Introduction
Situs inversus totalis (SIT) is a rare congenital
condition characterized by a mirror-image transposition of the
abdominal and thoracic viscera, its incidence accounts for 1/8,000
to 1/25,000 of the worldwide population (1). Occasionally, patients with a
combination of this condition and malignant tumors have been
encountered.
Previous studies on the surgical procedures for
patients with SIT have documented technical difficulties, as the
anatomy is abnormal (2–4). Surgery for patients with SIT and
cervical cancer has been previously reported; however, to the best
of our knowledge, there has been no report of surgery for
endometrial cancer in patients with SIT in the English literature
to date (5). This study presents a
patient with endometrial cancer with SIT who underwent staging
laparotomy.
Written informed consent was obtained from the
patient for publication of this case report and accompanying
images.
Case report
A 44-year-old woman visited a local hospital
reporting abnormal vaginal bleeding for six months. Endometrial
biopsy revealed an endometrioid adenocarcinoma and the patient was
referred to Bursa Şevket Yılmaz Research and Education Hospital
(Bursa, Turkey) in March, 2013 for further evaluation and surgical
treatment.
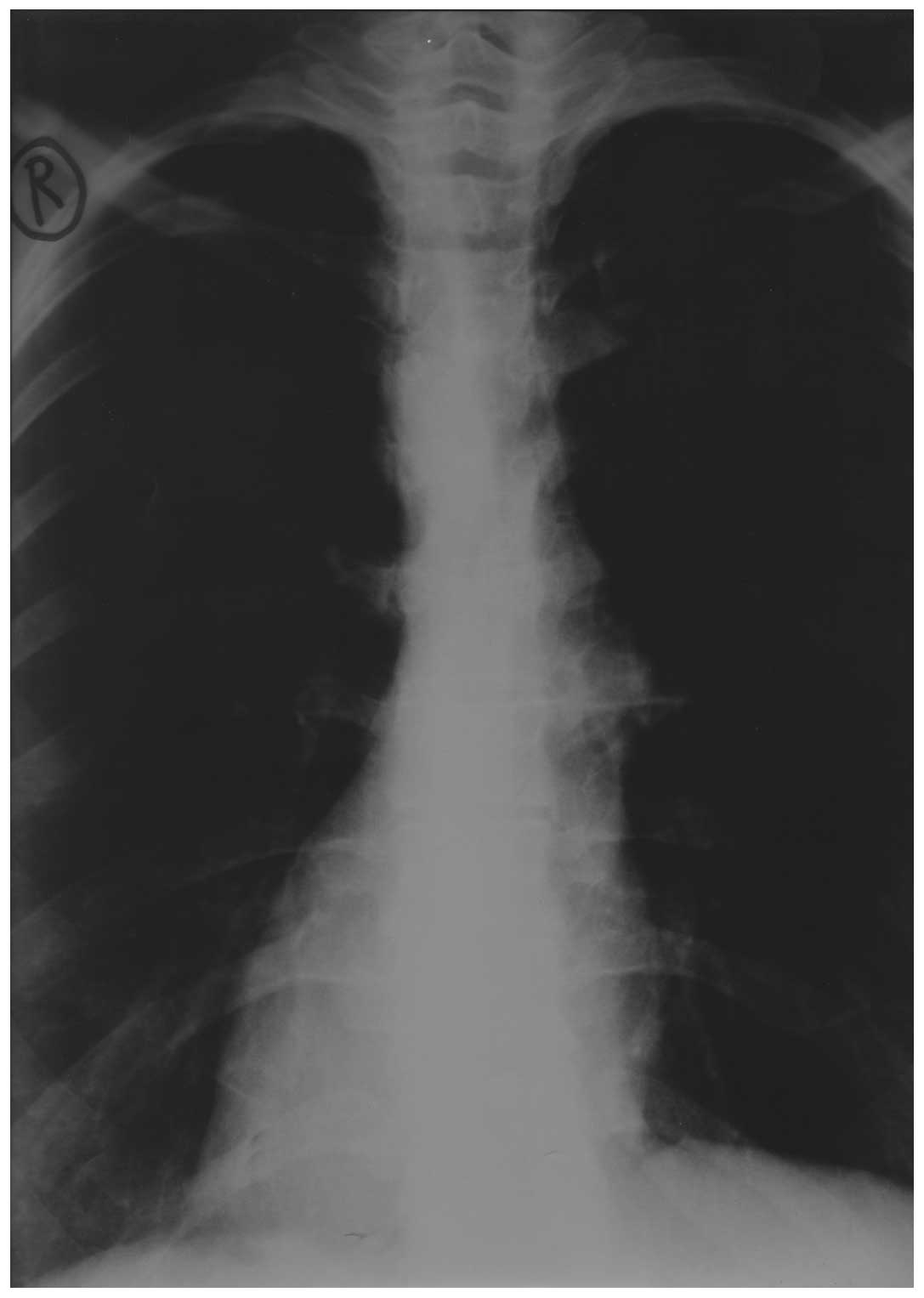
A standard preoperative chest radiograph revealed
dextrocardia with the stomach bubble situated on the right
(Fig. 1). Ultrasound and computed
tomography (CT) abdominal scanning revealed situs inversus.
Abdominal CT showed that all organs inside the abdomen were
inversely positioned without enlarged lymph node, distant
metastasis and abnormal course of vascularity. No other physical
abnormalities were noted. Routine laboratory tests yielded normal
results and the serum levels of carbohydrate antigen (CA) 19-9 and
CA 125 were normal.
In March, 2013, a staging laparotomy was performed.
Following administration of general anesthetic, the patient was
placed in a lithotomy position. The operator was situated on the
left and the first assistant was on the right (usual side of
surgery at the Bursa Şevket Yılmaz Research and Education
Hospital). The abdomen was explored through a midline incision. As
expected, complete transposition of the viscera was observed, the
stomach and spleen were lying on the right side, and the
gall-bladder, the large lobe of the liver and the caecum and
appendix were situated on the left. There was no macroscopic
serosal invasion and no evidence of ovarian, hepatic or peritoneal
metastases. Following explorative total abdominal hysterectomy,
bilateral salphingoophorectomy was performed. Pelvic
lymphadenectomy was performed in the usual manner. An incision in
the right lateral paracolic gutters with subsequent medial
reflection of the right colon was made to remove the right
para-aortic lymph nodes. An incision was then made in the
peritoneum overlying the left common iliac artery (the right in an
orthotopic patient). The incision was performed over the aorta to
the level of the duodenum. Using blunt dissection, the left ureter
and left ovarian vessels were identified and mobilized laterally.
The lymphatic tissue lateral to the left common iliac artery was
removed. The lymphatic packages were retrieved along the left side
of the aorta and the anterior surface of the inferior vena cava up
to the level of the renal veins (Fig.
2).
The position of the operator and assistant did not
differ from those in orthotopic patients. Total abdominal
hysterectomy, bilateral salphingoophorectomy and lymphadenectomy in
our patient were successfully performed by careful consideration of
the mirror-image anatomy. The total operation time was 3 h and 15
min, and the total blood loss was 1,280 ml.
Histological analysis of the resected specimen
confirmed the diagnosis of well-differentiated adenocarcinoma of
the endometrium infiltrating more than half of the myometrium.
Surgical staging showed no distant metastasis or metastatic lymph
nodes and the tumor was classified as stage 1B. The postoperative
course was uneventful and the patient was discharged from hospital
eight days after surgery. Following discharge, the patient received
adjuvant radiotherapy at the referred clinic (Department of Medical
Oncology, Ali Osman Sönmez Oncology Hospital, Bursa, Turkey).
Regarding the myometrial invasion, complementary radiation was
administered. Follow-up examinations revealed that the patient was
fit without any evidence of recurrence six months after surgical
treatment.
Discussion
SIT is inherited in an autosomal recessive manner
and requires great care due to abnormal anatomy. If the surgical
resection of any organ is required, it is important to understand
the association between the organ and its vascular structure
(6).
An increased risk of cardiac, splenic and
hepatobiliary malformations are found in patients with SIT
(7,8). Although rare malignant neoplasms have
been reported; this abnormality is not considered to be a malignant
entity (7).
In the present case, surgery itself presented
marginal difficulties. With SIT, abnormal vascularization of the
arteries and veins is common (9);
therefore, the preoperative confirmation of any abnormal
vascularization is important. The vascularity of our patient was
examined through abdominal CT scanning, which confirmed no evidence
of abnormal vascular malformation. In one study, CT alone was
considered to be insufficient for determining the vessel anatomy,
however, 3D reconstruction of an abdominal CT angiography image was
reported to obtain an improved result (10). During surgery the surgeon and
assistant may reverse positions, but is not likely to gain any
advantage. As a result, it is more important to understand the
anatomy and abnormal vascularization prior to surgery (11). To prevent surgery-related
complications, such as intraoperative bleeding or organ injury,
confidence in vascular anatomy and procedural carefulness are
mandatory. Therefore, surgery may be performed with a sufficient
number of retrieved lymph nodes and without additional blood loss
and time.
In conclusion, a review of the English literature
did not reveal any cases of endometrial carcinoma complicating
complete situs inversus. To the best of our knowledge, this is the
first study on staging laparotomy for an endometrial cancer patient
with SIT. Due to the frequency of associated malformations of
transposed organs and vascular anatomical variations that make
surgical management difficult, special attention should be paid to
diagnosis and preoperative staging.
References
|
1
|
Lee SE, Kim HY, Jung SE, Lee SC, Park KW
and Kim WK: Situs anomalies and gastrointestinal abnormalities. J
Pediatr Surg. 41:1237–1242. 2006.
|
|
2
|
Fujiwara Y, Fukunaga Y, Higashino M,
Tanimura S, Takemura M, Tanaka Y and Osugi H: Laparoscopic
hemicolectomy in a patient with situs inversus totalis. World J
Gastroenterol. 13:5035–5037. 2007.
|
|
3
|
Davies H, Slater GH and Bailey M:
Laparascopic sigmoid colectomy for diverticular disease in a
patient with situs inversus. Surg Endosc. 17:160–161. 2003.
|
|
4
|
Machado NO and Chopra P: Laparoscopic
cholecystectomy in a patient with situs inversus totalis:
feasibility and technical difficulties. JSLS. 10:386–391. 2006.
|
|
5
|
Shukunami K and Kotsuji F: Implication of
a reflected image illustration for pelvic lymphadenectomy on
uterine cervical cancer with situs inversus totalis. Gynecol Oncol.
84:5382002.
|
|
6
|
Yoshida M, Hino H, Machida H, Hatakeyama
N, Okano Y, Iwahara Y, Shinohara T and Oogushi F: Video-assisted
thoracic surgery lobectomy for lung cancer in a patient with
complete situs inversus. Gen Thorac Cardiovasc Surg. 61:155–159.
2013.
|
|
7
|
Yaghan RJ, Gharaibeh KI and Hammori S:
Feasibility of laparoscopic cholecystectomy in situs inversus. J
Laparoendosc Adv Surg Tech A. 11:233–237. 2001.
|
|
8
|
Sumi Y, Tomono A, Suzuki S, Kuroda D and
Kakeji Y: Laparoscopic hemicolectomy in a patient with situs
inversus totalis after open distal gastrectomy. World J
Gastrointest Surg. 27:22–26. 2013.
|
|
9
|
Benhammane H, Kharmoum S, Terraz S, Berney
T, Nguyen-Tang T, Genevay M, El Mesbahi O and Roth A: Common bile
duct adenocarcinoma in a patient with situs inversus totalis:
report of a rare case. BMC Res Notes. 5:6812012.
|
|
10
|
Min SH, Lee CM, Jung HJ, Lee KG, Suh YS,
Shin CI, Kim HH and Yang HK: Laparoscopic distal gastrectomy in a
patient with situs inversus totalis: a case report. J Gastric
Cancer. 13:266–272. 2013.
|
|
11
|
Benjelloun el B, Zahid FE, Ousadden A,
Mazaz K and Ait Taleb K: A case of gastric cancer associated to
situs inversus totalis. Cases J. 12:3912008.
|