Introduction
Brain metastases are a common complication in
patients with cancer and are an increasingly important cause of
morbidity and mortality (1). They
develop in 10–30% of adults and in 6–10% of children with cancer
(2–8). In adults, the most common types of
primary tumor responsible for brain metastases are lung (50%),
breast (15–20%), unknown primary (10–15%), melanoma (10%), and
colon (5%) (2,3). In children, the most common source of
brain metastases are sarcomas, neuroblastoma, and germ cell tumors
(2,9). Metastases from breast, colon, and
renal cell carcinoma are frequently single, while melanoma and lung
cancer have a greater tendency to produce multiple metastases
(2,10). They generally present in the cortex
of the frontal, parietal or temporal lobe, however, they rarely
invade the skull and meninges (6).
The current study, to the best of our knowledge, is the first
reported case of brain metastasis which simultaneously invaded the
subgaleal region, the skull, and the dural and cavernous sinuses.
In general, such patients can easily be misdiagnosed, so the
results of this case report may improve clinical studies of this
type.
Case report
In December 2010, a 54-year-old female presented at
the Tianjin Medical University General Hospital (Tianjin, China)
with a progressive headache of the left parietal area of the brain
that had persisted for one month. The patient provided written
informed consent. The results of the patient examination indicated
lethargy, double eyelid edema, a 5×7-cm2 purple swollen
area in the left frontal top scalp with tenderness, hypalgesia of
the left frontal scalp, chemosis, eye fixation and a positive
Babinski sign on the right side. The cerebrospinal fluid pressure
was 250 mmH2O, however, no other abnormalities were
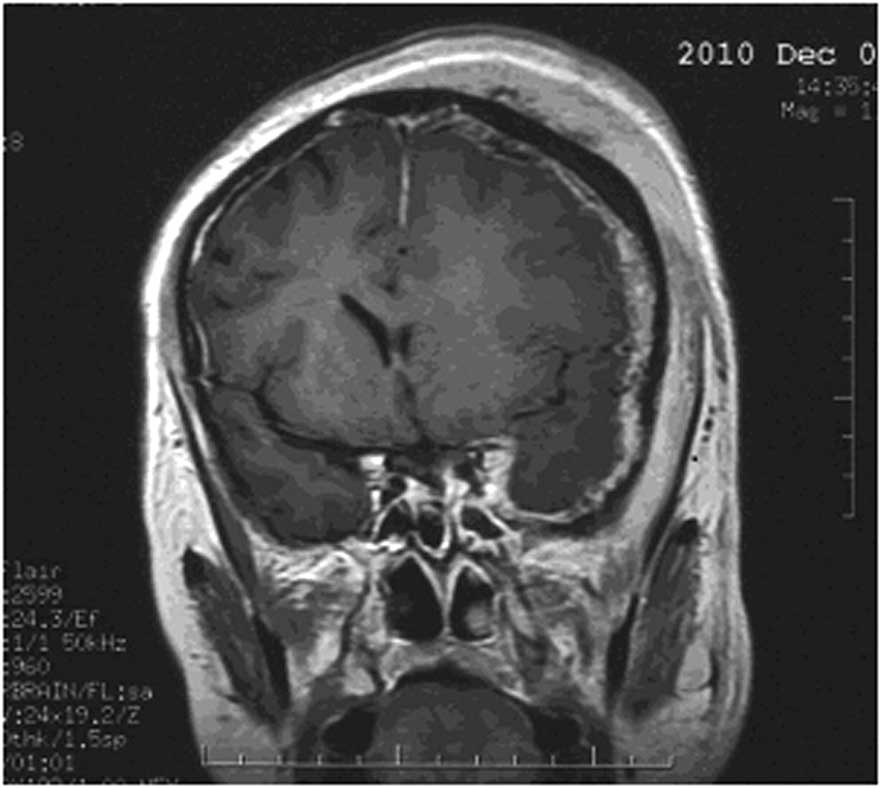
identified during the physical and laboratory examinations. Coronal
contrast-enhanced T1-weighted magnetic resonance imaging (MRI)
revealed a soft tissue swelling of the subgaleal tissue of the left
frontoparietal area, and a high intensity signal in the dural and
cavernous sinuses (Fig. 1). As a
result of the observations of the clinical manifestations, the
patient was initially diagnosed with an intracranial infection. The
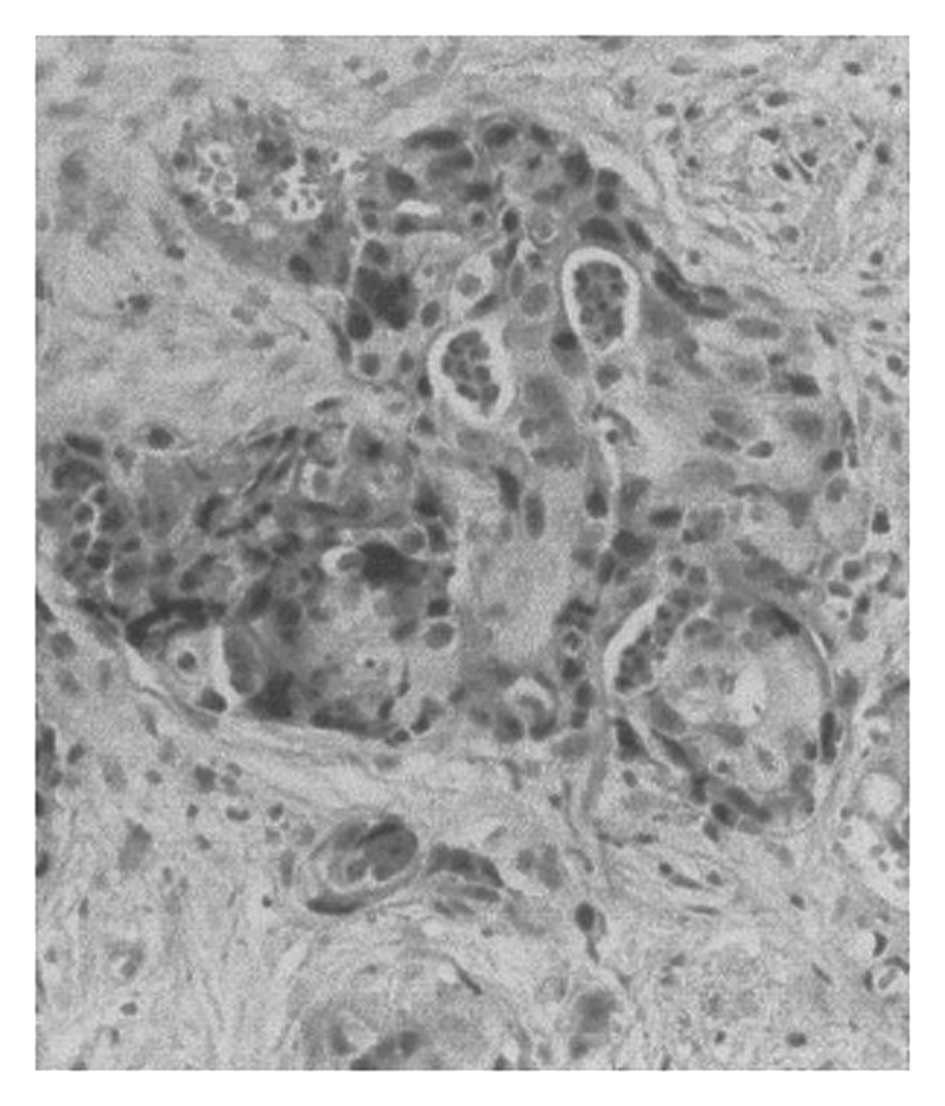
patient subsequently underwent a biopsy of the abnormal tissue,
which included tissue samples from the skull, dural sinus and
subgaleal region. The pathological diagnosis was determined as a
metastatic adenocarcinoma (Fig. 2).
However, following a series of imaging assessments, the primary
tumor was not located. In order to relieve the intracranial
hypertension, the patient underwent surgical resection of the
majority of the abnormal tissues and received a decompressive
craniectomy. The patient’s postoperative course was uneventful and
initially the symptoms improved. However, after two weeks, the
patient’s neurological condition began to progressively worsen.
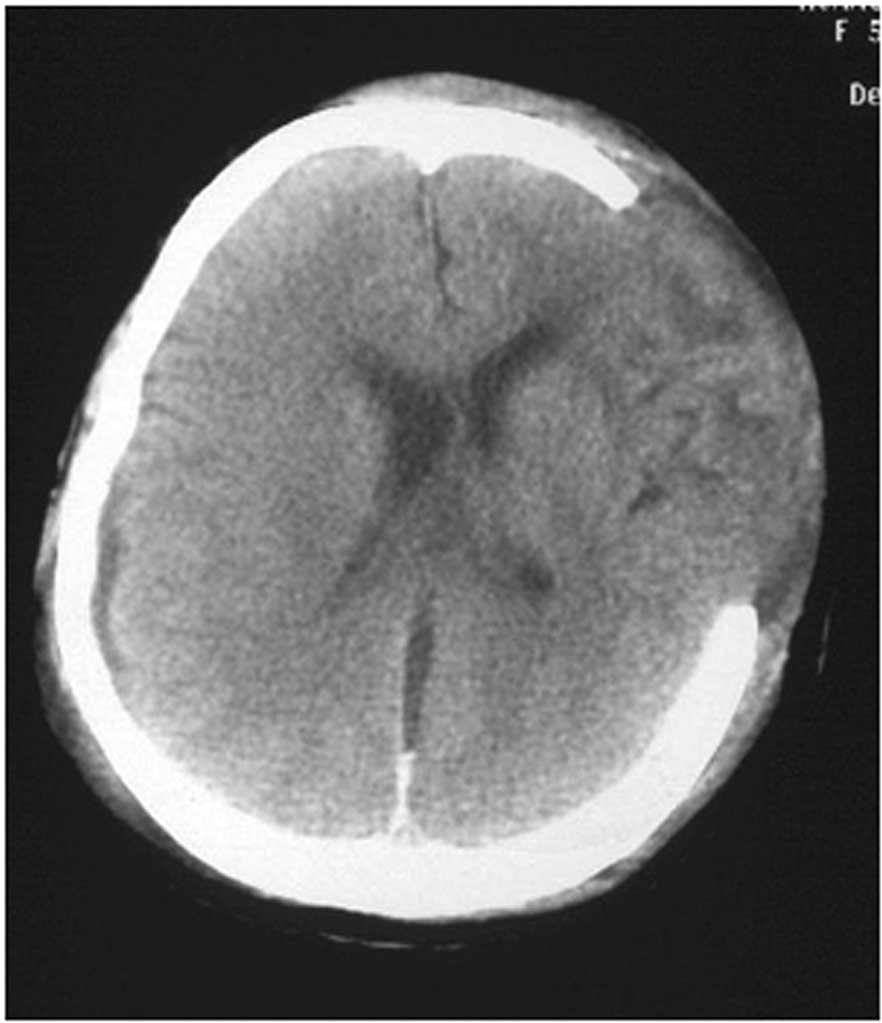
Axial computed tomography (CT) scan with a bone window demonstrated
a bulging growth in the brain tissue, which caused the ventricular
system to shift to the left (Fig.
3). Due to the widespread metastasis, the secondary surgical
removal had no effect. The patient declined further treatment and
succumbed after one month.
Discussion
According to previous studies, the majority of brain
metastases present in the brain parenchyma and rarely invade the
skull or the meningeal (11–13).
The current case of a patient with a brain metastatic carcinoma
invading the subgaleal region, skull, and the dural and cavernous
sinuses is considered to be particularly uncommon. In the present
case, due to the presence of intracranial hypertension, the sites
of high intensity signals in the MRI and the lack of a primary
tumor, the patient was misdiagnosed as presenting with an
intracranial infection. Therefore, the current case report presents
the clinical development of an unusual form of brain metastasis and
highlights the necessity for conducting a biopsy as soon as
possible in this type of patient.
In conclusion, in the patient described in the
present case report, the metastases invaded the subgaleal region,
the skull, and the dural and cavernous sinuses simultaneously,
which, to the best of our knowledge, has not previously been
reported. Although the patient underwent surgery (surgical
resection of the majority of the abnormal tissues and a
decompressive craniectomy), the patient succumbed after one month,
which is consistent with the poor prognosis associated with brain
metastases. This patient presented with intracranial hypertension;
however, the final diagnosis was determined via pathological
examination as a brain metastasis, although the primary tumor was
not found during the imaging examinations. Thus, this type of
patient may easily be misdiagnosed as exhibiting an intracranial
infection, therefore, performance of a biopsy is considered to be
necessary in the early stages of the diagnostic procedures.
Furthermore, the diagnosis of intracranial malignant metastases
must be considered for patients >40-year-old, who present with
rapid progression of clinical manifestations, such as a headache
and obvious intracranial hypertension, even when no primary tumor
is identified. The accurate diagnosis of this type of cancer relies
on the results that are obtained via biopsy; however, the prognosis
for this type of patient is generally poor.
References
|
1
|
Clouston PD, DeAngelis LM and Posner JB:
The spectrum of neurological disease in patients with systemic
cancer. Ann Neurol. 31:268–273. 1992.
|
|
2
|
Patchell R: Brain metastases. Handbook of
Neurology. 25:135–149. 1997.
|
|
3
|
Wen PY and Loeffler JS: Management of
brain metastases. Oncology (Williston Park). 13:941–962.
9691999.
|
|
4
|
Davey P: Brain metastases. Curr Probl
Cancer. 23:59–98. 1999.
|
|
5
|
Posner JB: Intracranial metastases.
Neurologic Complications of Cancer. FA Davis; Philadelphia, PA: pp.
77–110. 1995
|
|
6
|
Sawaya R, Bindal RK, Lang FF and Abi-Said
D: Metastatic brain tumors. Brain Tumors: An Encyclopedic Approach.
Kaye AH and Laws ER: Churchill Livingstone; Edinburgh: pp.
999–1046. 2001
|
|
7
|
Graus F, Walker RW and Allen JC: Brain
metastases in children. J Pediatr. 103:558–561. 1983.
|
|
8
|
Johnson JD and Young B: Demographics of
brain metastasis. Neurosurg Clin North Am. 7:337–344. 1996.
|
|
9
|
Bouffet E, Doumi N, Thiesse P, et al:
Brain metastases in children with solid tumors. Cancer. 79:403–410.
1997.
|
|
10
|
Delattre JY, Krol G, Thaler HT and Posner
JB: Distribution of brain metastases. Arch Neurol. 45:741–744.
1988.
|
|
11
|
Eichler AF and Loeffler JS:
Multidisciplinary management of brain metastases. Oncologist.
12:884–898. 2007.
|
|
12
|
Delattre JY, Krol G, Thaler HT and Posner
JB: Distribution of brain metastases. Arch Neurol. 45:741–744.
1988.
|
|
13
|
Elaimy AL, Mackay AR, Lamoreaux WT,
Fairbanks RK, Demakas JJ, Cooke BS, Peressini BJ, Holbrook JT and
Lee CM: Multimodality treatment of brain metastases: an
institutional survival analysis of 275 patients. World J Surg
Oncol. 9:692011.
|