Introduction
The most frequent sites of breast cancer metastasis
are the local and distant lymph nodes, brain, lung, liver and bone,
with metastasis to the stomach being relatively rare. The reported
incidence of gastric metastasis in breast cancer patients varies
between 2.8 and 27% (1,2). The most common sites of gastric
metastasis in breast cancer are the fundus (43%), antrum (43%) or
both (14%). In addition, the majority of gastric metastasis are
positive for hormonal receptors (79%) (3). Among the various types of breast
cancer, those with a lobular pathology have a higher tendency to
metastasize to the stomach (4).
Differentiating between primary gastric cancer and breast cancer
metastasis to the stomach is important for the planning of
treatment. The diagnosis is established by histological,
gastroscopy and immunohistochemical analysis, but it may be
difficult to differentiate primary gastric cancer from gastric
metastasis in breast cancer patients. The present study describes a
case of breast cancer metastasis to the stomach that was detected
using gastroscopy and immunohistochemical analysis. During the
treatment, the multiple apophysis lesions in the gastric body were
observed to significantly narrow and the symptoms of abdominal
discomfort were also alleviated. Patient provided written informed
consent.
Case report
Patient presentation
A 53-year-old female presented to the Department of
General Surgeryof the General Hospital of Shenyang Military Area
Command (Shenyang, China) seeking treatment for epigastric
discomfort from sour regurgitation and belching that had persisted
for one month. The patient had no history of bleeding, tarry stools
or associated hemorrhage symptoms. The patient had previously
undergone a modified radical mastectomy for an invasive lobular
carcinoma (ILC) of the left breast in September 2004.
Immunohistochemistry (IHC) revealed that three axillary lymph nodes
were involved and that the tissue samples were positive for
estrogen receptors (ERs) and progesterone receptors (PRs). Six
cycles of paclitaxel (240 mg) were administrated followed by the
oral administration of tamoxifen (10 mg) twice daily for five
years.
Diagnosis
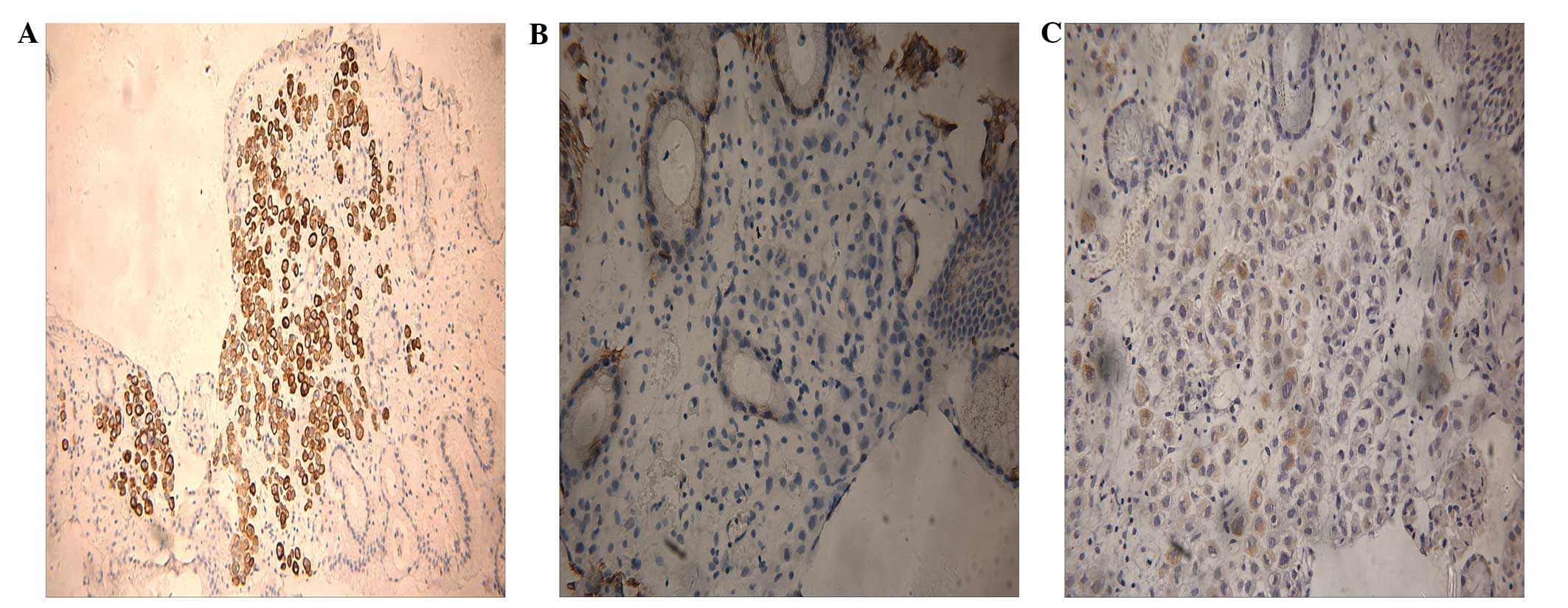
Gastroscopy revealed multiple apophysis lesions in
the body of the stomach (Fig. 1A),
which were diagnosed as metastatic tumors of the stomach. Multiple
endoscopic biopsies were performed. Few disseminated mild atypia
cells were identified in the lamina propria mucosa using
hematoxylin and eosin (H&E) staining. Moreover, IHC was
performed and showed the tissues to be cytokeratin (CK)
7+, CK20− and gross cystic disease fluid
protein (GCDFP)-15+ (Fig.
2). Based on the medical history of the patient and the
findings of IHC and gastroscopy, the patient was diagnosed with
breast cancer metastasis to the stomach.
Treatment
Six cycles of rescue chemotherapy with docetaxel
(120 mg) combined with capecitabine (1.5 g orally twice a day) were
administered. During the treatment, two gastroscopy procedures
revealed that the multiple apophysis lesions in the gastric body
were significantly narrowed (Fig. 1B
and C). The symptoms of abdominal discomfort were also
alleviated. Single drug chemotherapy using capecitabine (1.5 g
orally twice a day) was then administered. The patient is currently
undergoing follow-up treatment, while continuing capecitabine
chemotherapy.
Discussion
ILC was first described in 1941 by Foote and Stewart
(5). ILC accounts for 6–14% of all
breast cancer cases and has a distinctive biological behavior
(4–7). ILC derives from breast acinar
epithelial cells and is the second most common type of breast
cancer. Compared with infiltrating ductal carcinoma (IDC), ILC is
most likely to occur in older, postmenopausal females with large,
well-differentiated, ER-positive tumors and less vessel invasion
(5,6,8).
Pestalozzi et al (6)
reported that patients with ILC exhibited a significant early
advantage with respect to disease-free survival and overall
survival, and that patients with IDC exhibited a significant late
advantage after 6 and 10 years, respectively. It was found that the
most common sites of breast cancer metastasis were the local and
distant lymph nodes, brain, lung, liver and bone, while metastasis
to the stomach was relatively rare (6). Previous studies have reported that,
unlike IDC, ILC has a higher tendency to metastasize to the
stomach, ovaries, meninges, pleura, skin, peritoneum, duodenum and
colon (1,3,9,10).
This may be associated with the presence of discohesive small
cells, a phenotypic trait that characterizes ILC. The loss of
E-cadherin, which is observed in the majority of ILC cases, may
lead to changes in cell-cell adhesion and preferential growth at
sites of metastasis (8).
The metastasis of primary breast cancer to the
stomach is particularly uncommon at the time of the initial
diagnosis (3,11). Symptoms of gastric metastasis are
often non-specific and include epigastric pain, anorexia, non-fatal
hemorrhage, vomiting and dysphagia (2,12).
Substantial variability is shown by the endoscopic findings,
including the observation of lesions with a benign appearance or
primary gastric cancer (3,10,13)
with diffusely infiltrative lesions (2). Gastric metastases are usually
recognized as a diffuse infiltration by endoscopy (2). Endoscopic biopsies histologically
confirm ~90% of gastric metastatic lesions (12). Immunohistochemical analyses are
recommended for the accurate diagnosis of breast cancer metastasis
to the stomach. ER and PR expression are not observed in gastric
cancer and are useful for diagnosing breast cancer metastases to
the stomach (14). However, if the
primary lesion is negative for ER and PR, these markers are not
useful for diagnosing breast cancer metastases in the stomach
(15). Immunostaining of CK20 and
CK7 also aids in the formation of a diagnosis (15). The immunoperoxidase technique has
revealed that the negative expression of GCDFP-15 is found in
benign and malignant lesions of the stomach. Thus GCDFP-15 has been
proposed to be a specific tissue marker of apocrine epithelium and
breast carcinomas with apocrine features (16). Although certain methods are used to
diagnose gastric metastases, the diagnosis is difficult. The
identification of gastric metastases using endoscopy is also hard.
Furthermore, false-negative IHC results are common, as the tumor
cells are scattered and located in deep mucosal tissue following
pathological biopsy (2,3,10,12,13).
In the present study, the endoscopic findings of the patient showed
typical metastases with diffuse intramural infiltration to the
stomach.
The treatment recommendation for gastric metastases
from breast cancer is typically a systemic treatment. Surgical
intervention should be reserved for palliation or certain cases of
solitary resectable gastrointestinal tract metastases (17).
The patient discussed in the present study was
treated with docetaxel combined with capecitabine, and following
six cycles of rescue chemotherapy, gastroscopy revealed that this
treatment had induced a marked result. The patient also experienced
partial remission of the abdominal discomfort and an overall
improvement in the quality of life.
The present case represents a typical metastatic
tumor to the stomach, which was detected using gastroscopy eight
years after the surgical removal of ILC. It is essential to use
GCDFP-15 and CK7/20 immunostaining of the biopsy tissue in order to
identify breast cancer metastases in the stomach.
When a patient has a history of ILC, endoscopic
examinations should be performed carefully. Moreover, physicians
should provide the clinical history of the patient to the
endoscopist and the endoscopist should provide sufficient
information to the pathologist in order to obtain an accurate
diagnosis of breast cancer metastasis to the stomach and improve
the patient’s quality of life.
References
|
1
|
Ferlicot S, Vincent-Salomon A, Médioni J,
et al: Wide metastatic spreading in infiltrating lobular carcinoma
of the breast. Eur J Cancer. 40:336–341. 2004.
|
|
2
|
Taal BG, Peterse H and Boot H: Clinical
presentation, endoscopic features, and treatment of gastric
metastases from breast carcinoma. Cancer. 89:2214–2221. 2000.
|
|
3
|
Almubarak MM, Laé M, Cacheux W, et al:
Gastric metastasis of breast cancer: a single centre retrospective
study. Dig Liver Dis. 43:823–827. 2011.
|
|
4
|
Arpino G, Bardou VJ, Clark GM and Elledge
RM: Infiltrating lobular carcinoma of the breast: tumor
characteristics and clinical outcome. Breast Cancer Res.
6:R149–R156. 2004.
|
|
5
|
Foote FW and Stewart FW: Lobular carcinoma
in situ: A rare form of mammary cancer. Am J Pathol. 17:491–496.
1941.
|
|
6
|
Pestalozzi BC, Zahrieh D, Mallon E, et al:
Distinct clinical and prognostic features of infiltrating lobular
carcinoma of the breast: combined results of 15 international
Breast Cancer Study Group clinical trials. J Clin Oncol.
26:3006–3014. 2008.
|
|
7
|
Martinez V and Azzopardi JG: Invasive
lobular carcinoma of the breast: incidence and variants.
Histopathology. 3:467–488. 1979.
|
|
8
|
Cristofanilli M, Gonzalez-Angulo A, Sneige
N, et al: Invasive lobular carcinoma classic type: response to
primary chemotherapy and survival outcomes. J Clin Oncol. 23:41–48.
2005.
|
|
9
|
Abid A, Moffa C and Monga DK: Breast
cancer metastasis to the GI tract may mimic primary gastric cancer.
J Clin Oncol. 31:e106–e107. 2013.
|
|
10
|
Malhotra A, Guturu P, Basim MS and Raju
GS: A rare case of breast cancer metastasis presenting as linitis
plastica of the stomach and colon (with videos). Gastrointest
Endosc. 70:552–553. 2009.
|
|
11
|
Tremblay F, Jamison B and Meterissian S:
Breast cancer masquerading as a primary gastric carcinoma. J
Gastrointest Surg. 6:614–616. 2002.
|
|
12
|
De Palma GD, Masone S, Rega M, et al:
Metastatic tumors to the stomach: clinical and endoscopic features.
World J Gastroenterol. 12:7326–7328. 2006.
|
|
13
|
Dumoulin FL and Sen Gupta R: Breast cancer
metastasis to the stomach resembling small benign gastric polyps.
Gastrointest Endosc. 69:174–175. 2009.
|
|
14
|
van Velthuysen ML, Taal BG, van der Hoeven
JJ and Peterse JL: Expression of oestrogen receptor and loss of
E-cadherin are diagnostic for gastric metastasis of breast
carcinoma. Histopathology. 46:153–157. 2005.
|
|
15
|
Tot T: Cytokeratins 20 and 7 as
biomarkers: usefulness in discriminating primary from metastatic
adenocarcinoma. Eur J Cancer. 38:758–763. 2002.
|
|
16
|
Wick MR, Lillemoe TJ, Copland GT, Swanson
PE, Manivel JC and Kiang DT: Gross cystic disease fluid protein-15
as a marker for breast cancer: Immunohistochemical analysis of 690
human neoplasms and comparison with alpha-lactalbumin. Hum Pathol.
20:281–287. 1989.
|
|
17
|
Pectasides D, Psyrri A, Pliarchopoulou K,
et al: Gastric metastases originating from breast cancer: report of
8 cases and review of the literature. Anticancer Res. 29:4759–4763.
2009.
|