Introduction
Melanoma is a malignant tumor that is derived from
melanin-producing melanocytes. Although melanoma is a rare disease,
accounting for only 4% of all skin cancers, it is responsible for
80% of skin cancer-related mortalities worldwide (1). Between 3 and 15% of all cutaneous
melanomas affect the foot and ankle region and are associated with
a poor prognosis (2).
The treatment of malignant melanoma varies depending
on the tumor characteristics (for example, the stage or site).
Below-knee amputation is commonly adopted for the treatment of
malignant tumors of the foot and ankle, which effectively reduces
the recurrence rate, however, results in an increasing financial
and psychological burden for the patients (3). With the progress of microsurgical
reconstruction, limb salvage surgery using soft tissue
reconstruction has recently emerged as a potential alternative for
resectable malignant tumors of the extremities. The surgical
excision of melanoma, with adequate margins, is the fundamental
treatment that leads to recovery in the majority of cases (4). However, large, complex soft tissue
defects often remain following tumor excision, which are difficult
to reconstruct due to the exposure of the bones, joints and
tendons. Conversely, foot melanoma remains a challenge to surgeons
who are required to consider the oncologic resection whilst
preserving limb function (including, walking, moving and other
weight-bearing activities). Therefore, the availability of a safe,
easy and reliable reconstructive option is required to repair the
foot in the region of the melanoma. An ideal option would guarantee
the complete removal of the tumor as well as preservation of the
unique functions of the foot and ankle.
A variety of techniques, including skin grafting and
local- or free-tissue transfer, have been used for the soft tissue
reconstruction of the foot and ankle (5,6).
However, each has their own disadvantages and may not be suitable
for all patients. A cutaneous flap is a thick flap of skin whereby
the underlying subcutaneous layer is supplied with blood vessels
and nerves, and typically, a large quantity of subcutaneous fat.
Various reconstructive flaps have been used for repairing soft
tissue defects in the foot and ankle, including lateral
supramalleolar, medial plantar, reverse sural neurocutaneous
island, medial leg and lateral leg flaps. All of these types of
cutaneous flap yield satisfactory results (7–9).
The lateral supramalleolar flap was initially
described in 1988 by Masquelet et al (10), and is currently frequently used for
covering major tissue defects of the foot and ankle. It is usually
employed as a distally-based pedicle flap and has a wide range of
coverage that includes the whole dorsum of the foot, the medial and
lateral arches of the foot, and all of the regions of the heel
(11). The medial plantar flap is
one of the most versatile fasciocutaneous flaps of the foot, and
provides an ideal choice for the coverage of small plantar and
ankle defects, in terms of maintaining a good sensation and rapidly
enabling ambulation (12,13). The medial plantar flap has a wide
arc of rotation, which readily covers the plantar forefoot area.
The reverse sural artery neurocutaneous island flap was originally
described by Masquelet et al (14) in 1992 and is a distally-based flap,
which is generally accompanied by the sural nerve and vascularized
by the median superficial sural artery. It has been shown to be
ideal for coverage of the heel and the region of the lateral
malleolus of the foot, particularly for large soft tissue
defects.
Although cutaneous flaps have successfully been used
in the soft tissue reconstruction of the foot as a result of
trauma, infection and ischemia (7),
few studies have considered the results of cutaneous flap
reconstruction in patients presenting with a foot melanoma.
Therefore, the aim of the present study was to assess the
effectiveness of three types of cutaneous flap for reconstructing
soft tissue defects following melanoma resection.
Patients and methods
Patients and groups
A series of patients exhibiting melanoma involving
the foot and ankle, from the First Hospital of Jilin University
(Changchun, China) during the twelve-year period from January 1999
to December 2010, were retrospectively reviewed. A total of 21
patients (males, n=14; females, n=7) were enrolled in the present
study and the mean age was 54.2 years (range, 39–70 years). The
inclusion criteria were as follows: i) The patient diagnoses were
validated by postoperative biopsy; and ii) the patient’s skin
lesion was confined to the foot and ankle. Among the patients, 10
underwent amputation (group A) and the remaining 11 underwent
salvage surgery with soft tissue reconstruction (group S). One
patient was lost during the follow-up after 25 months; all of the
remaining patients were followed up for an additional 6–92 months
(median, 58 months) postoperatively. Patients provided written
informed consent and the study was approved by the ethics committee
of the First Hospital of Jilin University (Jilin, China).
Cutaneous flap design
Cutaneous flaps were designed based on the incision
size and anatomical characteristics of the affected area. Three
types of cutaneous flap, including the medial plantar, reverse
sural artery neurocutaneous island and the lateral supramalleolar
flap, were selected to repair the soft tissue defects of the foot
and ankle resulting from tumor resection. Specifically, a medial
plantar flap was used for the repair of the sole and forefoot; a
reverse sural neurocutaneous island flap was used for the repair of
the dorsum, sole and heel of the foot; and a lateral malleolus flap
was used for the repair of the lateral malleolus, dorsum and heel
of the foot.
The cutaneous flap design was guided by the
following rules: ii) The size and shape of the cutaneous flap must
be in accordance with the defect at the recipient site (not too
large or small). A cutaneous flap that is too large may cause a
bloated appearance of the skin, whereas a cutaneous flap that is
too small may influence the blood supply as a result of increased
local tension. ii) In order to secure a sufficient blood supply,
the pedicle of the cutaneous flap should be sufficiently wide and
long. iii) Considering that the foot comprises thin skin,
subcutaneous tissue and substantial joint activity, the cutaneous
flap for foot and ankle reconstruction is required to be as thin as
possible. If the cutaneous flap is too thick or bloated, it would
inevitably affect the activities of the ankle joint and aesthetics
of the foot. iv) The cutaneous flap for plantar reconstruction must
be wear-resistant and allow a protective sensation.
Surgical technique
Melanoma tumors were excised based on their site of
origin and anatomical characteristics. In group S, lesions were
widely excised using a margin of 3–5 cm in all cases and all
excisions extended into or included the deep fascia. Following
resection, frozen tumor sections underwent pathological testing, in
order to identify clean margins, and the exact size of the soft
tissue defect. Patients in group A underwent amputation, including
leg amputation, tarsometatarsal amputation and toe amputation.
Postoperative care and follow-up
Following surgery, all patients were admitted to a
specialized microsurgery intensive care unit for monitoring. The
patients were administered with postoperative chemotherapy and
biological therapy, either alone or in combination with
dacarbazine, cisplatin and intramuscular injection of
interleukin-2. Surgical complications, cutaneous flap survival,
tumor recurrence and metastasis, recovery of foot function, sensory
recovery, and patients’ complaints were observed during the
hospital stay and the follow-up period. The therapeutic efficacy
was observed in each group and compared.
Results
Patient cohort
The demographics of the patients in each group are
summarized in Table I. Among 21
patients, males outnumbered females at a ratio of 2:1 (males, n=14;
females, n=7), although previous studies revealed that melanoma may
be more prominent in females (15).
Of the 21 patients diagnosed with melanoma, nine were of the left
foot and 12 were of the right foot. In the present study, various
sites of the foot were found to be affected, including the sole of
the foot (n=7), the heel (n=4), the dorsum of the foot (n=3), the
toe (n=5) and the ankle joint (n=2). Patients commonly complained
of an increasing black mass, which bled easily when touched. The
mean course of disease in these patients was 60 days. According to
the European Organization for Research and Treatment of Cancer
criteria (16), at diagnosis, there
were 11 stage-I patients, seven stage-II patients and three
stage-III patients. Three patients (one in group S and two in group
A) exhibited ipsilateral inguinal lymph node metastases at
diagnosis, as confirmed by intraoperative inspection of a lymph
node biopsy.
 | Table IDemographics of the patients in groups
S and A. |
Table I
Demographics of the patients in groups
S and A.
| A, Group S |
|---|
|
|---|
| | | | | | | Post surgery |
|---|
| | | | | | |
|
|---|
| Patient no. | Gender | Age (years) | Affected foot | Location | Tumor stage | Surgical method | Follow-up
(months) | Recurrence/
Metastasis | Patient status |
|---|
| 1 | Female | 60 | Right | Lateral plantar
foot | I | Extended resection +
MPF + skin graft | 48 | No/No | Succumbed to CVD |
| 2 | Female | 49 | Left | Plantar | II | Extended resection +
MPF | 25a | No/No | N/A |
| 3 | Male | 63 | Right | Heel | II | Extended resection +
RSIF | 6 | Yes/Yes (Ing.) | DOD |
| 4 | Male | 63 | Right | Lateral dorsal
foot | I | Extended resection +
RSIF | 77 | No/No | AWD |
| 5 | Female | 55 | Left | Plantar | I | Extended resection +
MPF | 62 | No/No | AWD |
| 6 | Male | 39 | Right | Heel | II | Tumor resection +
RSIF | 13 | Yes/Yes
(Ing./Pop.) | DOD |
| 7 | Female | 54 | Right | Lateral
malleolus | II | Extended resection +
LSMF | 57 | No/No | AWD |
| 8 | Male | 57 | Right | Dorsum of foot | I | Extended resection +
RSIF | 62 | No/No | NED |
| 9 | Male | 70 | Left | Heel | III | Tumor resection +
RSIF | 8 | No/Yes (Lung) | DOD |
| 10 | Male | 61 | Left | Plantar | II | Extended resection +
MPF | 18 | No/No | NED |
| 11 | Female | 50 | Right | Heel | I | Extended resection +
RSIF | 13 | No/No | NED |
|
| B, Group A |
|
| | | | | | | Post surgery |
| | | | | | |
|
| Patient no. | Gender | Age (years) | Affected foot | Location | Tumor stage | Surgical method | Follow-up
(months) |
Recurrence/Metastasis | Patient status |
|
| 12 | Female | 52 | Right | Plantar | I | Leg amputation | 92 | No/No | NED |
| 13 | Male | 55 | Right | Medial dorsal
foot | I | Leg amputation | 73 | No/No | NED |
| 14 | Male | 58 | Left | Medial malleolus | II | Skin graft, leg
amputation | 22 | Yes/Yes
(Ing./Pop.) | DOD |
| 15 | Male | 46 | Left | Toe | I | Toe amputation | 68 | No/No | NED |
| 16 | Female | 45 | Left | Toe | I | Toe amputation | 58 | No/No | NED |
| 17 | Male | 59 | Right | Medial plantar
foot | I | Tarsometatarsal
amputation | 55 | No/No | NED |
| 18 | Male | 49 | Right | Toe | I | Leg amputation | 10 | No/No | NED |
| 19 | Male | 59 | Left | Toe | III | Toe amputation +
ilioinguinal lymph node dissection | 12 | No/Yes (Lung) | DOD |
| 20 | Male | 46 | Left | Second toe | III | Toe amputation | 9 | Yes/No | DOD |
| 21 | Male | 49 | Right | Plantar | II | Leg amputation | 29 | No/No | NED |
Postoperative course of the patients in
groups S and A
In group S, the size of the soft tissue defects
following excision of the melanoma ranged from 4×4 cm to 8×11 cm.
The reverse sural neurocutaneous island flap was used in six cases,
medial plantar flaps were used in four cases and a lateral
malleolus flaps was used in one case, for foot reconstruction
(Table II). The length of the
cutaneous flaps varied from 6 to 25 cm (mean, 12.2 cm) and the
width varied from 4 to 10 cm (mean, 6.6 cm). The patients were
administered with routine treatment, which included elevation of
the affected leg, anticoagulant agents, and anti-infection
medication following surgery. During the postoperative follow-up,
all cutaneous flaps survived the transfer and provided stable
defect coverage, good contour, and nine out of 11 patients were
able to ambulate with full weight bearing and no pain. For the
recovery of sensation, all five patients with medial plantar flaps
or a lateral supramalleolar flap obtained a good recovery of
sensation. However, when the reverse sural island flap was used as
an option for soft tissue defects of the foot, certain patients
complained about a loss of sensation on the lateral aspect of the
foot due to the routine sacrifice of the sural nerve during
surgery, which has been reported in a previous study (17).
 | Table IIFeatures of the cutaneous flaps
observed in the patients in Group S. |
Table II
Features of the cutaneous flaps
observed in the patients in Group S.
| Patient no. | Type of flap | Size of wound (cm ×
cm) | Size of flap (cm ×
cm) | Sensory
recovery | Wear-resistant | Short-term
complication |
|---|
| 1 | MPF | 4×4 | 6×4 | Yes | Yes | None |
| 2 | MPF | 5×4 | 8×6 | Yes | Yes | None |
| 3 | RSIF | 6×5 | 15×8 | No | No | Edema |
| 4 | RSIF | 11×8 | 25×8 | No | No | None |
| 5 | MPF | 6×5 | 8×7 | No | Yes | None |
| 6 | RSIF | 6×8 | 11×8 | No | Yes | None |
| 7 | LSMF | 4×4 | 8×4 | Yes | Yes | None |
| 8 | RSIF | 5×4 | 12×6 | Yes | Yes | Mild infection |
| 9 | RSIF | 8×9 | 25×10 | Yes | Yes | Mild infection,
partial necrosis |
| 10 | MPF | 5×4 | 8×6 | Yes | Yes | None |
| 11 | RSIF | 6×4 | 8×6 | Yes | Yes | Limited range of
motion |
The postoperative complication rate was an important
parameter to assess surgical success. The complications associated
with salvage surgery using cutaneous flap reconstruction were
observed in four patients. Two patients developed a mild infection
at the incision site and one patient developed edema. The symptoms
disappeared rapidly following symptomatic treatment. In addition to
a mild infection, one of the patients developed partial necrosis at
the distal tip of the cutaneous flap, however, experienced a
complete recovery within two weeks following debridement and
regular changing of the wound dressing (Table I). Another patient experienced a
limitation of ankle plantar flexion, as the heel did not completely
touch the ground when performing a squat. It was proposed that the
cutaneous flap may not have been adequately loose, or the patient
failed to do any exercise soon after surgery, thus resulting in
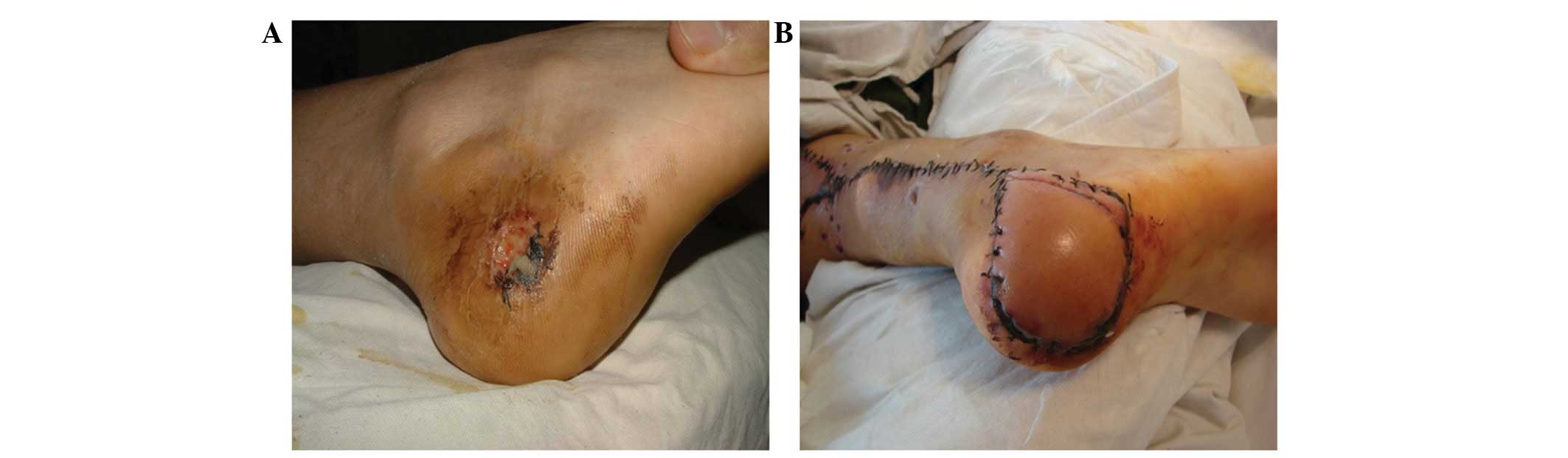
scar contracture around the defects. Figs. 1 and 2 present two patients who underwent
salvage surgery using cutaneous flap reconstruction (one using
medial plantar flaps and the other using a reverse sural
neurocutaneous island flap).
All patients in group A underwent amputation,
including leg, tarsometatarsal and toe amputation. One patient was
initially misdiagnosed with a benign tumor in another hospital, and
thereafter underwent tumor excision surgery and skin graft. Three
months later, the tumor recurred and the disease worsened. The
patient subsequently attended the First Hospital of Jilin
University, was diagnosed with a melanoma and underwent a lower leg
amputation. Another patient, who was diagnosed with melanoma in
another hospital, initially received a right toe tumor resection
and defect reconstruction using a dorsalis pedis artery flap. Two
weeks postoperatively, small black masses with visible exudation at
the cut edges were observed on the right toe. After transfer to the
First Hospital of Jilin University, pathological findings
identified the recurrence of melanoma and the patient’s leg was
amputated.
Patients in groups S and A demonstrated
similar oncologic outcomes
Not including one patient in group S who was lost
during the follow-up period, all of the patients were followed up
for 6–92 months (median, 58 months). The overall survival rate of
patients was 65.0% (13/20) with a median survival time of 57 months
(95% confidence interval [CI], 28.5–85.5 months) for group S and 58
months (95% CI, 50.5–65.5 months) for group A. Patients in the two
groups showed similar oncological outcomes. Not including one
patient in group S who succumbed as a result of cardiovascular
diseases four years following surgery, none of the patients with
clinical stage I (0/4 in group S and 0/6 in group A) succumbed due
to melanoma-associated causes. Furthermore, no patients developed
any signs of tumor recurrence or metastasis. For the seven patients
with clinical stage II melanoma, excluding one patient who was lost
during the follow-up period, the mortality rate in the two groups
was 50% (2/4 in group S and 1/2 in group A). The three patients
with clinical stage II succumbed to the disease at six, 13 and 22
months following surgery, due to tumor recurrence or
inguinal/popliteal lymph node metastasis. All three patients with
clinical stage III melanoma succumbed due to their disease at
eight, nine and 12 months due to tumor recurrence, or pulmonary or
ilioinguinal lymph node metastasis, irrespective of the group
assignment (Table I).
Discussion
Reconstruction of complex soft-tissue defects of the
foot following extensive excision of a tumor remains a challenge
due to the limited availability of local soft tissue, in addition
to the particular structural and functional characteristics of this
area. Recent studies have demonstrated and compared the benefits of
cutaneous flaps for the coverage of defects of the foot and ankle
(18,19), although primarily following trauma
or ischemia. Few studies have investigated the benefits of salvage
surgery using cutaneous flap reconstruction for the treatment of
foot melanoma. The present study represents a retrospective
analysis of a single-center experience for the use of cutaneous
flaps for soft tissue reconstruction as part of the treatment of
patients with foot and ankle melanoma.
The ideal reconstruction of the foot should provide
anatomical contour, durable skin, a protective sensation and, to a
certain extent, preserve limb function (standing, walking and
weight-bearing activities). Commonly, the amputation of a toe does
not impair the ability to walk and bear weight. Therefore, when
melanoma present on a toe or on the webbing between the toes, a toe
amputation at the nearest joint is often proposed prior to the
disease spreading to local lymph nodes. In the present study, five
patients underwent toe amputation, and one underwent leg amputation
(due to inguinal/popliteal lymph node metastasis).
The type of cutaneous flap was selected based on the
specific histological and anatomical features of the affected area.
Skin over the sole of the foot, particularly the weight-bearing
portion, requires reconstruction with similar tissues to obtain
long-term function. The heel is an important, integrated aspect of
the foot and is essential for smooth walking and weight-bearing
activities. Without the heel, the propelling function of the foot
during walking is severely interrupted. The medial plantar flap,
initially described by Harrison and Morgan (20) in 1981, is a fasciocutaneous island
flap raised from the non-weight bearing instep of the plantar foot.
The dominant vascular pedicle of the flap consists of the medial
plantar artery and venae comitantes. Furthermore, the medial
plantar flap has a similar texture (thick, glabrous plantar skin,
shock-absorbing fibro-fatty tissue and plantar fascia) and good
sensation and is, therefore, the ideal type of cutaneous flap for
plantar reconstruction, especially for weight-bearing heel defects
(21). Although this type of
cutaneous flap may be transferred to the defect as a proximally- or
distally-pedicled island flap, it is typically used for small- or
moderately-sized defects (13).
Koshima et al (22)
described a variant of this cutaneous flap that did not include
fascia and was based only on a perforator of the medial plantar
artery. Its advantages are that it requires an easier and shorter
dissection procedure and is associated with minimal donor-site
morbidity.
A reverse sural neurocutaneous island flap is
presented as an alternative to the cutaneous flaps that are
currently used for the reconstruction of large defects of the ankle
and heel. Its anatomical structures constitute the pedicle, the
superficial and deep fascias, the sural nerve, the short saphenous
vein and the superficial sural artery (23). The advantages of this type of
cutaneous flap include a simple dissection procedure, low
donor-site morbidity and a decreased surgical time when compared
with traditional coverage methods. Rohmiller et al (24) reported that 11 procedures using
reverse sural neurocutaneous flaps have been performed for
hind-foot and ankle defects (mean size, 53 cm2) and all
cutaneous flaps achieved stable coverage. However, certain patients
complained of a loss of sensation on the lateral aspect of the foot
due to the routine sacrifice of the sural nerve during surgery. Dai
et al (25) compared the
clinical outcome and complications following transfer of a fascia
pedicle- or a perforator pedicle-based sural neurocutaneous flap,
and the results demonstrated that the latter was a more reliable
and safe procedure for the coverage of soft tissue defects in the
lower extremities.
Large, complex, soft-tissue defects on the dorsum of
the foot are usually exposed to tendons, joints, bones, nerves and
vessels as the skin is thin, which renders reconstruction more
complex. The lateral supramalleolar flap is a fasciocutaneous flap
that is raised from the lateral aspect of the lower leg and
supplied by the perforating branch of the dorsal peroneal artery
(26). A previous study indicated
that the lateral supramalleolar flap is reliable and useful for
coverage of the dorsum of the foot, and the medial and lateral
arches of the foot, however, is not suitable for covering the
weight-bearing surface of the foot (27). Hamdi and Khlifi (26) described eight children who underwent
salvage surgery using the lateral supramalleolar flap for the
reconstruction of skin defects of the ankle, heel and foot. All
experienced satisfactory results, as no necrosis of the cutaneous
flap was reported and the donor site morbidity was minimal. In the
present study, the reverse sural neurocutaneous island flap was
used in six patients, a medial plantar flap in four patients and a
lateral malleolus flap in one patient, following the excision of
melanoma lesions in the ankles and feet, which achieved good
success rates.
In the present study, the cutaneous flaps varied in
size according to the dimensions of the lesion resulting from
extended resection of the tumor. The lesions ranged from 6×4 cm to
25×10 cm in diameter. The design of the cutaneous flaps is an
important factor when considering the final cosmetic appearance and
reducing complications during the postoperative period. In the
current study, the majority of the cutaneous flaps had sufficient
blood supply, which provided good anti-infection protection. Only
two patients developed a mild infection at the incision site
following the salvage surgery, which soon disappeared following the
administration of anti-infection treatment. In previous studies,
the most frequently described complication of a reverse sural
island flap was superficial flap necrosis. Afifi et al
(28) conducted a retrospective
study using 32 consecutive reverse sural flaps for foot and ankle
defects. Four patients had minor superficial loss of the cutaneous
flap and four patients experienced a delayed recovery. During the
follow-up of the present study, one of the patients demonstrated
superficial flap necrosis at the distal tip of the cutaneous flap,
and recovered completely within two weeks of debridement and
regular changes of the wound dressing.
The goal of melanoma treatment is to increase the
survival rate and the quality of life of cancer patients. Walsh
et al (29) reported that,
for patients with a melanoma of the foot/ankle, the overall
five-year survival rate was 52%, compared with 84% for patients
with a melanoma elsewhere on the lower extremities. Kang et
al (11) reported their
experience of using a distally-based island flap for soft tissue
reconstruction of the foot during limb salvage surgery for 13
melanoma patients. While all 13 cutaneous flaps survived completely
and provided normal weight-bearing ambulation, four patients
succumbed to their disease at seven, 10, 13 and 15 months following
surgery.
As foot melanoma is rare, numerous studies have
combined melanoma of the foot with the hand, leg or thigh for
statistical purposes, which add great variability to the survival
rate of foot melanoma, particularly when including a variety of
treatment options (15). The
present study compared the survival rate of patients with stage I,
II or III melanoma in groups of patients who underwent
reconstruction or amputation. Limb salvage surgery with cutaneous
flap reconstruction exhibited a similar survival rate, as well as
local recurrence and tumor metastasis, when compared with
amputation. Therefore, salvage surgery is recommended as a reliable
method to treat patients with melanoma of the foot and ankle,
particularly for the patients with stage I melanoma, enabling them
to avoid the trauma associated with leg amputation and experience
an improved quality of life. In addition, all patients in the
current study were administered with postoperative chemotherapy and
biological therapy, alone or in combination with dacarbazine,
cisplatin and intramuscular injections of interleukin-2, which
contributed to the efficacy of the therapy. Furthermore, a previous
study hypothesized that reasonable surgical adjuvant treatment
programs aided with reducing the risk of recurrence of melanoma and
improved the overall survival rate (30).
In conclusion, limb salvage surgery achieves
positive oncological and functional results with adjuvant
treatment, particularly for patients with stage I melanoma. The
medial plantar flap, reverse sural artery neurocutaneous island
flap and lateral supramalleolar flap all provide effective coverage
of soft tissue defects of varying sizes on the foot following the
wide excision of a melanoma.
References
|
1
|
Miller AJ and Mihm MC Jr: Melanoma. N Engl
J Med. 355:51–65. 2006.
|
|
2
|
Bristow IR, de Berker DA, Acland KM,
Turner RJ and Bowling J: Clinical guidelines for the recognition of
melanoma of the foot and nail unit. J Foot Ankle Res. 3:252010.
|
|
3
|
Papagelopoulos PJ, Mavrogenis AF, Badekas
A and Sim FH: Foot malignancies: a multidisciplinary approach. Foot
Ankle Clin. 8:751–763. 2003.
|
|
4
|
Testori A, Rutkowski P, Marsden J, et al:
Surgery and radiotherapy in the treatment of cutaneous melanoma.
Ann Oncol. 20(Suppl 6): vi22–vi29. 2009.
|
|
5
|
Yeh JT, Lin CH and Lin YT: Skin grafting
as a salvage procedure in diabetic foot reconstruction to avoid
major limb amputation. Chang Gung Med J. 33:389–396. 2010.
|
|
6
|
Langstein HN, Chang DW, Miller MJ, et al:
Limb salvage for soft-tissue malignancies of the foot: an
evaluation of free-tissue transfer. Plast Reconstr Surg.
109:152–159. 2002.
|
|
7
|
Ayyappan T and Chadha A: Super sural
neurofasciocutaneous flaps in acute traumatic heel reconstructions.
Plast Reconstr Surg. 109:2307–2313. 2002.
|
|
8
|
Yiacoumettis A and Mallouris A:
Reconstructive options for defects after melanoma excision in the
foot and ankle region. J Foot Ankle Surg. 50:498–503. 2011.
|
|
9
|
Lee YH, Rah SK, Choi SJ, Chung MS and Baek
GH: Distally based lateral supramalleolar adipofascial flap for
reconstruction of the dorsum of the foot and ankle. Plast Reconstr
Surg. 114:1478–1485. 2004.
|
|
10
|
Masquelet AC, Beveridge J, Romana C and
Gerber C: The lateral supramalleolar flap. Plast Reconstr Surg.
81:74–81. 1988.
|
|
11
|
Kang HG, Kim JH, Cho HS, Han I, Oh JH and
Kim HS: Soft tissue reconstruction of the foot using the distally
based island pedicle flap after resection of malignant melanoma.
Clin Orthop Surg. 2:244–249. 2010.
|
|
12
|
Duman H, Er E, Işík S, et al: Versatility
of the medial plantar flap: our clinical experience. Plast Reconstr
Surg. 109:1007–1012. 2002.
|
|
13
|
Oh SJ, Moon M, Cha J, Koh SH and Chung CH:
Weight-bearing plantar reconstruction using versatile medial
plantar sensate flap. J Plast Reconstr Aesthet Surg. 64:248–254.
2011.
|
|
14
|
Masquelet AC, Romana MC and Wolf G: Skin
island flaps supplied by the vascular axis of the sensitive
superficial nerves: anatomic study and clinical experience in the
leg. Plast Reconstr Surg. 89:1115–1121. 1992.
|
|
15
|
Rashid OM, Schaum JC, Wolfe LG, Brinster
NK and Neifeld JP: Prognostic variables and surgical management of
foot melanoma: review of a 25-year institutional experience. ISRN
Dermatol. 2011:3847292011.
|
|
16
|
Garbe C, Peris K, Hauschild A, Saiag P,
Middleton M, Spatz A, et al: European Dermatology Forum; European
Association of Dermato-Oncology; European Organization of Research
and Treatment of Cancer: Diagnosis and treatment of melanoma.
European consensus-based interdisciplinary guideline - Update 2012.
Eur J Cancer. 48:2375–2390. 2012.
|
|
17
|
Esezobor EE, Nwokike OC, Aranmolate S,
Onuminya JE and Abikoye FO: Sural nerve preservation in reverse
sural artery fasciocutaneous flap - a case report. Ann Surg Innov
Res. 6:102012.
|
|
18
|
Gir P, Cheng A, Oni G, Mojallal A and
Saint-Cyr M: Pedicled-perforator (propeller) flaps in lower
extremity defects: a systematic review. J Reconstr Microsurg.
28:595–601. 2012.
|
|
19
|
Hallock GG: A paradigm shift in flap
selection protocols for zones of the lower extremity using
perforator flaps. J Reconstr Microsurg. 29:233–240. 2013.
|
|
20
|
Harrison DH and Morgan BD: The instep
island flap to resurface plantar defects. Br J Plast Surg.
34:315–318. 1981.
|
|
21
|
Acikel C, Celikoz B, Yuksel F and Ergun O:
Various applications of the medial plantar flap to cover the
defects of the plantar foot, posterior heel, and ankle. Ann Plast
Surg. 50:498–503. 2003.
|
|
22
|
Koshima I, Narushima M, Mihara M, et al:
Island medial plantar artery perforator flap for reconstruction of
plantar defects. Ann Plast Surg. 59:558–562. 2007.
|
|
23
|
Almeida MF, da Costa PR and Okawa RY:
Reverse-flow island sural flap. Plast Reconstr Surg. 109:583–591.
2002.
|
|
24
|
Rohmiller MT and Callahan BS: The reverse
sural neurocutaneous flap for hindfoot and ankle coverage:
experience and review of the literature. Orthopedics. 28:1449–1453.
2005.
|
|
25
|
Dai J, Chai Y, Wang C, Wen G, Liu S and
Zhang W: Comparative study of two types of distally based sural
neurocutaneous flap for reconstruction of lower leg, ankle, and
heel. J Reconstr Microsurg. 29:125–130. 2013.
|
|
26
|
Hamdi MF and Khlifi A: Lateral
supramalleolar flap for coverage of ankle and foot defects in
children. J Foot Ankle Surg. 51:106–109. 2012.
|
|
27
|
Voche P, Merle M and Stussi JD: The
lateral supramalleolar flap: experience with 41 flaps. Ann Plast
Surg. 54:49–54. 2005.
|
|
28
|
Afifi AM, Mahboub TA, Losee JE, Smith DM
and Khalil HH: The reverse sural flap: modifications to improve
efficacy in foot and ankle reconstruction. Ann Plast Surg.
61:430–436. 2008.
|
|
29
|
Walsh SM, Fisher SG and Sage RA: Survival
of patients with primary pedal melanoma. J Foot Ankle Surg.
42:193–198. 2003.
|
|
30
|
Garbe C, Peris K, Hauschild A, et al:
Diagnosis and treatment of melanoma: European consensus-based
interdisciplinary guideline. Eur J Cancer. 46:270–283. 2010.
|