Introduction
Ameloblastic carcinoma, peripheral secondary type,
is a rare odontogenic carcinoma (1), and few cases of the intracranial
extension of these tumors have been reported. Ameloblastic
carcinoma is defined as a rare malignant odontogenic tumor that
retains the histological features of ameloblastoma and also
exhibits cytological features of malignancy (1–5).
11C-methionine positron emission tomography (PET) is the
most common method used to detect intracranial malignancies with
high resolution, as 11C-methionine is preferentially
absorbed in tissue with highly active amino acid and protein
synthesis. Protein synthesis is initiated at the first methionine
amino acid and the level of 11C-methionine uptake
indicates the level of protein synthesis. As the normal brain
tissue has low levels of protein synthesis activitiy, intracranial
malignant lesions usually uptake much higher levels of
11C-methionine. Predominantly, 11C-methionine
PET is applied to detect malignant lesions in the head and neck
region and has never been used for the detection of ameloblastic
carcinoma, due to the rarity of the tumor (6–8). The
current study presents a rare case of maxillary ameloblastic
carcinoma, peripheral secondary type, extending into the right
middle cranial fossa. In addition, the value of
11C-methionine PET is discussed with regard to detecting
ameloblastic carcinoma. The patient provided written informed
consent.
Case report
A 58-year-old male was admitted to the Hokuto
Hospital (Hokkaido, Japan) with a moderate headache and dizziness.
The patient had a normal level of consciousness. No evident central
nervous system disorders were observed. The patient had a history
of ameloblastoma, which had been treated 12 years prior to
admission. The post-operative follow-up for this occurrence had
been discontinued by the Obihiro-Kosei General Hospital (Obihiro,
Japan).
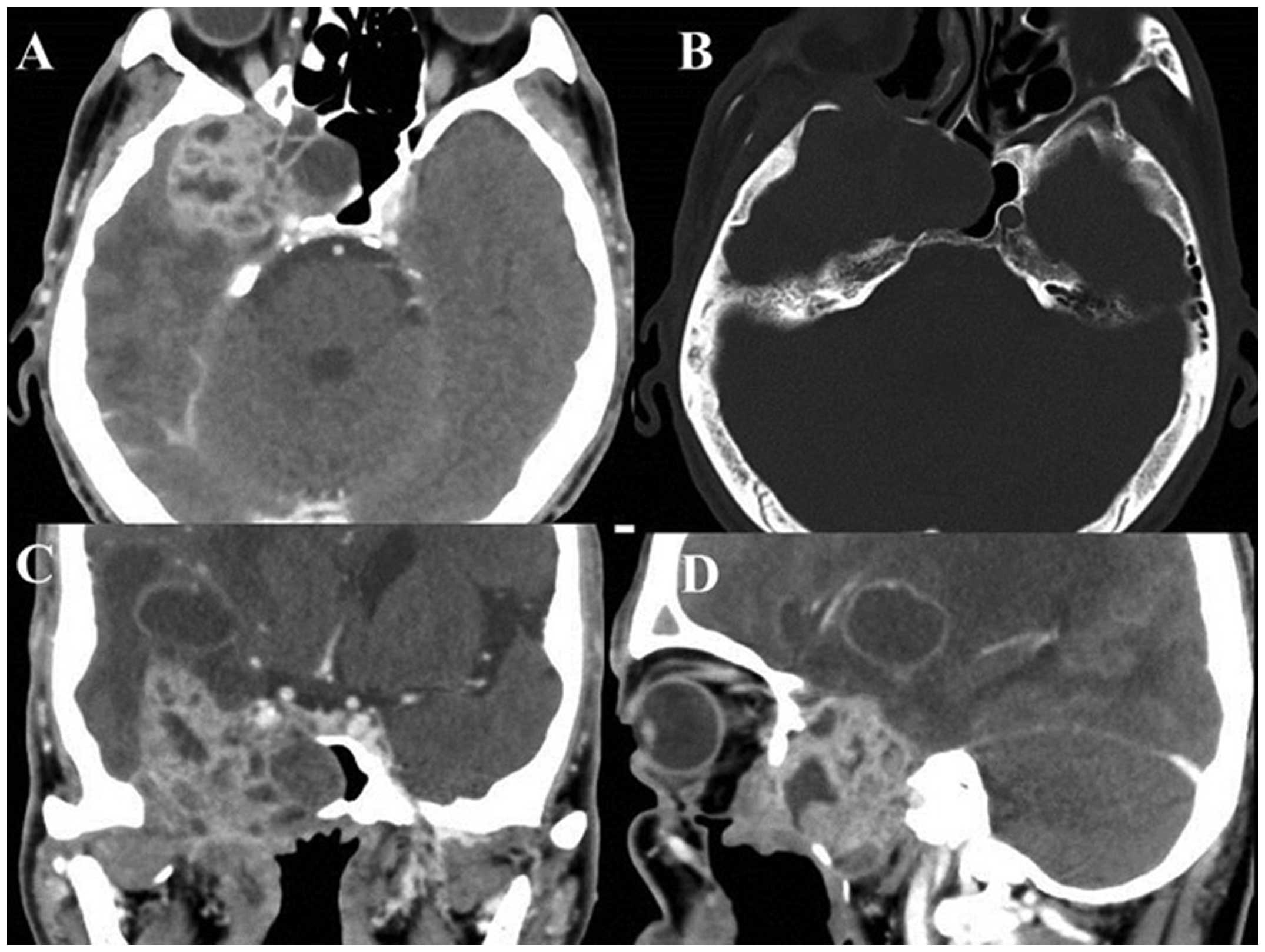
Computed tomography (CT) and magnetic resonance
imaging (MRI) revealed a mass lesion in the right infratemporal
fossa, middle cranial space and upper maxilla, with a wide-range
bone defect in the right middle skull base (Fig. 1 and 2). A histopathological specimen was
obtained from the tumor in the oral cavity. Hematoxylin and eosin
(HE) staining demonstrated marked atypia, high cellularity,
hyperkeratosis and necrosis surrounded by the typical ameloblastoma
histology (Fig. 3). MIB-1 staining
showed 25% positive cells in the lesion (Fig. 3). These findings indicated a
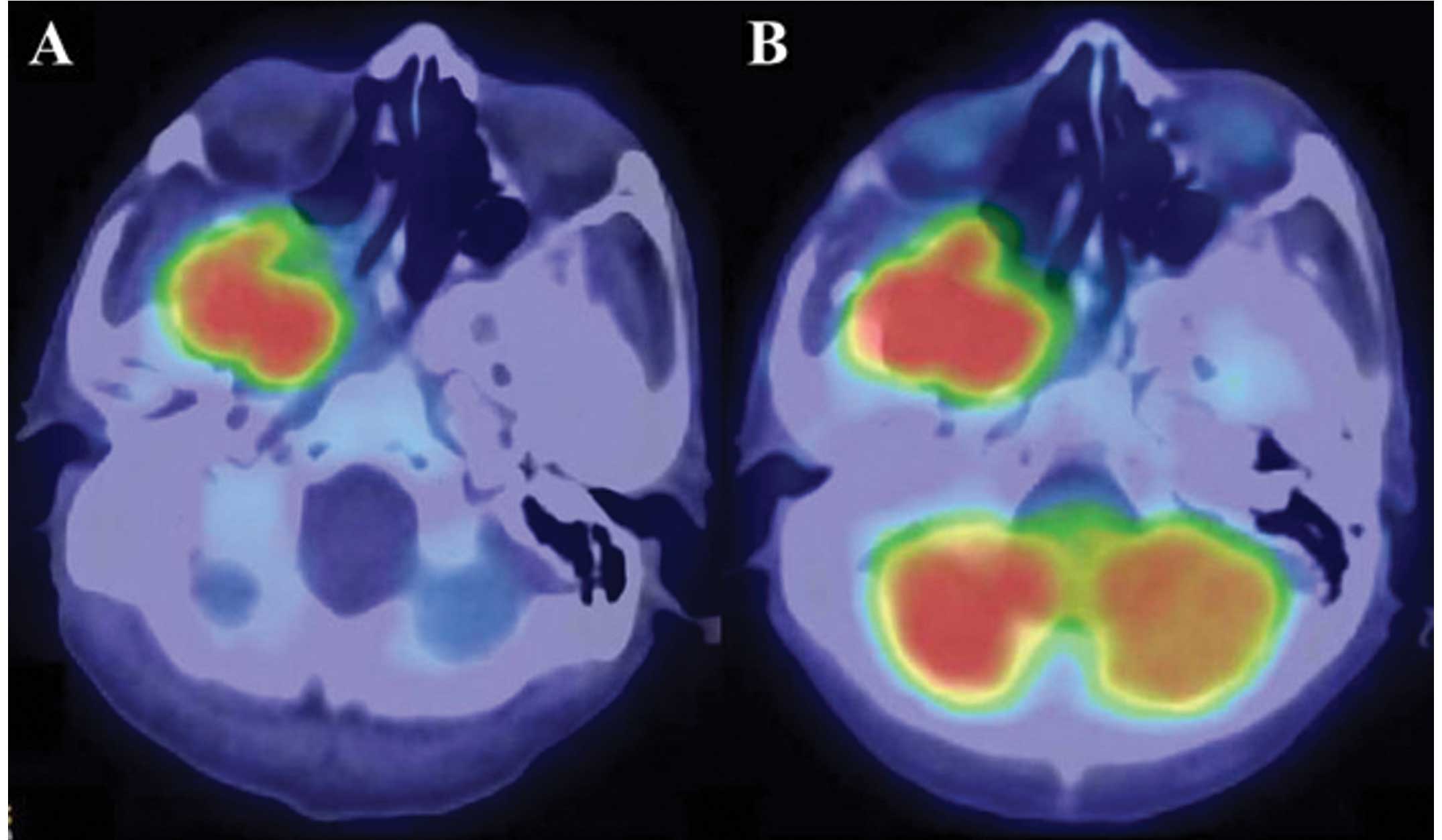
diagnosis of ameloblastic carcinoma. For contrast agents, 185 MBq
18F-fluorodeoxyglucose and 370 MBq 11C-methionine (10
mCi) were injected intravenously as bolus injections. PET revealed
a high level of accumulation of 18F-fluorodeoxyglucose (FDG) and
11C-methionine in the mass (Fig. 4). No evident lesions were detected,
except for the brain mass, on enhanced whole-body MRI or PET.
A surgical resection of the tumor was performed.
Almost all the tumor components were removed, except for a small
amount of remnant tissue around the right internal carotid artery.
During the early post-operative follow-up period, although neither
FDG-PET nor enhanced MRI could visualize the residual tissue,
11C-methionine PET was able to detect the tumor remnant
(Fig. 5). At present, the patient
is continuing a therapeutic course of radiation and evident mass
reduction has been observed. However, the therapeutic effects are
currently under consideration.
Discussion
According to the 2005 histological classification by
the World Health Organization (WHO), ameloblastic carcinoma is
classified into the primary type, the intraosseous secondary type
and the peripheral secondary type (1,2).
Whereas primary-type ameloblastic carcinoma develops de
novo, secondary-type ameloblastic carcinoma is derived from the
malignant transformation of ameloblastoma due to repeated
inflammatory stimulation (3).
Ameloblastic carcinoma exhibits cytological atypia, with or without
metastasis (4,5). In the present study, due to the
patient’s past history of ameloblastoma and the findings of
histopathological malignancy, a diagnosis of ameloblastic
carcinoma, peripheral secondary type, was made. Furthermore, the
ameloblastic carcinoma had extended into the intracranial space.
Although odontogenic tumors typically arise from oral cavity
tissues, one study in the English literature has indicated that
these lesions can grow in the head and neck region (9). Furthermore, a small number of studies
have also reported the intracranial extension of ameloblastoma
(10–14), while a few others have presented
cases of ameloblastic carcinoma with extension into the
intracranial space or cranial bone (15–17).
Enhanced CT or MRI and/or FDG-PET are generally used
to detect the regrowth or metastasis of tumors. In contrast, X-ray,
plain CT and enhanced CT are usually applied in cases of malignant
ameloblastoma or ameloblastic carcinoma. To the best of our
knowledge, the extension of these tumors into the intracranial
space is generally detected using plain or enhanced CT (10–14,16).
MRI is also useful for detecting the intracranial extension of
ameloblastic carcinoma (16).
Furthermore, FDG-PET is often applied to assess systemic metastasis
(17,18) and skull bone metastasis (17) of ameloblastic carcinoma. However, no
previous studies have reported the value of methionine PET for
treating ameloblastic carcinoma.
Generally, intracranial malignant lesions are
identified on enhanced CT or MRI. Although whole-body FDG-PET is
useful for detecting the systemic distribution of malignant lesions
(19–22), it is difficult to evaluate small
intracranial lesions by this method, as normal brain tissues also
exhibit the uptake of FDG to a certain extent (23,24).
As protein synthesis is upregulated in tumor cells compared with
that observed in the central nervous system, methionine PET is
useful for visualizing the clear border of intracranial malignant
lesions in cases of glioma (25).
In addition, a positive association has been reported between the
efficiency of methionine accumulation and the MIB-1 index, an
indicator of the proliferation of malignancy, in the setting of
rectal cancer metastasis (26). In
previous studies, FDG-PET has been described as a diagnostic tool
for detecting ameloblastic carcinoma (17–19).
The present study confirmed that methionine PET is superior to
FDG-PET in detecting intracranial ameloblastic carcinoma, with
remarkable sensitivity. In the present case, only methionine PET
was able to detect the extremely small amount of remnant tissue of
the post-operative ameloblastic carcinoma surrounding the internal
carotid artery (Fig. 5C and D). To
the best of our knowledge, there have been no previous studies
regarding the effectiveness of methionine PET in diagnosing
ameloblastic carcinoma. In this case, the accumulation of
methionine in the ameloblastic carcinoma lesion was clearly
observed on a PET scan (Fig. 4A and
5C). These findings indicate that
methionine PET is a more useful diagnostic tool than FDG-PET for
detecting intracranial ameloblastic carcinoma.
References
|
1
|
Yoshioka Y, Toratani S, Ogawa I and
Okamaoto T: Ameloblastic carcinoma, secondary type, of the
mandible: a case report. J Oral Maxillofac Surg. 71:e58–e62.
2013.
|
|
2
|
Barnes L, Eveson J, Reichat P and
Sidransky D: World Health Organization Classification of Tumours.
Pathology and Genetics of Head and Neck Tumours. IARC Press; Lyon,
France: pp. 286–291. 2005
|
|
3
|
Karakida K, Aoki T, Sakamoto H, et al:
Ameloblastic carcinoma, secondary type: a case report. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 110:e33–e37. 2010.
|
|
4
|
França DC, Moreira JM Jr, De Aguiar SM, De
Carvalhos AA and Goiato MC: Ameloblastic carcinoma of the maxilla:
A case report. Oncol Lett. 4:1297–1300. 2012.
|
|
5
|
Madan M, Singh J, Arora R and Bansal M:
Ameloblastic carcinoma: A case report and literature review. Int J
Appl Basic Med Res. 1:54–56. 2011.
|
|
6
|
Glaudemans AW, Enting RH, Heesters MA, et
al: Value of 11C-methionine PET in imaging brain tumours and
metastases. Eur J Nucl Med Mol Imaging. 40:615–635. 2013.
|
|
7
|
Crippa F, Alessi A and Serafini GL: PET
with radiolabeled aminoacid. Q J Nucl Med Mol Imaging. 56:151–162.
2012.
|
|
8
|
Gulyás B and Halldin C: New PET
radiopharmaceuticals beyond FDG for brain tumor imaging. Q J Nucl
Med Mol Imaging. 56:173–190. 2012.
|
|
9
|
Temporale H, Zatoński T, Roszkowska A and
Kręcicki T: Ameloblastoma of the nasal septum origin: a case
report. Case Rep Otolaryngol. Sep 21–2013.(Epub ahead of
print).
|
|
10
|
Takeuchi S, Kobayashi K, Minakawa T, Azumi
T and Fukushima M: Metastatic ameloblastoma of the skull. Surg
Neurol. 15:182–185. 1981.
|
|
11
|
Azumi T, Nakajima T, Takeuchi S, Fukushima
M and Ishiki T: Malignant ameloblastoma with metastasis to the
skull: report of case. J Oral Surg. 39:690–696. 1981.
|
|
12
|
Sato K, Sudo S, Fukuya Y and Sakuma H:
Maxillary ameloblastoma with intracranial invasion - case report.
Neurol Med Chir (Tokyo). 34:704–707. 1994.
|
|
13
|
Hayashi N, Iwata J, Masaoka N, Ueno H,
Ohtsuki Y and Moriki T: Ameloblastoma of the mandible metastasizing
to the orbit with malignant transformation. A histopathological and
immunohistochemical study. Virchows Arch. 430:501–507. 1997.
|
|
14
|
Leibovitch I, Schwarcz RM, Modjtahedi S,
Selva D and Goldberg RA: Orbital invasion by recurrent maxillary
ameloblastoma. Ophthalmology. 113:1227–1230. 2006.
|
|
15
|
Benlyazid A, Lacroix-Triki M, Aziza R,
Gomez-Brouchet A, Guichard M and Sarini J: Ameloblastic carcinoma
of the maxilla: case report and review of the literature. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 104:e17–e24. 2007.
|
|
16
|
Ozlugedik S, Ozcan M, Basturk O, et al:
Ameloblastic carcinoma arising from anterior skull base. Skull
Base. 15:269–273. 2005.
|
|
17
|
Devenney-Cakir B, Dunfee B, Subramaniam R,
et al: Ameloblastic carcinoma of the mandible with metastasis to
the skull and lung: advanced imaging appearance including computed
tomography, magnetic resonance imaging and positron emission
tomography computed tomography. Dentomaxillofacial Radiol.
39:449–453. 2010.
|
|
18
|
Matsuzaki H, Katase N, Hara M, et al:
Ameloblastic carcinoma: a case report with radiological features of
computed tomography and magnetic resonance imaging and positron
emission tomography. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 112:e40–e47. 2011.
|
|
19
|
Davis KR, New PF, Solis OJ and Roberson
GH: A review of the findings on computed cranial tomography
following intravenous contrast media. Rev Interam Radiol. 2:15–18.
1977.
|
|
20
|
Graif M and Steiner RE: Contrast-enhanced
magnetic resonance imaging of tumours of the central nervous
system: a clinical review. Br J Radiol. 59:865–873. 1986.
|
|
21
|
Wilms G, Marchal G, Demaerel PH, Van Hecke
P and Baert AL: Gadolinium-enhanced MRI of intracranial lesions. A
review of indications and results. Clin Imaging. 15:153–165.
1991.
|
|
22
|
Dillon WP: Imaging of central nervous
system tumors. Curr Opin Radiol. 3:46–50. 1991.
|
|
23
|
Olivero WC, Dulebohn SC and Lister JR: The
use of PET in evaluating patients with primary brain tumours: is it
useful? J Neurol Neurosurg Psychiatry. 58:250–252. 1995.
|
|
24
|
Chen W: Clinical applications of PET in
brain tumors. J Nucl Med. 48:1468–1481. 2007.
|
|
25
|
Van Laere K, Ceyssens S, Van Calenbergh F,
et al: Direct comparison of 18F-FDG and
11C-methionine PET in suspected recurrence of glioma:
sensitivity, inter-observer variability and prognostic value. Eur J
Nucl Med Mol Imaging. 32:39–51. 2005.
|
|
26
|
Koizumi M, Saga T, Yoshikawa K, et al:
11C-methionine-PET for evaluation of carbon ion
radiotherapy in patients with pelvic recurrence of rectal cancer.
Mol Imaging Biol. 10:374–380. 2008.
|