Introduction
Neurilemmoma, also known as schwannoma, is an
uncommon benign neoplasm originating from the Schwann cells in the
peripheral nerve sheaths (1,2). The
majority of the tumors commonly localize in the trunk, head and
extremities (3). However,
occurrence in the anterior abdominal wall is extremely rare. The
present study reports the case of a 67-year-old female with a
schwannoma of low malignant potential in the right anterior
abdominal wall and analyzes the main ultrasound and computed
tomography (CT) imaging observations. This study highlights the
clinical features and imaging findings of schwannoma in the
abdominal wall, and may aid in the future diagnosis and
differential diagnosis of this condition. Patient provided written
informed consent.
Case report
Patient and clinical data
A 67-year-old female was admitted to the Affiliated
Hospital of Nanjing University of Traditional Chinese Medicine
(Nanjing, China) complaining of a disconcerting mass in the right
anterior abdominal wall. A small mass had incidentally been found
10 years ago, with no restriction of movement present in the right
abdominal wall. As the patient did not exhibit any evident
uncomfortable symptoms, not enough attention was drawn to the
lesion. Over the year prior to the present hospital admittance, the
lump gradually increased in size and the patient felt soreness and
suffered untimely gas pains. To acquire a diagnosis and treatment,
the patient was referred to the outpatient clinic of the the
Affiliated Hospital of Nanjing University of Traditional Chinese
Medicine. There was no history of anergy, fever, anorexia, weight
loss, trauma or surgery, and there was no family history of a
similar complaint.
A physical examination showed a 6×4-cm mass
protruding through the right anterior abdominal wall. The mass was
firm, non-tender and not fixed to the skin of the abdominal wall.
All routine laboratory tests were within the normal ranges.
Ultrasound and CT imaging findings
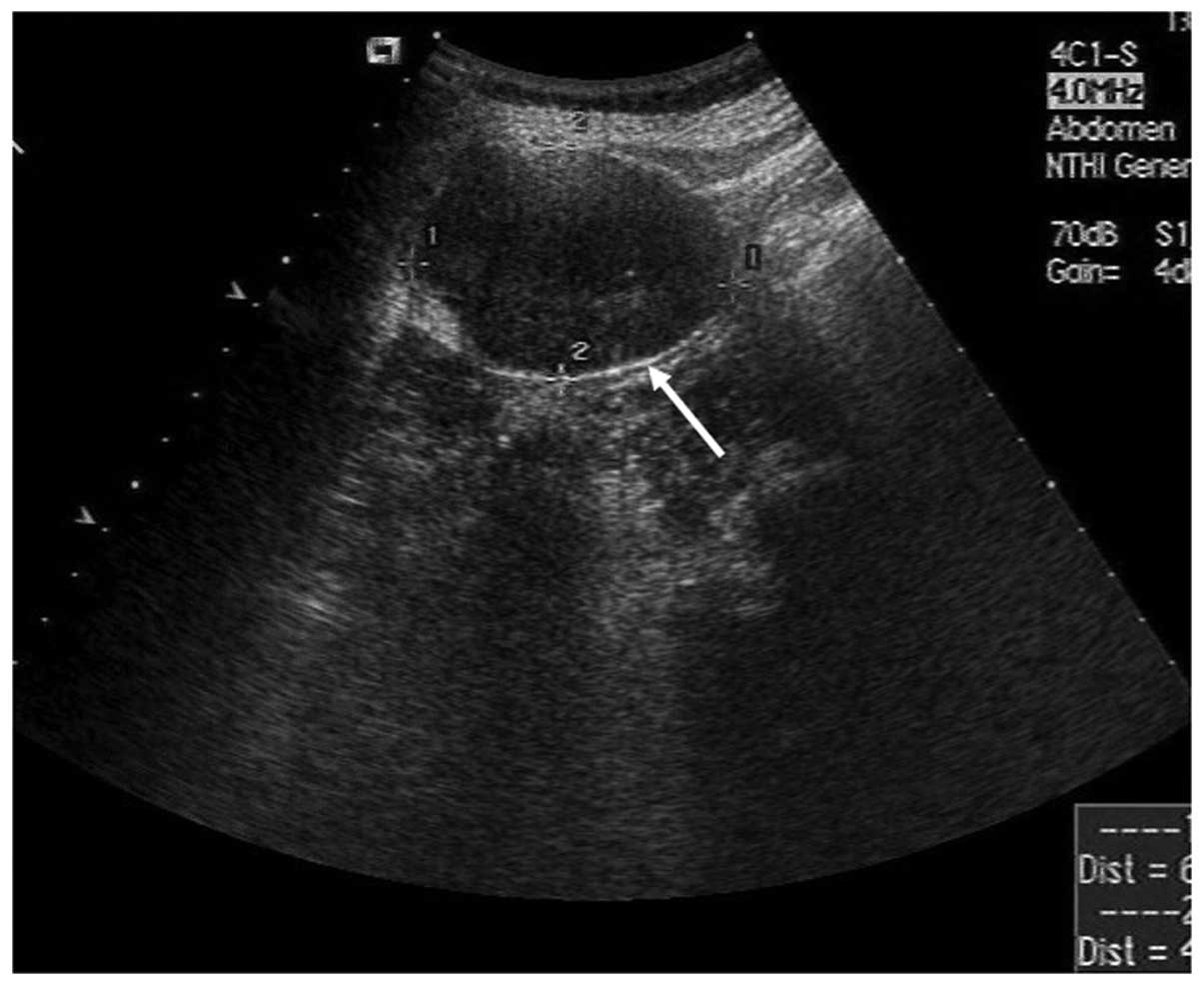
An abdominal ultrasound examination showed a
well-defined, elliptic, low echo level, heterogeneous mass just
beneath the abdominal skin (Fig.
1). The diameter of the tumor was 5.6 cm. A CT scan without
contrast enhancement revealed a solid, homogeneous mass with a low
density relative to the muscle in the abdominal wall (Fig. 2A). Contrast-enhanced scans showed a
evident gradually- and heterogeneously-enhanced lesion during the
arterial (Fig. 2B) and venous
(Fig. 2C) phases. Centripetal
fill-in was demonstrated and the mass was markedly,
homogenously-enhanced relative to the muscles (Fig. 2D and E) during the balanced and
delayed phases. The coronal CT image also clearly showed that the
mass was localized in the abdominal wall (Fig. 2F). The tumor showed marked
enhancement on contrast-enhanced CT. The time-intensity curve
following contrast agent injection is shown in Fig. 2G. Peak enhancement was observed
during the venous phase (120 sec after contrast agent injection)
and then slowly declined. However, the mass was hyperattenuated
during the delayed phase (360 sec after contrast agent injection).
No cysts, calcification or necrosis were found in the patient even
though the mass was large. A radiological diagnosis of a
paraganglioma or a vascular genesis tumor was considered.
Surgery and histopathological
examination
The lesion was completely excised and a frozen
section of the specimen was sent for histological examination.
Histological examination (Fig. 3A)
showed that the tumor was composed of abundant spindle-shaped
cells, which locally invaded the surrounding fat tissues.
Karyokinesis of the tumor cells could occasionally be observed. A
primary diagnosis of a spindle cell tumor and neurofibroma was
made. Immunohistochemical examination showed that the specimen was
negative for S-100 (Fig. 3B). Based
on the imaging findings and histopathological results, a final
diagnosis of a schwannoma of low malignant potential was made. The
patient was discharged 10 days after the surgery and no further
treatment was required. No evidence of recurrence was found during
the 3-month follow-up.
Discussion
Schwannomas or neurilemmomas are benign,
encapsulated, slow-growing mesenchymal neoplasms that arise from
Schwann cells and have a low malignant potential. These neoplasms
can present at any age, and most commonly occur in adult females
between the ages of 20 and 50 years old. Up to 20% of cases are
associated with neurofibromatosis type 1 (4). Although sporadic cases of these tumors
arising in the retroperitoneum, pelvis, perineum, adrenals, kidneys
and inguen have been previously reported (1), their occurrence in the abdominal wall
is extremely rare and only a few of these cases have been reported
(1,4–6).
The majority of schwannomas arise from the nerve
sheath of large peripheral nerves, occurring at the level of or
below the subcutaneous fat layer (7). Thus, the clinical signs and symptoms
may vary according to the tumor location. The tumors may be
asymptomatic and only found incidentally during examination.
However, when they grow larger, they can put pressure on the
surrounding large nerves (1), as
found in the patient of the present study.
Radiological examinations, CT or magnetic resonance
imaging (MRI) can provide important information about these tumors,
including the tumor site, its characteristics and its associations
with other tissues. The imaging features of schwannomas are
associated with its two components: Antoni type A (cellular
component) and Antoni type B (myxoid component). The former
consists of spindle-shaped cells that are arranged compactly in
interlacing fascicles or short bundles. Antoni B schwannomas are
loosely composed of reticular fibers, cysts, vascellum and the
Schwann cells (8). Accordingly,
schwannomas usually present as a well-defined, homogeneous
soft-tissue mass on conventional CT scan (9,10). The
tumors show minimal or mild heterogeneous enhancement following the
injection of contrast agent (9,10). In
the present case, marked peripheral enhancement was demonstrated
during the artery and venous phases. The progressive centripetal
fill-in was then observed, and homogeneous enhancement occurred in
the lag period. The CT imaging observations of the schwannoma in
this study were similar with that of a hemangioma. In general,
schwannomas appear as hypointense on T1-weighted and hyperintense
on T2-weighted MRI. The hypercellular (Antoni A) and hypocellular
(Antoni B) components display hypointense and hyperintense signals,
respectively, on T2-weighted images (4,9). With
gadolinium administration, the enhancement portion corresponds to
the solid component of the Antoni A. Loose cellularity with diffuse
edematous change may result in minimal contrast enhancement. If
there is degenerative change of the neurilemmoma, it often shows a
poor blood supply, cyst formation, calcifications, hemorrhage and
hyalinization (11). In the present
case, no cyst formation, calcification or necrosis was
observed.
Although MRI and CT are ideally suited to detect the
tumor pathology and delineate the soft tissue and its components,
the final diagnosis can only be confirmed by histopathological
examination. Immunohistochemical examinations besides hematoxylin
and eosin staining are required to form a differential diagnosis
(12). Although a previous study
has shown that the diffuse immunoreactivity for S-100 is almost
universal in schwannomas (13),
another study showed that 10–50% of cases were negative (5). In the present case, the schwannoma was
also negative for S-100.
The ideal treatment for schwannoma is complete
surgical excision, and the prognosis is good (11), although recurrence of schwannomas
in situ or at a distant site, attributed to incomplete
resection, has also been reported (2). The present patient recovered well and
no evidence of recurrence was found on CT images during the 3-month
follow-up.
In conclusion, the present study indicates that a
diagnosis of schwannoma should be considered for certain patients
with masses in the abdominal wall. The observations of gradual and
heterogeneous enhancement during the artery and venous phases,
progressive centripetal fill-in and homogeneous enhancement during
the delayed phase may be useful information for the imaging
diagnosis of schwannomas.
References
|
1
|
Bhatia RK, Banerjea A, Ram M and Lovett
BE: Benign ancient schwannoma of the abdominal wall: an unwanted
birthday present. BMC Surg. 10:12010.
|
|
2
|
Forthman CL and Blazar PE: Nerve tumors of
the hand and upper extremity. Hand Clin. 20:233–242. 2004.
|
|
3
|
Canda MŞ: Peripheral nerve sheath tumors.
Türkiye Ekopatoloji Dergisi. 10:65–74. 2004.(In Turkish).
|
|
4
|
Mishra A, Hamadto M, Azzabi M and Elfagieh
M: Abdominal wall schwannoma: case report and review of the
literature. Case Rep Radiol. 2013:4568632013.
|
|
5
|
Khorgami Z, Nasiri S, Rezakhanlu F and
Sodagari N: Malignant schwannoma of anterior abdominal wall: report
of a case. J Clin Med Res. 1:233–236. 2009.
|
|
6
|
Kataoka D, Nonaka M, Yamamoto S, Kawada T,
Takaba T and Kunimura T: Multiple synchronous intrathoracic
neurilemmomas who had a past history of neurilemmoma on the
abdominal wall; report of a case. Kyobu Geka. 58:158–160. 2005.(In
Japanese).
|
|
7
|
Cho SB, Kim HS, Paik JH, Ryu DJ and Oh SH:
Dome-shaped tumor with surface changes on the abdominal wall. Clin
Exp Dermatol. 35:95–96. 2010.
|
|
8
|
Qin S, Yang C and Ren H: Cerebral hernia
caused by a thoracic surgery for multiple schwannomas in a patient
with neurofibromatosis type 2. Turk Neurosurg. 23:245–248.
2013.
|
|
9
|
Ogose A, Hotta T, Morita T, et al:
Diagnosis of peripheral nerve sheath tumors around the pelvis. Jpn
J Clin Oncol. 34:405–413. 2004.
|
|
10
|
Hu S, Chen Y, Wang Y, Chen KM and Song Q:
Clinical and CT manifestation of pleural schwannoma. Acta Radiol.
53:1137–1141. 2012.
|
|
11
|
Lao WT, Yang SH, Chen CL and Chan WP:
Mesentery neurilemmoma: CT, MRI and angiographic findings. Intern
Med. 50:2579–2581. 2011.
|
|
12
|
de Mesquita Neto JW, Lima Verde Leal RM,
de Brito EV, Cordeiro DF and Costa ML: Solitary schwannoma of the
cecum: case report and review of the literature. Case Rep Oncol.
6:62–65. 2013.
|
|
13
|
Rodriguez FJ, Folpe AL, Giannini C and
Perry A: Pathology of peripheral nerve sheath tumors: diagnostic
overview and update on selected diagnostic problems. Acta
Neuropathol. 123:295–319. 2012.
|