Introduction
Dermatofibrosarcoma protuberans (DFSP) is an
uncommon, slow-growing, low-grade sarcoma of putative dermal
fibroblastic origin, all recurrence is in situ and rarely
metastasizes. The incidence rate is reported to be ~5 per 1 million
persons annually (1). Typically,
DFSP starts as a red or blue-red coloured nodules. Nodules may
gradually develop to become irregularly shaped swellings (2). The five-year survival rate can reach
88.9%. DFSP is relatively resistant to chemotherapy and
radiotherapy, thus surgery is the primary treatment for DFSP
(3). DFSP frequently involves the
trunk. While the head, neck and extremities are commonly involved
in DFSP, breast involvement is rare (4). Therefore, DFSP is often misdiagnosed
as a benign breast tumor, delaying treatment.
Case report
Patient presentation
A 26-year old woman underwent ablation of a left
breast lump, which was diagnosed as DFSP one year previously at
YueBei People’s Hospital, Shaoguan, China). Six months after
surgery, the patient noticed a lump gradually growing underneath
the scarred area of the surgical site of the left breast. Physical
examination revealed a brown-red, firm, fixed breast mass with an
ill-defined border and smooth margins. The patient had no history
of systemic disease or malignancy and the laboratory data were
normal.
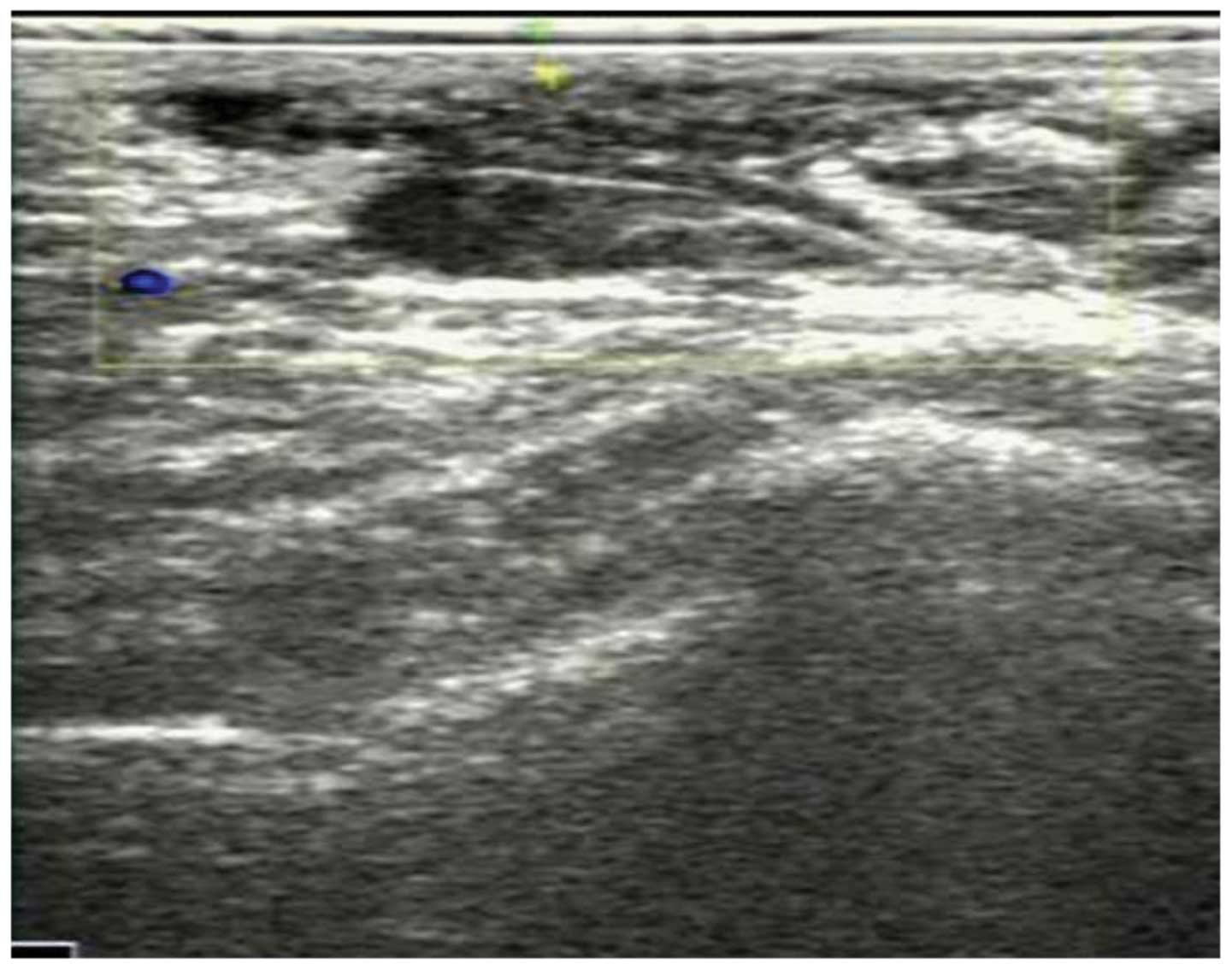
Ultrasound imaging
Targeted ultrasound of the left breast revealed a
32×9-mm hypoechoic mass lesion with an irregular border at the five
o’clock position, 2 mm deep in the skin and ~40 mm from the nipple.
No peripheral or internal blood flow was observed. Local invasion
of subcutaneous fat and skin was also detected. The mass was
classified as a Breast Imaging-Reporting and Data
System-ultrasonography 4 lesion (Fig.
1).
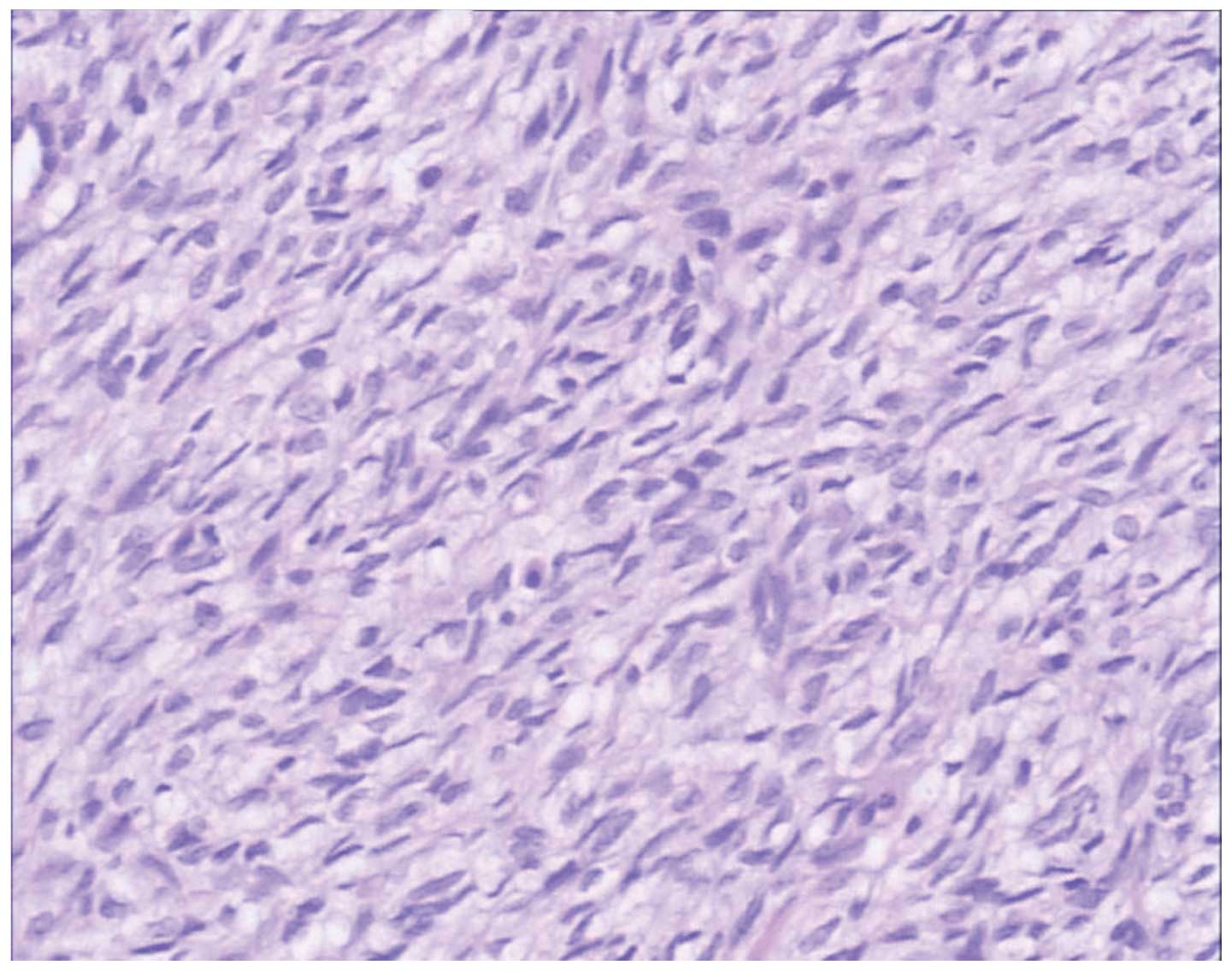
Surgery and follow-up
The mass was excised with 3-cm margins. The patient
underwent excisional breast biopsy following surgery. Pathological
analysis revealed that the mass consisted of spindle cells arranged
in storiform patterns and short fascicles (Fig. 2) that were cluster of
differentiation (CD) 34-positive (Fig.
3). The patient was followed-up for ~12 months and did not
exhibit any signs of recurrence.
Discussion
DFSP is a rare cutaneous malignancy that arises from
the dermis. The reported incidence of DFSP is approximately five
cases per one million individuals per year (5). DFSP was first described by Darier and
Ferrand (6) in 1924, and was termed
DFSP by Hoffmann (7) in 1925. While
DFSP is a low-grade sarcoma, it is capable of infiltration and
local recurrence following inadequate excision.
DFSP usually involves the trunk. DFSP is also often
reported in the limbs, head and neck; however, involvement of the
breast is rare, as described previously (8). Typically, DFSP develops as a deep-red
or blue-red plaque and grows slowly, usually reaching a size of ≥3
cm (2).
DFSP is a relatively rare cancer of the breast and
is difficult to diagnose. DFSP may be difficult to distinguish from
mammary fibroadenomas due to the lack of peripheral or internal
blood flow and the oval or spherical lump observed using B-mode
ultrasound. However, the high rate of local spreading and the
involved area of the dermis differentiate DFSP from other mammary
fibroadenomas (1,9).
Surgery is the preferred treatment option for DFSP.
Due to the high recurrence rate associated with DFSP, treatment
consists of radical excision, which involves either complete
surgical excision with wide margins (>3 cm) performed during
conventional surgery or Mohs micrographic surgery. Selective or
superselective lymphadenectomy is not important. As in the present
case, pathological analysis reveals spindle cells arranged in
storiform patterns and short fascicles (2,10) that
are CD34-positive (3,10,11).
Postoperative recurrence has been associated with the index of cell
division, cell structure, and incisal margin (12). In the present case, the patient was
advised to undergo a physical examination and breast B-mode
ultrasound examination twice a year in the first year, followed by
annual physical and B-mode ultrasound examinations.
Due to the rare involvement of the breast in cases
of DFSP, the present study reports this unique case with the
clinical features and B-mode ultrasound imaging findings.
Diagnostic imaging examinations are useful tools for pre-surgical
examination of breast DFSP, as well as for detecting its
post-surgical recurrence.
References
|
1
|
Chuang TY, Su WP and Muller SA: Incidence
of cutaneous T cell lymphoma and other rare skin cancers in a
defined population. J Am Acad Dermatol. 23:254–256. 1990.
|
|
2
|
Sin FN and Wong KW: Dermatofibrosarcoma
protuberans of the breast: a case report. Clin Imaging. 35:398–400.
2011.
|
|
3
|
Llombart B, Serra-Guillén C, Monteagudo C,
et al: Dermatofibrosarcoma protuberans: a comprehensive review and
update on diagnosis and management. Semin Diagn Pathol. 30:13–28.
2013.
|
|
4
|
Yeniay L, Unalp O, Sezak M and Yilmaz R:
Dermatofibrosarcoma protuberans of the breast. Breast J.
18:493–494. 2012.
|
|
5
|
Beaman FD, Kransdorf MJ, Andrews TR, et
al: Superficial soft-tissue masses: analysis, diagnosis, and
differential considerations. Radiographics. 27:509–523. 2007.
|
|
6
|
Darier S and Ferrand M: Recurrent or
progressive dermatofibromas and fibrosarcoma of the skin. Ann
Dermatol Venereol. 5:545–562. 1924.(In French).
|
|
7
|
Hoffman E: Regarding the knollentrichencle
fibrosarcoma of the skin (dermatofibrosarcoma protuberans).
Dermatol Z. 43:1–28. 1925.(In German).
|
|
8
|
Lin JY, Sheen-Chen SM, Hsu W, et al:
Dermatofibrosarcoma protuberans of the breast. Tumori. 94:861–863.
2008.
|
|
9
|
Liu SZ, Ho TL, Hsu SM, et al: Imaging of
dermatofibrosarcoma protuberans of breast. Breast J. 16:541–543.
2010.
|
|
10
|
Stivala A, Lombardo GA, Pompili G, et al:
Dermatofibrosarcoma protuberans: Our experience of 59 cases. Oncol
Lett. 4:1047–1055. 2012.
|
|
11
|
Foroozan M, Sei JF, Amini M, et al:
Efficacy of Mohs micrographic surgery for the treatment of
dermatofibrosarcoma protuberans: systematic review. Arch Dermatol.
148:1055–1063. 2012.
|
|
12
|
Makkar M, Singh DP, Rana A and Madan M:
Recurrent dermatofibrosarcoma protuberans: A continuing problem.
Indian Dermatol Online J. 4:68–69. 2013.
|