Introduction
Gastrointestinal stromal tumors (GISTs) are a common
mesenchymal tumor of the gastrointestinal tract. GISTs were
mistaken for leiomyosarcoma and other mesenchymal sarcomas prior to
1983 and have an incidence of ~1–2/100,000 worldwide (1–4). The
majority of GISTs are located in the stomach and small intestine,
while ~5% of the cases reported are located in the colon and rectum
(5).
Previously, the synchronous occurrence of GISTs and
other primary gastrointestinal malignancies has been reported in
the literature (6–7). However, to the best of our knowledge,
there are few studies regarding either synchronous or metachronous
GISTs (particularly multiple GISTs), as well as adenocarcinoma of
the colon and rectum. In the current report, we present the case of
a patient who exhibited metachronous multiple colonic GISTs as well
as adenocarcinoma of the colon.
Case report
In June 2008, an 80-year-old male patient was
admitted to the Department of Colorectal Surgery at The Liaoning
Provincial Tumor Hospital (Shenyang, China) complaining of anemia
and increasing paroxysmal abdominal pain during the previous month
prior to admission. The patient’s medical history was unremarkable.
On physical examination, the patient’s abdomen was flat and soft
without tenderness and no mass was palpated. A blood count test
revealed anemia, while the levels of carcinoembryonic antigen (CEA)
and carbohydrate antigen (CA)19-9 were 14.14 ng/ml and 28.9 U/l,
respectively. The chest X-ray was unremarkable and an abdominal
computed tomography (CT)-scan, conducted to establish the tumor
staging, demonstrated that there were no sites of distant
metastasis. A fiberoptic colonoscopy showed an irregular bulging
mass in the ascending colon, which occupied half of the intestinal
lumen, however, no other abnormalities were detected in the
remaining regions of the colon and rectum. Histological examination
of the biopsy specimen revealed a well-differentiated
adenocarcinoma.
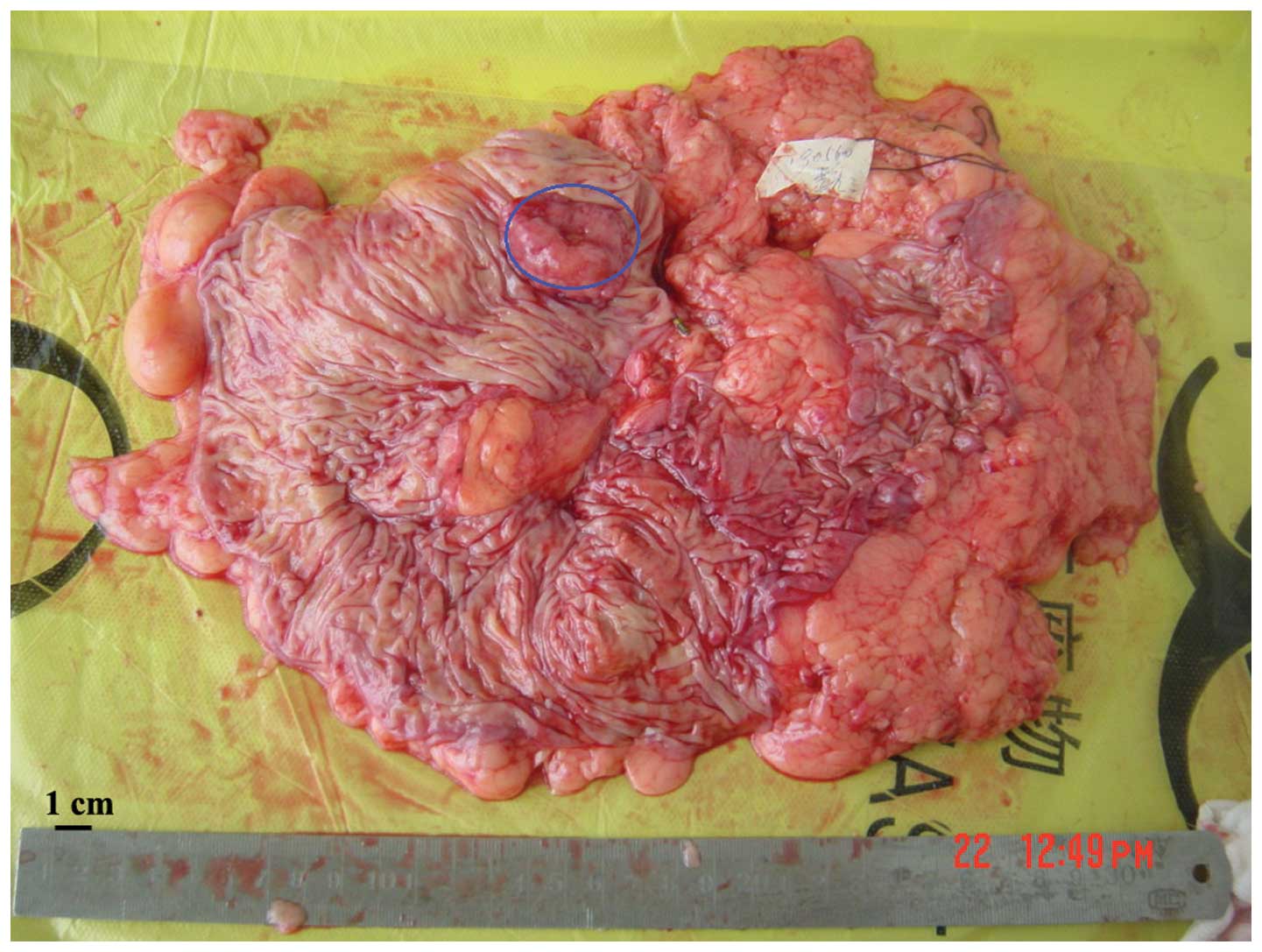
A laparoscopy assisted right hemicolectomy was
subsequently performed. During surgery, a tumor mass, measuring 3×2
cm, which was invading the serous membrane was detected in the
ascending colon; there was no evidence of lymph node metastasis
(Fig. 1). Histological examination
of the whole resected specimen demonstrated the combined presence
of a moderately differentiated adenocarcinoma and a mucinous
adenocarcinoma, which were located at the ascending colon and
invading the subserous layer of the colon (Fig. 2). None of the 16 resected lymph
nodes contained metastasis. According to the seventh edition of the
tumor, node, metastasis (TNM) staging classification (2009) of
colorectal cancer from the American Joint Committee on Cancer, the
pathological stage of the tumor was determined to be T3N0M0.
Following surgery, the patient received oral capecitabine
(Xeloda®; F. Hoffmann-La Roche, Basel, Switzerland) as
adjuvant chemotherapy at a dose of 1,250 mg/m2 twice
daily, administered on days 1–14 every 21 days over 24 weeks.
A regular follow-up regime included a complete
physical examination, basic serum chemistry, a chest X-ray, an
abdominal ultrasound or CT-scan, and assessments of CEA and CA19-9
levels; this regime was performed every three months for two years.
A fiberoptic colonoscopy was performed annually following
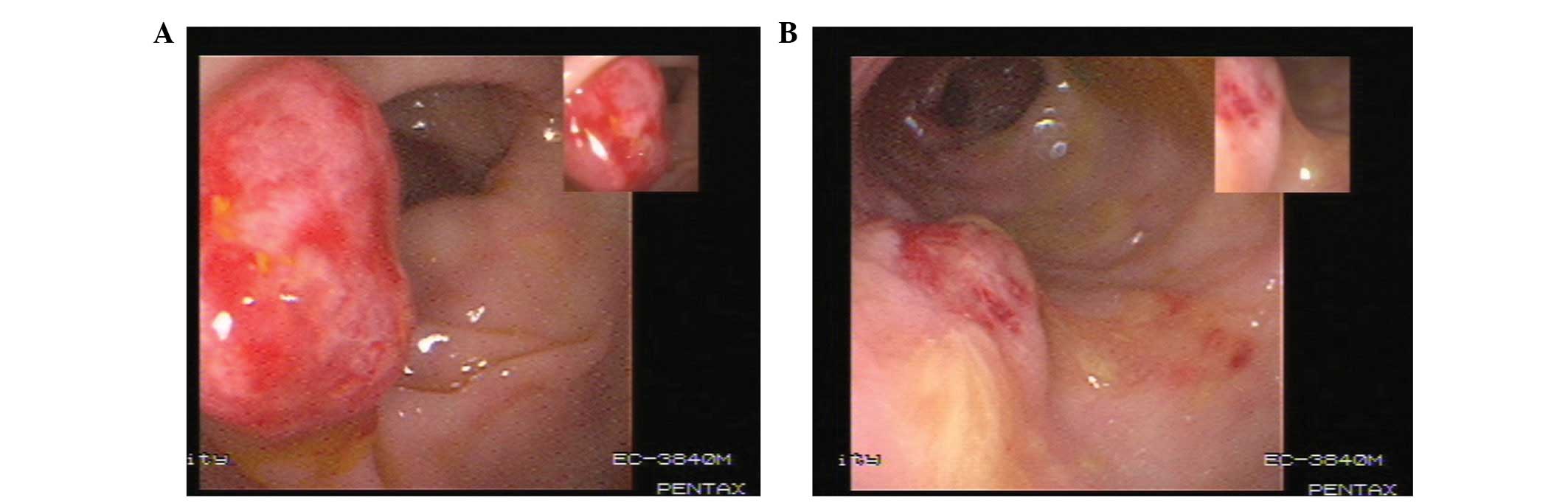
treatment. In April 2010, two disc-like bulging lesions were
identified in the descending colon and rectosigmoid during the
follow-up colonoscopy. This included one lesion, which was a
distance of 40 cm from the anus at the descending colon and
measured 1.5×1.5 cm. The other lesion was located at the
rectosigmoid and measured 1.2×1.2 cm (Fig. 3). An exploratory laparotomy followed
by a segmental bowel resection was performed. The two lesions
infiltrated the basement membrane and the submucosa. Pathological
examination revealed that the two colonic lesions were mesenchymal
cell tumors with mitotic activity, which were less than five
mitoses per 50 high-power fields. Immunohistochemistry of the
lesions were positive for cluster of differentiation (CD)117, CD34
and discovered on GIST-1 (Fig. 4).
Routine treatment was administered following the surgery and the
patient recovered well. Written informed consent was obtained from
the patient and the patient’s relatives for publication of this
case report.
Discussion
Previous studies have demonstrated that ~20% of
patients with GISTs develop other types of cancer, with the
predominant GIST-associated cancers being gastrointestinal (47%),
lymphoma/leukemia (7%), prostate (9%) and breast (7%) (6–7).
However, to the best of our knowledge, a coexistence of
metachronous multiple GISTs and colorectal carcinoma has not
previously been described. In the present case report, a patient
with multiple GISTs, which were identified during a routine
follow-up colonoscopy examination 21 months after a colectomy, is
presented.
Despite recent progress regarding the diagnosis and
treatment of GISTs, little is currently known concerning the rare
case of synchronous or metachronous GISTs along with tumors of
different histogenesis. The majority of previous case reports
describe small GISTs that were discovered during surgical
procedures for another primary malignancy (8). In the present case, two lesions could
have been incorrectly diagnosed as a reappearance of colon cancer,
as the second colonoscopy and biopsy prior to surgery were
indicative of a case of poorly differentiated adenocarcinoma;
furthermore, the patient had a history of cancer of the ascending
colon. Therefore, it is important to be aware that lesions, which
are discovered during a postoperative colonoscopy following
colorectal cancer surgery, may be another primary tumor of
different histopathology rather than a recurrence.
As a result of postoperative pathological
examination and immunohistochemical analysis of the relevant
factors, including CD117, the diagnosis was finally determined to
be colonic multiple GISTs. Based on the location, size and number
of mitotic figures, and according to the improved National
Institute of Health risk classification (9), the patient was considered to have a
low-grade tumor. Generally, GISTs are sporadic, however, they may
be detected as multiple lesions in familial forms and associated
with type 1 neurofibromatosis (10). Furthermore, the majority of small
GISTs are asymptomatic and, when they present alone, mimic other
neoplastic conditions, which complicates the diagnosis (11,12).
In the present case, the preoperative pathology was not consistent
with the postoperative pathology as the colonoscopic biopsy
obtained samples which were too small and the morphous was
different as it exhibited an increased number of intestinal
epithelial cells, which resulted in a diagnosis of poorly
differentiated or undifferentiated adenocarcinoma rather than
GISTs.
As the natural history of GISTs is unknown, the
method for the effective management of GISTs that are <2 cm in
size remains elusive. However, the present case indicates that a
resection may be essential for a colonic cancer patient, when the
endoscopic diagnosis of new lesions in the colon, during an
endoscopic follow-up, is complicated.
In conclusion, metachronous GISTs and adenocarcinoma
in the colon are rare. However, it is important to carefully
investigate and differentiate between potential lesions during a
routine postoperative colonoscopy following colorectal cancer
surgery, as the patient may present with rare GISTs, which may be
confused with the recurrence of colorectal cancer. In addition, a
surgical resection may be necessary, when the diagnosis of new
neoplastic lesions during the follow-up colonoscopy of a colonic
cancer patient is in doubt.
References
|
1
|
Mazur MT and Clark HB: Gastric stromal
tumors. Reappraisal of histogenesis. Am J Surg Pathol. 7:507–519.
1983.
|
|
2
|
Nilsson B, Bümming P, Meis-Kindblom JM,
Odén A, Dortok A, Gustavsson B, Sablinska K and Kindblom LG:
Gastrointestinal stromal tumors: the incidence, prevalence,
clinical course, and prognostication in the preimatinib mesylate
era - a population-based study in western Sweden. Cancer.
103:821–829. 2005.
|
|
3
|
Monges G, Bisot-Locard S, Blay JY, Bouvier
AM, Urbieta M, Coindre JM and Scoazec JY: The estimated incidence
of gastrointestinal stromal tumors in France. Results of PROGIST
study conducted among pathologists. Bull Cancer. 97:E16–E22.
2010.
|
|
4
|
Tran T, Davila JA and El-Serag HB: The
epidemiology of malignant gastrointestinal stromal tumors: an
analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol.
100:162–168. 2005.
|
|
5
|
Woodall CE III, Brock GN, Fan J, Byam JA,
Scoggins CR, McMasters KM and Martin RC II: An evaluation of 2537
gastrointestinal stromal tumors for a proposed clinical staging
system. Arch Surg. 144:670–678. 2009.
|
|
6
|
Pandurengan RK, Dumont AG, Araujo DM,
Ludwig JA, Ravi V, Patel S, Garber J, Benjamin RS, Strom SS and
Trent JC: Survival of patients with multiple primary malignancies:
a study of 783 patients with gastrointestinal stromal tumor. Ann
Oncol. 21:2107–2111. 2010.
|
|
7
|
Agaimy A, Wünsch PH, Sobin LH, Lasota J
and Miettinen M: Occurrence of other malignancies in patients with
gastrointestinal stromal tumors. Semin Diagn Pathol. 23:120–129.
2006.
|
|
8
|
Ferreira SS, Werutsky G, Toneto MG, Alves
JM, Piantá CD, Breunig RC, Brondani da Rocha A, Grivicich I and
Garicochea B: Synchronous gastrointestinal stromal tumors (GIST)
and other primary cancers: case series of a single institution
experience. Int J Surg. 8:314–317. 2010.
|
|
9
|
Joensuu H, Vehtari A, Riihimäki J, et al:
Risk of recurrence of gastrointestinal stromal tumour after
surgery: an analysis of pooled population-based cohorts. Lancet
Oncol. 13:265–274. 2012.
|
|
10
|
Miettinen M, Fetsch JF, Sobin LH and
Lasota J: Gastrointestinal stromal tumors in patients with
neurofibromatosis 1: a clinicopathologic and molecular genetic
study of 45 cases. Am J Surg Pathol. 30:90–96. 2006.
|
|
11
|
Lee YT, Chiu PW, Choi PC and Sung JJ:
Esophageal small-cell cancer mimicking stromal tumor. Endoscopy.
38(Suppl 2): E21–E22. 2006.
|
|
12
|
Troupis TG, Chatzikokolis S, Michalinos A,
Sarakinos A, Kotsopoulos P, Patsea H, Kotsinas A, Evangelou K and
Gorgoulis VG: GIST mimicking an hyperplastic polyp of descending
colon. Ann Ital Chir. 82:141–146. 2011.
|