneventful and no recurrence or metastasis was observed during the
12-year follow-up period (Fig. 3A and
B). Currently, the patient’s functional outcome is excellent;
the range of motion in the knee joint is not limited and the
patient is able to sit on his heels with a straight back without
experiencing pain (Fig. 3C). The
patient is also able to run a complete marathon and, according to
the Musculoskeletal Tumor Society Staging system, achieved a score
of 100% (8).
Written informed consent was obtained from the
patient for publication of this case report and the accompanying
images.
Discussion
Desmoplastic fibroma of the bone is a benign,
non-metastatic, but locally aggressive tumor, which often occurs in
adolescents and young adults. Long bones are the most common sites
of occurrence with mandible, femur, pelvic, radial and tibial
involvement in 23, 15, 13, 12 and 9% of cases, respectively
(3). Therefore, when the disease
involves the long bones in young patients, surgery is required to
achieve good long-term functional outcomes without local recurrence
following treatment. However, surgical experience is limited owing
to the rarity of the disease; desmoplastic fibroma only accounts
for ~0.1% of all primary bone tumors (9). As a result, surgical management of
this rare condition remains controversial.
The primary surgical procedures for the treatment of
desmoplastic fibroma include curettage, marginal or wide resection,
cryosurgery and amputation (3).
Böhm et al (3) analyzed 191
cases of desmoplastic fibroma of the bone and reported that
recurrence rates following curettage, excision and wide resection
were 55, 72 and 17%, respectively. Thus, it was concluded that the
recommended primary treatment for desmoplastic fibroma of the bone
is a marginal or wide resection of the tumors. Based on their
analysis, the majority of physicians currently advocate en-bloc
surgical excision with negative tumor margins. Several recent case
studies have demonstrated that the majority of surgeons selected
en-bloc or wide resection of tumors as the primary procedure when
the tumors were located in the ulna (4), femur (5), ilium (6), scapula (7) and calcaneus (10). Therefore, desmoplastic fibroma
tumors are predominantly treated with wide resection despite their
lack of metastatic potential.
Extended curettage has been widely described in
tumor surgery as a unique modality of surgical treatment for bone
tumors. One of the advantages of this technique is its minimally
invasive approach compared with conventional surgical procedures.
Intralesional curettage has been considered the preferred treatment
option for giant cell tumors (GCTs), another type of locally
aggressive benign bone tumor, rather than resection, as it
preserves the anatomy and function (11,12).
Similar to desmoplastic fibroma, GCT is also noted for its
potential to recur following curettage. Therefore, following
thorough intralesional curettage, various adjuvant therapeutic
procedures have been employed to enhance local control, such as
liquid nitrogen, heat ablation, phenol treatment and acrylic
cement. However, the effectiveness of such adjuvant therapeutic
procedures during curettage remains unclear in cases of
desmoplastic fibroma. In a study that included 191 cases (3), a high recurrence rate (55%) of
desmoplastic fibroma was observed in patients who underwent
curettage, however, it was not observed in those who underwent
curettage with adjuvant therapy. According to their analysis, only
four patients underwent curettage with adjuvant therapy and the
recurrence rate in these patients was 25%, which was markedly lower
compared with that in those who underwent curettage alone.
Recently, although certain reports have described
the successful treatment of desmoplastic fibroma using curettage
with lesion ablation (12), the
follow-up duration in these studies was insufficient. Rastogi et
al (10) proposed that when a
resection causes major functional loss, an attempt at intralesional
curettage is justified. In the present case, the patient was a
young marathon runner and the lesion was located in the metaphysis
of the femur. Therefore, heat ablation was selected as the adjuvant
therapeutic procedure following thorough intralesional curettage in
order to preserve good function of the knee and prevent local
recurrence. While tumor resection is currently the preferred
modality of treatment for desmoplastic fibroma, curettage with heat
ablation has proved to be an acceptable alternative. Additional
studies are required to investigate the effectiveness of adjuvant
therapeutic procedures during surgery for the treatment of
desmoplastic fibroma.
Furthermore, diagnosis of this rare disease is
challenging and often inaccurate. Low-grade fibrosarcoma is often
the most difficult differential diagnosis (14). Compared with desmoplastic fibroma, a
typical fibrosarcoma is increasingly cellular with a herringbone
pattern, which exhibits increased polymorphisms and higher mitotic
activity (2). However, mitosis is
not a prominent feature in low-grade bone fibrosarcoma (2). Therefore, in such cases, the
diagnostic process is challenging and a final confirmation is often
determined only after follow-up visits. In these instances,
resection with negative margins is required to treat the tumor,
rather than curettage.
In conclusion, the current report presents the rare
case of a patient with desmoplastic fibroma of the distal femur who
was successfully treated with extended curettage, heat ablation and
artificial bone grafting. To preserve good, long-term function,
extended curettage with heat ablation may be the preferred
treatment for this benign lesion in the femur, rather than
resection, owing to the lack of metastatic potential of the
tumor.
References
|
1
|
Fletcher CDM, Unni KK and Mertens F: World
Health Organization Classification of Tumours. Pathology and
genetics of tumours of soft tissue and bone. IARC Press; Lyon: pp.
2882002
|
|
2
|
Jaffe HL: Desmoplastic fibroma and
fibrosarcoma. Tumors and Tumorous Conditions of the Bones and
Joints. Lea and Febiger; Philadelphia, PA: pp. 298–303. 1958
|
|
3
|
Böhm P, Kröber S, Greschniok A, Laniado M
and Kaiserling E: Desmoplastic fibroma of the bone. A report of two
patients, review of the literature, and therapeutic implications.
Cancer. 78:1011–1023. 1996.
|
|
4
|
Goyal T, Rastogi S and Tripathy SK:
Desmoplastic fibroma of ulna: Excision and reconstruction of
olecranon with a fibular graft. Indian J Orthop. 47:207–210.
2013.
|
|
5
|
Gao S, Cai Q, Yao W, Wang J, Zhang P and
Wang X: Desmoplastic (collagenous) fibroma of the femur: A case
report and review of the literature. Oncol Lett. 6:1285–1288.
2013.
|
|
6
|
Rouchy RC, Courvoisier A, Wimsey S,
Bourgeois E, Burroni B and Griffet J: Desmoplastic fibroma of the
ilium. Int J Surg Case Rep. 4:875–878. 2013.
|
|
7
|
Okubo T, Saito T, Takagi T, Torigoe T,
Suehara Y, Akaike K, Yao T and Kaneko K: Desmoplastic fibroma of
the scapula with fluorodeoxyglucose uptake on positron emission
tomography: a case report and literature review. Int J Clin Exp
Pathol. 6:2230–2236. 2013.
|
|
8
|
Enneking WF, Dunham W, Gebhardt MC,
Malawar M and Pritchard DJ: A system for the functional evaluation
of reconstructive procedures after surgical treatment of tumors of
the musculoskeletal system. Clin Orthop Relat Res. 286:241–246.
1993.
|
|
9
|
Dahlin DC and Unni KK: Fibrosarcoma and
desmoplastic fibroma. Bone Tumors. 4th edition. Thomas;
Springfield, IL: pp. 375–378. 1986
|
|
10
|
Rastogi S, Varshney MK, Trikha V, Khan SA
and Mittal R: Desmoplastic fibroma: a report of three cases at
unusual locations. Joint Bone Spine. 75:222–225. 2008.
|
|
11
|
Campanacci M, Baldini N, Boriani S and
Sudanese A: Giant-cell tumor of bone. J Bone Joint Surg Am.
69:106–114. 1987.
|
|
12
|
AlSulaimani SA and Turcotte RE; Canadian
Orthopaedic Oncology Society (CANOOS) collaborators. Iterative
curettage is associated with local control in giant cell tumors
involving the distal tibia. Clin Orthop Relat Res. 471:2668–2674.
2013.
|
|
13
|
Koba T, Susa M, Nakayama R, Watanabe I,
Horiuchi K, Mukai M, Yabe H, Toyama Y and Morioka H: Desmoplastic
fibroma arising in the distal phalanx of the great toe: a case
report. J Foot Ankle Surg. 53:71–74. 2014.
|
|
14
|
Callahan KS, Eberhardt SC, Fechner RE and
Cerilli LA: Desmoplastic fibroma of bone with extensive
cartilaginous metaplasia. Ann Diagn Pathol. 10:343–346. 2006.
|