Introduction
In developed countries where the aging population is
increasing, cancer is one of the most prominent diseases with
regard to public welfare and health measures. One in four
mortalities in the USA, for example, is due to cancer (1). In the USA, the incidence of colorectal
cancer (CRC) has increased significantly in recent years due to the
changing lifestyle of the population and is currently one of the
most frequently exhibited malignancies and leading causes of
cancer-related mortality. The metastatic dissemination of primary
tumors is directly associated with patient survival, and distant
metastases, such as of the liver or lungs, are the major cause of
mortality in CRC patients. Furthermore, metastatic disease is the
most frequent reason for treatment failure (2). Therefore, the identification of genes
that are responsible for the development and progression of CRC,
and comprehension of the clinical significance of these genes is
critical for the diagnosis and adequate treatment of CRC. The
characterization of these key molecules is promising for the
development of novel treatment strategies for CRC.
The hepatocyte growth factor
(HGF)/mesenchymal-epithelial transition factor (MET)
signaling pathway was reported to have a key role in cellular
growth, invasiveness and metastasis (3–5). The
metastasis-associated in colon cancer-1 (MACC1) induces
MET expression and promotes HGF-induced scattering,
which the mitogen-activated protein kinase (MAPK) signaling
pathway prevents (6). This
indicates that MACC1 expression in primary tumors is
associated with metastasis and results in a poor prognosis.
The aim of the present study was to analyze the
correlation between MACC1 expression levels, in tissue
obtained from CRC patients, with their clinicopathological factors,
and to investigate the possible functions of MACC1 in the
metastasis of CRC.
Materials and methods
Clinical tissue samples
One hundred and seventy-four patients (99 males and
75 females) with CRC underwent curative surgery of CRC and distant
metastases (if present) at the Department of Gastroenterological
Surgery, Osaka University Graduate School of Medicine and Medical
Institute of Bioregulation at Kyusyu University (Osaka, Japan)
between 1994 and 2003. No patients had received chemotherapy or
radiotherapy prior to surgery. Primary CRC specimens and adjacent
normal colorectal mucosa were obtained from patients following
receipt of written informed consent, which was in accordance with
the institutional ethical guidelines. The surgical specimens were
fixed in formalin, processed through graded ethanol, and embedded
in paraffin. The sections were stained with hematoxylin and eosin
and Elastica van Gieson stain (Merck Millipore, Billerica, MA,
USA), and the degree of histological differentiation, lymphatic
invasion, and venous invasion was examined. Additionally, samples
of each specimen were frozen in liquid nitrogen immediately after
resection and stored at −80°C until RNA extraction. Following
surgery, the patients underwent follow-up blood examinations to
assess the tumor markers, serum carcinoembryonic antigen and cancer
antigen 19–9 and imaging, such as abdominal ultrasonography,
computed tomography and chest X-rays were conducted every 3–6
months. Postoperatively, stage III and IV patients received
5-fluorouracil-based chemotherapy [mFOLFOX6; 85 mg/m2
oxaliplatin and 2800 mg/m2 5-fluorouracil, for two weeks
for a total of 12 courses of treatment; 300 mg/m2/day
UFT, for 28 days for five weeks for five courses of treatment; 2500
mg/m2/day capecitabine for 14 days for three weeks for 8
courses of treatment, and/or 80 mg/m2/day TS-1 (tegafur,
gimestat and otastat potassium) for 28 days for six weeks and four
courses of treatment]. Adjuvant therapeutic strategies were
performed, except for stage I and II patients who received no
chemotherapy, according to the guidelines laid out by the Japanese
Society for Cancer of the Colon and Rectum (7). Clinicopathological factors were
assessed according to the tumor node metastasis (TNM)
classification system of the International Union Against Cancer
(8). This study was approved by the
ethics committee of Osaka University Graduate School of Medicine
(Osaka, Japan).
RNA preparation and expression
analysis
Total RNA was prepared using TRIzol reagent
(Invitrogen Life Technologies, Carlsbad, CA, USA) or using DNase
and a modified acid guanidinium-phenol-chloroform procedure
(9). Reverse transcription (RT) was
performed with SuperScript™ II (Invitrogen Life Technologies) or by
the methods reported previously (10) and an MACC1 fragment was
amplified by polymerase chain reaction (PCR). Two human
MACC1 oligonucleotide primers were designed as follows:
Forward, 5′-TTCTTTTGATTCCTCCGGTGA-3′ and reverse,
5′-ACTCTGATGGGCATGTGCTG-3′. A PCR kit (Takara Ex Taq; Takara Bio
Inc., Shiga, Japan) on a GeneAMP® PCR System 9600 (PE
Applied Biosystems, Foster City, CA, USA) was used to perform 35
cycles of PCR with the following parameters: 95°C for 40 sec, 45°C
for 40 sec and 72°C for 60 sec. An 8-μl aliquot of each reaction
mixture was size-fractionated in a 1.5% agarose gel and visualized
with ethidium bromide staining. To ensure the RNA was not degraded,
a PCR assay with primers specific for the
glyceraldehydes-3-phosphate dehydrogenase (GAPDH) gene was
performed for 1 min at 95°C, 1 min at 56°C, and 1 min at 72°C for
30 cycles. The GAPDH primers were as follows: Forward,
5′-TTGGTATCGTGGAAGGACTCA-3′ and reverse, 5′-TGTCATCATATTGGCAGGTT-3′
and produced a 270-bp amplicon. Complementary DNA (cDNA) from Human
Reference Total RNA (Clontech Laboratories, Mountain View, CA, USA)
was analyzed concurrently and served as a positive control. For
quantitative assessment, RT-qPCR was performed using a
LightCycler® FastStart DNA Master SYBR Green I kit
(Roche Diagnostics, Tokyo, Japan) for cDNA amplification of
MACC1 and GAPDH. The amplification protocol consisted
of 35 cycles of denaturation at 95°C for 10 sec, annealing at 60°C
for 10 sec, and elongation at 72°C for 10 sec. The products were
then subjected to a temperature gradient from 55°C to 95°C with
continuous fluorescence monitoring to produce a melting curve of
the products. The expression ratios of the MACC1 mRNA copies
in the tumor and normal tissues were calculated following
normalization against the GAPDH mRNA expression.
Statistical analysis
The association between MACC1 expression and
patient clinicopathological factors was analyzed using the
χ2 test. Kaplan-Meier survival curves were plotted and
compared with the generalized log-rank test. Univariate and
multivariate analyses were performed to identify prognostic factors
using a Cox proportional hazards regression model. The in
vitro assay values were analyzed using the Wilcoxon signed-rank
test. All tests were analyzed with JMP software (SAS Institute
Inc., Cary, NC, USA) and P<0.05 was considered to indicate a
statistically significant difference.
Results
Expression levels of MACC1 in clinical
tissue specimens
RT-qPCR analysis was performed on tissues from
primary CRC and adjacent normal colorectal regions. MACC1
expression was calculated by normalising it to GAPDH
expression for each tumor or normal tissue sample (Fig. 1). A significant difference was
identified between the tissue types, with the average expression in
tumor tissues larger than that of the corresponding normal tissues.
In the following analyses, MACC1 expression, normalized to
GAPDH expression, in tumor tissue was calculated following
division by MACC1/GAPDH expression in the normal
tissue.
Expression levels of MACC1 and patient
clinicopathological characteristics
For the clinicopathological evaluation, experimental
samples were divided into two groups according to the expression
status. Patients with values >1 (MACC1 expression level
of tumor tissue greater than that of the corresponding normal
tissue) were assigned to the high-expression group and patients
with values <1 were assigned to the low-expression group. The
clinicopathological factors that were associated with the
MACC1 expression status of the 174 patients are summarized
in Table I. The data indicates that
the level of MACC1 expression was not significantly
correlated with the clinicopathological factors.
 | Table IClinicopathological factors and
MACC1 mRNA expression in 174 colorectal cancer tissue
samples. |
Table I
Clinicopathological factors and
MACC1 mRNA expression in 174 colorectal cancer tissue
samples.
| Factor | Low expression n=31
(%) | High expression n=143
(%) | P-value |
|---|
| Age (years) |
| <68 | 19 (61.3) | 70 (48.9) | 0.212 |
| ≥68 | 12 (38.7) | 73 (51.1) | |
| Gender |
| Male | 13 (41.9) | 86 (60.1) | 0.063 |
| Female | 18 (58.1) | 57 (39.9) | |
| Histological
grade |
| Wel-Mod | 31 (100) | 134 (93.7) | 0.151 |
| Por-Muc | 0 (0) | 9 (6.3) | |
| Tumor size |
| <30 mm | 11 (35.5) | 41 (28.7) | 0.452 |
| ≥30 mm | 20 (64.5) | 102 (71.3) | |
| Tumor invasion |
| Tis | 7 (22.6) | 8 (5.6) | 0.006a |
| T1 | 4 (12.9) | 12 (8.4) | |
| T2 | 8 (25.8) | 23 (16.1) | |
| T3 | 9 (29.0) | 74 (51.7) | |
| T4 | 3 (9.7) | 26 (18.2) | |
| Lymph node
metastasis |
| N0 | 23 (74.2) | 83 (58.0) | 0.094 |
| N1-2 | 8 (25.8) | 60 (42.0) | |
| Lymphatic
invasion |
| Absent | 17 (54.8) | 83 (58.0) | 0.743 |
| Present | 14 (45.2) | 60 (42.0) | |
| Venous invasion |
| Absent | 27 (87.1) | 111 (77.6) | 0.237 |
| Present | 4 (12.9) | 32 (22.4) | |
| Distant
metastasis |
| M0 | 31 (100) | 134 (93.7) | 0.151 |
| M1 | 0 (0) | 9 (6.3) | |
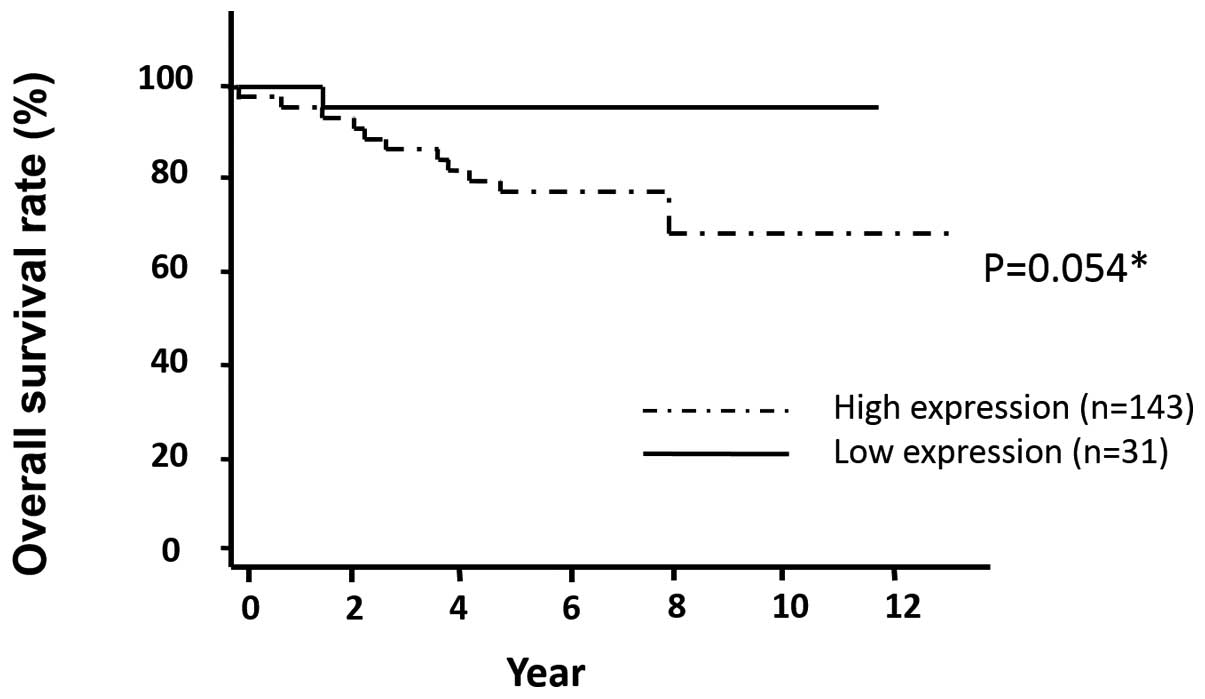
Association between MACC1 expression and
prognosis
The data showed that the postoperative disease-free
survival rate was significantly lower in patients in the
high-expression group than that of the low-expression group
(P=0.019; Fig. 2). The
postoperative overall survival rate was lower in patients in the
high-expression group than in the patients in the low-expression
group (P=0.054; Fig. 3). The median
follow-up was 4.1 years. Table II
shows the results of the univariate and multivariate analyses for
factors associated with disease-free survival. The univariate
analysis showed that age (P=0.035), tumor invasion (P<0.001),
lymph node metastasis (P<0.001), lymphatic invasion
(P<0.001), venous invasion (P=0.011), distant metastasis
(P<0.001) and MACC1 expression (P=0.005) were
significantly correlated with disease-free survival. The
multivariate regression analysis indicated in the MACC1
high-expression group (hazard ratio [HR], 2.27; 95% confidence
interval [CI], 1.01–9.71; P=0.044), lymph node metastasis (HR,
3.15; 95% CI, 1.44–7.48; P=0.003), lymphatic invasion (HR, 2.87;
95% CI, 1.28–6.86; P=0.010) and distant metastasis (HR, 12.83; 95%;
CI, 4.62–34.57; P<0.001) were independent predictors of
disease-free survival.
 | Table IIUnivariate and multivariate analyses
for disease-free survival (Cox proportional hazards regression
model). |
Table II
Univariate and multivariate analyses
for disease-free survival (Cox proportional hazards regression
model).
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|---|
| Factor | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age (years) |
| (<68/≥68) | 2.10 | 1.05–4.49 | 0.035 | 1.99 | 0.98–4.28 | 0.056 |
| Gender |
| (Male/Female) | 1.46 | 0.79–3.12 | 0.289 | | | |
| Histological
grade |
|
(Por-Muc/Wel-Mod) | 1.52 | 0.61–2.79 | 0.304 | | | |
| Tumor size
(mm) |
| (≥30/<30) | 1.38 | 0.93–2.18 | 0.106 | | | |
| Tumor invasion |
| (T3-4/Tis-2) | 7.11 | 2.53–29.64 | <0.001a | 1.69 | 0.52–7.62 | 0.403a |
| Lymph node
metastasis |
| (N1-2/N0) | 5.87 | 2.83–13.35 | <0.001a | 3.15 | 1.44–7.48 | 0.003a |
| Lymphatic
invasion |
|
(Present/Absent) | 3.71 | 1.85–7.94 | <0.001a | 2.87 | 1.28–6.86 | 0.010a |
| Venous
invasion |
|
(Present/Absent) | 2.62 | 1.25–5.21 | 0.011a | 2.24 | 0.98–5.06 | 0.054 |
| Metastasis |
| (M1/M0) | 10.18 | 4.25–21.95 | <0.001a | 12.83 | 4.62–34.57 | <0.001a |
| MACC1
expression |
| (High/Low) | 2.736 | 1.26–11.53 | 0.005a | 2.27 | 1.01–9.71 | 0.044a |
Discussion
HGF activates the HGF/MET
signaling pathway, which is involved in metastasis of CRC. The
HGF receptor, the gene for the receptor tyrosine kinase,
MET was identified as the first transcriptional target of
MACC1 (11). MACC1 is
located on chromosome 7 and was identified through genome-wide
expression analyses conducted on primary and metastatic colon
cancer (12). MACC1 binds
to, and promotes, MET gene expression by translocating from
the cytoplasm to the nucleus, leading to migration, invasion and
metastasis.
The present study demonstrated that MACC1
expression levels are an independent factor of disease-free
survival for CRC. Tumor malignancy was identified to correlate with
MACC1 expression levels and MACC1 expression may
affect the values of other prognostic factors in multivariate
analysis, such as distant metastasis, which was found to be
significant in univariate analysis. MACC1 expression levels
were a significant prognostic factor, reflecting disease-free
survival as well as the occurrence of distant metastasis. The
present study is considered to be important as it has provided
analyses of a large number of samples, which demonstrate that
MACC1 expression levels may be used as a statistically
significant marker for CRC metastasis following curative resection,
along with other reported predictors (13). The present results support recent
reports that a MACC1-dependent signaling pathway is involved
in the progression of CRC (12,14,15).
It is useful to determine the necessity for
intensive follow-up and adjuvant CRC therapy by predicting
recurrence and metastases following curative surgical resection
(16–18). Certain patients respond well to the
treatment of CRC, however others do not. Thus, more precise and
personalized predictions and strategies for treating metastases are
required (19). In the present
study, the clinicopathological analysis of a large number of
patients revealed that CRC samples exhibiting a low expression of
MACC1 were an improved predictor for disease-free and
overall survival when compared with the high-expression group. The
data indicates that MACC1 expression levels are an effective
predictor of CRC prognosis.
In CRC, various adjuvant chemotherapeutic strategies
are facilitative during certain disease stages and indicate the
usefulness of less invasive surgery for CRC (13,16–18,20–26).
For these cases, an informative prognostic marker, which is
independent from the traditional TNM classification and contributes
to diagnosis and treatment, is important. In conclusion, the
present data indicates MACC1 expression levels as a
potential prognostic marker for CRC. Whilst improved preoperative
and postoperative treatment strategies for CRC, such as chemo- and
radiotherapy combined with surgery, have contributed to the
reduction of recurrences, eventually half of the cases metastasize
despite the systemic chemotherapy and surgery (27). Adjuvant chemotherapy for CRC is
advantageous in cases where recurrence is considered to be likely.
In these cases, MACC1 expression level analysis may present
as a tool to predict poor prognosis and provide adequate treatment
for patients.
References
|
1
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010.
|
|
2
|
Stein U and Schlag PM: Clinical,
biological, and molecular aspects of metastasis in colorectal
cancer. Recent Results Cancer Res. 176:61–80. 2007.
|
|
3
|
Birchmeier C, Birchmeier W, Gherardi E and
Vande Woude GF: Met, metastasis, motility and more. Nat Rev Mol
Cell Biol. 4:915–925. 2003.
|
|
4
|
Mazzone M and Comoglio PM: The Met
pathway: master switch and drug target in cancer progression. FASEB
J. 20:1611–1621. 2006.
|
|
5
|
Sattler M and Salgia R: c-Met and
hepatocyte growth factor: potential as novel targets in cancer
therapy. Curr Oncol Rep. 9:102–108. 2007.
|
|
6
|
Potempa S and Ridley AJ: Activation of
both MAP kinase and phosphatidylinositide 3-kinase by Ras is
required for hepatocyte growth factor/scatter factor-induced
adherens junction disassembly. Mol Biol Cell. 9:2185–2200.
1998.
|
|
7
|
Watanabe T, Itabashi M, Shimada Y, et al:
Japanese Society for Cancer of the Colon and Rectum: Japanese
Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010
for the treatment of colorectal cancer. Int J Clin Oncol. 17:1–29.
2012.
|
|
8
|
Sobin LH and Fleming ID: TNM
classification of malignant tumors, fifth edition (1997). Union
Internationale Contre le Cancer and the American Joint Committee on
Cancer. Cancer. 80:1803–1804. 1997.
|
|
9
|
Mimori K, Mori M, Shiraishi T, et al:
Clinical significance of tissue inhibitor of metalloproteinase
expression in gastric carcinoma. Br J Cancer. 76:531–536. 1997.
|
|
10
|
Mori M, Staniunas RJ, Barnard GF, et al:
The significance of carbonic anhydrase expression in human
colorectal cancer. Gastroenterology. 105:820–826. 1993.
|
|
11
|
Stein U: MACC1-a novel target for solid
cancers. Expert Opin Ther Targets. 17:1039–1052. 2013.
|
|
12
|
Stein U, Walther W, Arlt F, et al: MACC1,
a newly identified key regulator of HGF-MET signaling, predicts
colon cancer metastasis. Nat Med. 15:59–67. 2009.
|
|
13
|
André T, Quinaux E, Louvet C, et al: Phase
III study comparing a semimonthly with a monthly regimen of
fluorouracil and leucovorin as adjuvant treatment for stage II and
III colon cancer patients: final results of GERCOR C96.1. J Clin
Oncol. 25:3732–3738. 2007.
|
|
14
|
Juneja M, Ilm K, Schlag PM and Stein U:
Promoter identification and transcriptional regulation of the
metastasis gene MACC1 in colorectal cancer. Mol Oncol. 7:929–943.
2013.
|
|
15
|
Zhang Y, Wang Z, Chen M, et al:
MicroRNA-143 targets MACC1 to inhibit cell invasion and migration
in colorectal cancer. Mol Cancer. 11:232012.
|
|
16
|
Wolpin BM and Mayer RJ: Systemic treatment
of colorectal cancer. Gastroenterology. 134:1296–1310. 2008.
|
|
17
|
Kornmann M, Formentini A, Ette C, et al:
Prognostic factors influencing the survival of patients with colon
cancer receiving adjuvant 5-FU treatment. Eur J Surg Oncol.
34:1316–1321. 2008.
|
|
18
|
Bathe OF, Dowden S, Sutherland F, et al:
Phase II study of neoadjuvant 5-FU + leucovorin + CPT-11 in
patients with resectable liver metastases from colorectal
adenocarcinoma. BMC Cancer. 4:322004.
|
|
19
|
Sadanandam A, Lyssiotis CA, Homicsko K, et
al: A colorectal cancer classification system that associates
cellular phenotype and responses to therapy. Nat Med. 19:619–625.
2013.
|
|
20
|
Iijima M, Kano Y, Nohno T and Namba M:
Cloning of cDNA with possible transcription factor activity at the
G1-S phase transition in human fibroblast cell lines. Acta Med
Okayama. 50:73–77. 1996.
|
|
21
|
Hansen WJ, Cowan NJ and Welch WJ:
Prefoldin-nascent chain complexes in the folding of cytoskeletal
proteins. J Cell Biol. 145:265–277. 1999.
|
|
22
|
Hodgson G, Hager JH, Volik S, et al:
Genome scanning with array CGH delineates regional alterations in
mouse islet carcinomas. Nat Genet. 29:459–464. 2001.
|
|
23
|
Lacy AM, García-Valdecasas JC, Delgado S,
et al: Laparoscopy-assisted colectomy versus open colectomy for
treatment of non-metastatic colon cancer: a randomised trial.
Lancet. 359:2224–2229. 2002.
|
|
24
|
Weeks JC, Nelson H, Gelber S, et al:
Short-term quality-of-life outcomes following laparoscopic-assisted
colectomy vs open colectomy for colon cancer: a randomized trial.
JAMA. 287:321–328. 2002.
|
|
25
|
No authors listed. Laparoscopically
assisted colectomy is as safe and effective as open colectomy in
people with colon cancer Abstracted from: Nelson H, Sargent D,
Wieand HS, et al: for the Clinical Outcomes of Surgical Therapy
Study Group. A comparison of laparoscopically assisted and open
colectomy for colon cancer. N Engl J Med. 350:2050–2059. 2004.
|
|
26
|
Jayne DG, Guillou PJ, Thorpe H, et al; UK
MRC CLASICC Trial Group. Randomized trial of laparoscopic-assisted
resection of colorectal carcinoma: 3-year results of the UK MRC
CLASICC Trial Group. J Clin Oncol. 25:3061–3068. 2007.
|
|
27
|
Koshariya M, Jagad RB, Kawamoto J, et al:
An update and our experience with metastatic liver disease.
Hepatogastroenterology. 54:2232–2239. 2007.
|