Introduction
Desmoid tumors (DTs) are histologically benign
monoclonal myofibroblastic neoplasms. However, these tumors tend to
be locally invasive and infiltrate into the surrounding soft
tissue, but are lacking in metastatic potential (1).
Numerous studies have demonstrated that DTs account
for just 0.03% of all neoplasms and ~3% of all soft-tissue tumors
(2–5). The majority of cases occur between the
ages of 15 and 60 years old, with a peak incidence between 25 and
35 years old (6). The exact
etiology of DTs is complicated and remains unknown, however,
genetic abnormalities, such as familial adenomatous polyposis and
Gardner’s syndrome, and endocrine and physical factors play a role
in the pathogenesis of DTs (7,8). These
tumors commonly occur in the abdominal wall, followed by intra- or
extra-abdominal occurrences, including occurrences in the chest
wall and shoulder (9,10). Nevertheless, there have been few
reported cases of DTs originating from the lung. The present study
reports the computed tomography (CT) and pathological diagnosis
findings of a recurrent DT arising from the mediastinum in a
50-year-old female following treatment with surgery and
postoperative radiation. Patient provided written informed
consent.
Case report
A 50-year-old female presented with a dull pain in
the left scapular region and a decreased range of motion of the
left upper limb that had been present for five years. The patient
was treated at a local hospital in June 2009. A computed tomography
(CT) scan revealed a homogenous soft-tissue density mass lesion in
the superior lobe of the left lung. Surgery was performed within
the left side of the upper mediastinum and the tumor was completely
removed. The longest diameter of the mass was ~6.1 cm. Surgical
biopsies of the mass revealed a fibroma. However, in the year
following surgery, the pain in the left scapular region occurred
again and slowly progressed. Tumor recurrence was diagnosed through
a CT scan and histological examination of the tumor. The left chest
wall of the patient was treated with radiation therapy (64 Gy for
32 fractions). However, no notable improvement was found. The
patient was referred to the West China Hospital (Chengdu, Sichuan,
China) for a recurrent tumor of the mediastinum in November 2012. A
CT scan revealed that the left thoracic wall had collapsed and
there were two soft-tissue masses, located in the left pulmonary
apex and the costal pleura below the left plumonary apex,
respectively. The maximum cross-section was ~3.3×2.6 cm. The first
tumor was wrapped around the left subclavian artery and caused
erosion of the adjoining ribs (Fig.
1). The number of inflammatory nodules increased. Furthermore,
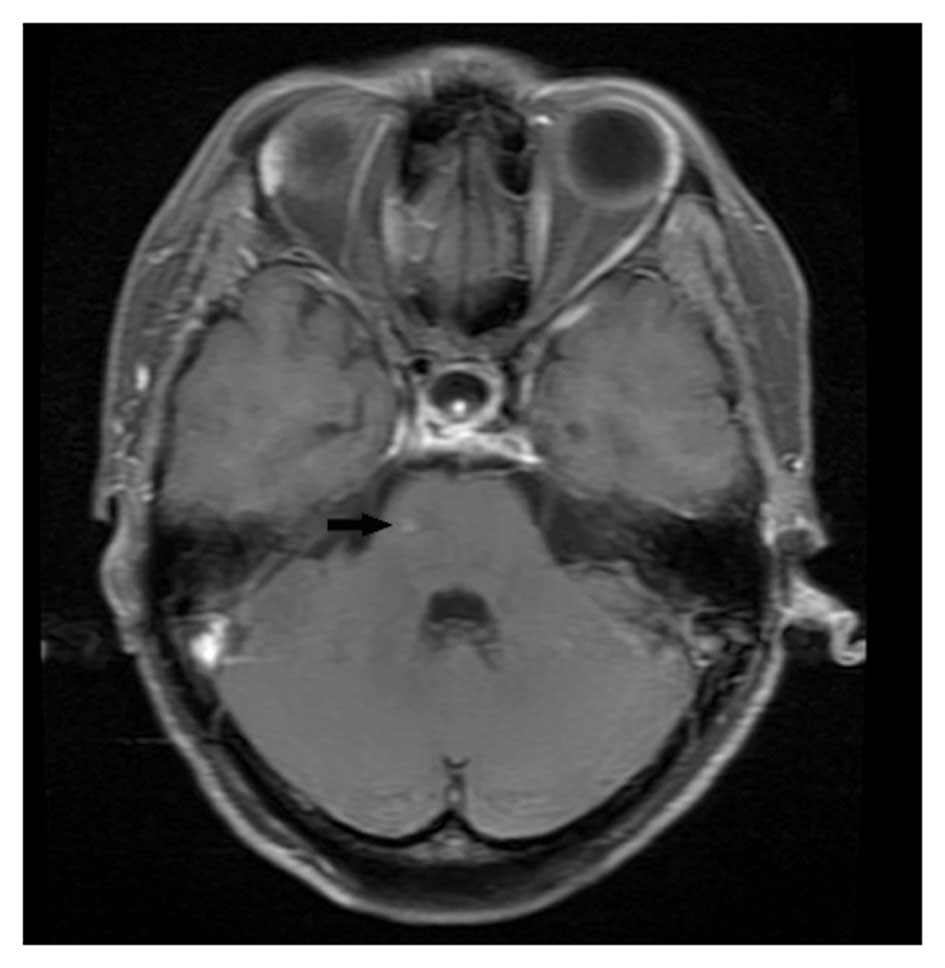
brain magnetic resonance imaging (MRI) showed a nodule measuring
0.3 cm in the right side of the pons (Fig. 2). A detailed general examination
showed no other metastatic or primary lesions. Histopathology
revealed a circumscribed tumor composed of spindle cells with bland
nuclei and extracellular collagen in the stroma (Fig. 3). The lesion was typical of a
fibromatosis (DT). A CT-guided puncture biopsy of the mediastinal
mass failed to provide a further pathological diagnosis. The nature
of the specific lesions in the pons was also not clear. Since the
recurrent DTs were extensively invasive, radical surgery may have
been difficult or even impossible. Considering that the quality of
life of the patient was not affected and to avoid the potential
complications of surgery or other treatments, the patient was
treated with a ‘wait-and-see’ policy. A 9-month clinical follow-up
was carried out, whereby CT scan (August 2013) revealed that the
left thoracic wall had collapsed and the presence of two
soft-tissue masses, located in the left pulmonary apex and the
costal pleura below the left pulmonary apex, respectively. In
comparison to the previous CT scan (November 2012), no changes in
the masses were identified. In addition, no changes in the size of
the mediastinal lymph nodes were identified. Brain MRI (August
2013) revealed a nodule measuring 0.3 cm in the right side of the
pons. Following the CT and MRI scans, the patient was determined to
be in a stable condition.
Discussion
In the present case, the DT originated from the
mediastinum, which is a rare location, and the recurrence occurred
one year after the initial surgery. However, the range of the
recurrent mass was wide and infiltrated up into the neck and down
into the lung. When purely analyzed by imaging, the tumor could be
misdiagnosed as a malignant tumor arising from the lung. The most
puzzling finding is that MRI revealed a nodule that could be
considered as brain metastasis in the right side of the pons.
Thus, the definitive diagnosis, classification and
differential diagnosis of DTs require a histopathological
examination (1,11). However, fine-needle aspiration may
not be useful due to the hypocellularity of this tumor (12). In the present case, one attempt was
made to obtain a pathological diagnosis of the patient by CT-guide
percutaneous lung puncture biopsy during the follow-up period,
however, this failed.
Complete surgical excision with wide tumor-free
margins is the current treatment for primary and recurrent DTs
(11). However, a ‘wait-and-see’
policy (13,14) was adopted as the therapeutic option
for the patient in the present study. The patient exhibited a
recurrent and widely invasive DT, and the left thoracic wall had
collapsed due to the primary wide radical resection, therefore, a
complete excision through reoperation would have been difficult to
achieve. Considering the unpredictable treatment complications and
the increased risk of mortality, only a long-term follow-up was
carried out. Furthermore, a previous study has reported that
reoperations are associated with a high risk of local recurrence
(15). An individualized and
comprehensive evaluation was required for the treatment of the
patient in the present study, and in fact, the recurrent DT and the
nodule in the right side of the pons were stable during the 9-month
follow-up and showed no brain metastasis.
Age, tumor location and margin status are all
factors associated with recurrence (16). If the DT becomes progressive, a
multimodal concept should be followed and another treatment should
be used singly or in combination, including chemotherapy (17), radiation therapy (18), hormonal therapy and targeted
therapy, such as the use of tyrosine kinase inhibitors (19).
In conclusion, the early detection of DTs and the
use of a complete surgical resection play an important role in the
prognosis. Long-term follow-up is an indispensable guide to future
treatment.
References
|
1
|
Escobar C, Munker R, Thomas JO, Li BD and
Burton GV: Update on desmoid tumors. Ann Oncol. 23:562–569.
2012.
|
|
2
|
Reitamo JJ, Scheinin TM and Häyry P: The
desmoid syndrome. New aspects in the cause, pathogenesis and
treatment of the desmoid tumour. Am J Surg. 151:230–237. 1986.
|
|
3
|
Papagelopoulos PJ, Mavrogenis AF,
Mitsiokapa EA, et al: Current trends in the management of
extra-abdominal desmoid tumours. World J Surg Oncol. 4:212006.
|
|
4
|
Wanjeri JK and Opeya CJ: A massive
abdominal wall desmoid tumor occurring in a laparotomy scar: a case
report. World J Surg Oncol. 9:352011.
|
|
5
|
Micke O and Seegenschmiedt MH: German
Cooperative Group on Radiotherapy for Benign Diseases: Radiation
therapy for aggressive fibromatosis (desmoid tumors): results of a
national Patterns of Care Study. Int J Radiat Oncol Biol Phys.
61:882–891. 2005.
|
|
6
|
Meazza C, Bisogno G, Gronchi A, et al:
Aggressive fibromatosis in children and adolescents: the Italian
experience. Cancer. 116:233–240. 2010.
|
|
7
|
Ferenc T, Sygut J, Kopczyński J, et al:
Aggressive fibromatosis (desmoid tumors): definition, occurrence,
pathology, diagnostic problems, clinical behavior, genetic
background. Pol J Pathol. 57:5–15. 2006.
|
|
8
|
Ling W, Kedong S, Hong W, Weiguo Z and
Decheng L: Desmoid tumor of posterior cruciate ligament of the
knee: a case report. BMC Musculoskelet Disord. 14:692013.
|
|
9
|
Mankin HJ, Hornicek FJ and Springfield DS:
Extra-abdominal desmoid tumors: a report of 234 cases. J Surg
Oncol. 102:380–384. 2010.
|
|
10
|
Kasper B, Ströbel P and Hohenberger P:
Desmoid tumors: clinical features and treatment options for
advanced disease. Oncologist. 16:682–693. 2011.
|
|
11
|
Arshad AR and Normala B: Surgical
management of large desmoid tumour of the anterior abdominal wall.
Asian J Surg. 31:90–95. 2008.
|
|
12
|
Aggarwal D, Dalal U, Mohapatra PR and
Singhal N: Intra-thoracic desmoid tumor. Lung India. 29:160–162.
2012.
|
|
13
|
Molloy AP, Hutchinson B and O’Toole GC:
Extra-abdominal desmoid tumours: a review of the literature.
Sarcoma. 2012:5780522012.
|
|
14
|
Fiore M, Rimareix F, Mariani L, et al:
Desmoid-type fibromatosis: a front-line conservative approach to
select patients for surgical treatment. Ann Surg Oncol.
16:2587–2593. 2009.
|
|
15
|
Abbas AE, Deschamps C, Cassivi SD, et al:
Chest-wall desmoid tumors: results of surgical intervention. Ann
Thorac Surg. 78:1219–1223. 2004.
|
|
16
|
Peng PD, Hyder O, Mavros MN, et al:
Management and recurrence patterns of desmoids tumors: a
multi-institutional analysis of 211 patients. Ann Surg Oncol.
19:4036–4042. 2012.
|
|
17
|
Al-Otaibi ML, Turcotte RE, Hings I, et al:
Low-dose chemotherapy for extra-abdominal desmoid tumor. Saudi Med
J. 29:1730–1734. 2008.
|
|
18
|
Gluck I, Griffith KA, Biermann JS, Feng
FY, Lucas DR and Ben-Josef E: Role of radiotherapy in the
management of desmoid tumors. Int J Radiat Oncol Biol Phys.
80:787–792. 2011.
|
|
19
|
Santos GA, Cunha IW, Rocha RM, et al:
Evaluation of estrogen receptor alpha, estrogen receptor beta,
progesterone receptor, and cKIT expression in desmoids tumors and
their role in determining treatment options. Biosci Trends.
4:25–30. 2010.
|