Introduction
Prostate carcinoma is the most prevalent and lethal
form of genitourinary cancer in males and is often identified
following serum prostate-specific antigen (PSA) testing (1). Unusual histological prostatic
carcinomas, which account for 5–10% of the carcinomas that
originate in the prostate, have been described, including small
cell carcinoma, sarcomatoid carcinoma (SC), squamous cell carcinoma
and adenosquamous carcinoma (ASC) (2). Mixed prostate carcinomas are extremely
rare and thus, no effective treatment has been identified and
prognosis is poor. The present study reports the case of a prostate
adenocarcinoma patient who developed mixed SC and ASC components
following hormonal therapy. Written informed consent was obtained
from the patient.
Case report
On March 4, 2011, a 62-year-old male presented to
the Department of Urology, Zunyi Medical College Fifth Affiliated
Hospital (Guangdong, China), with recurrent symptoms of urinary
retention and difficulty in voiding. During a routine physical
examination, an incidental elevated PSA level of 30.5 ng/ml (normal
range, 0–4 ng/ml) was identified. A bone scan revealed evidence of
multi-focal bone metastases to certain regions, including the
sternum, ribs, thoracic vertebrae, lumbar vertebrae, ilium, sacrum
and femur. The patient underwent a prostate needle biopsy on March
10, 2011. Microscopic examination of the biopsy specimens revealed
conventional poorly-differentiated adenocarcinoma of the prostate
(Gleason score, 4+5). The patient was diagnosed with advanced
prostate cancer, clinical stage T1cNxM1b, according to the
Guidelines on Prostate cancer, European Association of Urology,
2008 (3).
The patient was treated with adjuvant hormonal
therapy consisting of bicalutamide (50 mg a day) and triptorelin
(3.0 mg once every four weeks) for six months following the
confirmation of the diagnosis, and the initial response was good.
Treatment lasted until acute urinary retention occured. The serum
PSA level decreased to 0.401 ng/ml after two months, then decreased
further to 0.118 ng/ml after 3 months and finally decreased further
to the lowest level of 0.082 ng/ml after 4 months. The patient was
free of urinary symptoms 5 months after the prostate needle biopsy.
Over the ensuing time, recurrent and progressive urinary symptoms
developed and the patient was referred to the Department of Urology
again due to acute urinary retention, on September 12, 2011.
Catheterization was performed and the post-void residual urine
volume was ~400 ml. The PSA level had risen to 15.630 ng/ml. A
transurethral resection of the prostate (TURP) was performed to
improve the urinary symptoms. Pathological analysis revealed a
Gleason grade 5+5 adenocarcinoma of the prostate, with SC and ASC
components. One month later, the PSA level increased rapidly to
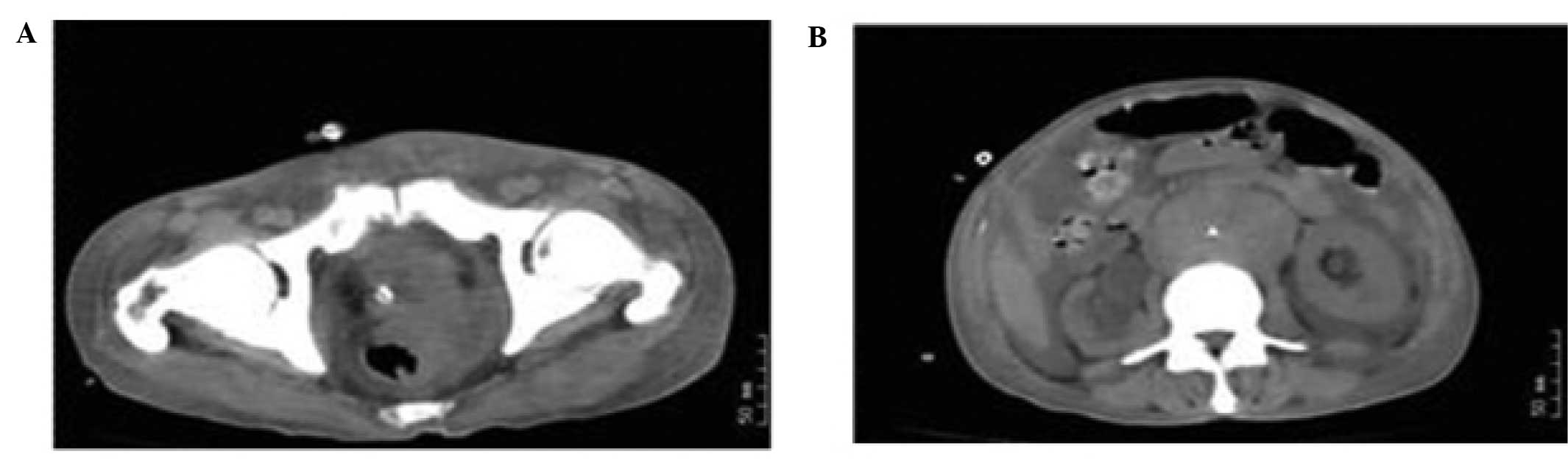
122.591 ng/ml. Computed tomography of the abdomen and pelvis
demonstrated multi-organ metastases, including metastases to the
rectum and retroperitoneal lymph nodes, with a hydrothorax and
ascites (Fig. 1). The patient’s
clinical stage was T4N1M1c. The patient’s condition deteriorated
rapidly and resulted in mortality due to multiple organ failure on
November 26, 2011.
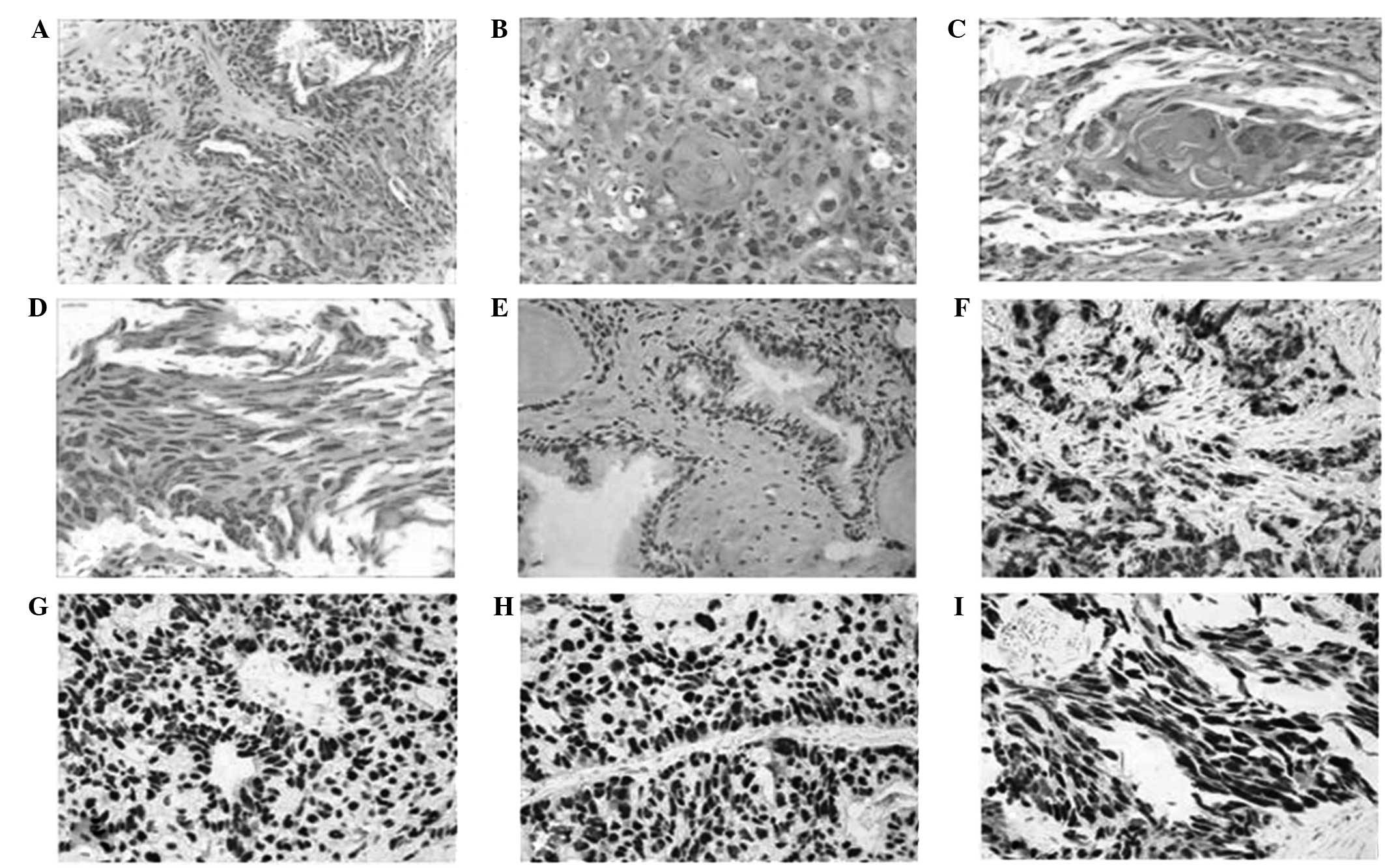
The first 13 biopsy specimens of the prostate
revealed conventional poorly-differentiated adenocarcinoma with
several acinar structures (Fig.
2A), with a Gleason score of nine out of 10, in four specimens
from the left base and one specimen from the right midzone.
Immunohistochemical studies revealed that the tumor cells were
positive for PSA and CK, and negative for vimentin and the S-100
protein. The specimen from a TURP procedure 6-month after hormonal
therapy, with a Gleason grade of 5+5, consisted of multiple
fragments of necrotic tissue weighing ~15g. Microscopic examination
of specimens from the TURP revealed different pathological
features. Conventional prostatic adenocarcinoma were identified.
The tumor was predominantly composed of sheets of small cells with
round or oval-shaped nuclei, vesicular nuclear chromatin and sparse
eosinophilic cytoplasm. Many of the cells appeared only as naked
nuclei. Focal areas of necrosis were present. Immunohistochemical
staining revealed that the tumor was positive for PSA and P504S.
The final diagnoses of SC, ASC and adenocarcinoma were made based
on histological studies (Fig.
2B–D). p53 was evaluated by immunohistochemistry (IHC) in
detail and the results are shown in Fig. 2.
Discussion
Mixed prostatic carcinoma is exceedingly rare and
its pathogenesis is not clear (4).
Previous studies have demonstrated that hormonal treatment and
radiotherapy may lead to changes in the nature of the tumor
(5). In the present study, the
patient was diagnosed with adenocarcinoma, ASC and SC following
hormonal treatment, and the patient’s condition progressively
deteriorated despite active treatment.
The patient was diagnosed with mixed prostatic
carcinoma by histological studies. The intercellular bridges and
the keratin pearls that were found by hematoxylin and eosin (HE)
staining confirmed the diagnosis of squamous cell carcinoma. In
addition, HE staining confirmed the mesenchymal differentiation in
the sarcomatoid component. In summary, the diagnoses of SC,
adenocarcinoma and ASC were made based on pathological
evidence.
Additionally, the p53 protein level in the biopsy
samples was evaluated by IHC. To the best of our knowledge, IHC
staining should be positive for wild-type p53 and for mutant-type
p53, but the wild-type p53 is only barely detectable by IHC
(6). The half-life of the wild-type
p53 protein is short, but mutant p53 exhibits an altered structure
that confers a longer half-life and greater stability compared with
wild-type p53. As a result, the majority of positive cells
represent mutant p53 (6). p53 is an
important tumor suppressor that is involved in numerous molecular
events, such as the regulation of DNA repair, apoptosis and
senescence, and it is induced by various stress signals, including
DNA damage and inflammation (7).
However, previous studies have shown that the aberration of p53 may
be the key event in the progression of carcinoma, as mutations in
p53 result in a strong predisposition to cancer in humans (8). The majority of mutant p53 proteins
lose their ability to bind wild-type p53-responsive elements and to
regulate the expression of p53 transcriptional targets, thus losing
tumor suppressor activity (9).
Therefore, cellular preservation of mutated p53 may confer
malignant potential, such as the capacity to metastasize, through
gain of function activities (9). In
the present study, the p53 level was markedly elevated in almost
all the carcinoma cell nuclei in the TURP specimen compared with
the needle biopsy staining, which indicated that p53 expression was
negative in the gland area and weakly positive in the interstitial
area (Fig. 2). The overexpression
of p53 suggested the presence of mutations in p53. Previous studies
have shown that mutations in p53 are possibly a mechanism to
explain the change from castration-sensitive prostate carcinoma to
castration-resistant prostate carcinoma (10). In the present patient, the change in
carcinoma characteristics and the case prognosis was possibly
associated with p53 mutation, according to the aforementioned
studies.
In conclusion, mixed carcinoma in the prostate is a
rare tumor with active clinical behavior. The disease often occurs
following radiation or hormonal therapy, but the mechanism
underlying its development is unclear. The present study speculates
that the variation in carcinoma type is possibly associated with
mutations in p53.
Acknowledgements
This study was supported by the Shenzhen Key Project
of Science and Technology (grant no. 200901015).
References
|
1
|
Siegel R, DeSantis C, Virgo K, et al:
Cancer treatment and survivorship statistics, 2012. CA Cancer J
Clin. 62:220–241. 2012.
|
|
2
|
Mazzucchelli R, Lopez-Beltran A, Cheng L,
Scarpelli M, Kirkali Z and Montironi R: Rare and unusual
histological variants of prostatic carcinoma: clinical
significance. BJU Int. 102:1369–1374. 2008.
|
|
3
|
Heidenreich A, Aus G, Bolla M, et al;
European Association of Urology. EAU guidelines on prostate cancer.
Eur Urol. 53:68–80. 2008.
|
|
4
|
Grignon DJ: Unusual subtypes of prostate
cancer. Mod Pathol. 17:316–327. 2004.
|
|
5
|
Hansel DE and Epstein JI: Sarcomatoid
carcinoma of the prostate: a study of 42 cases. Am J Surg Pathol.
30:1316–1321. 2006.
|
|
6
|
Zong L, Chen P, Jiang J, Wang L and Li QG:
Predictive value of p53 expression in the risk of malignant
gastrointestinal stromal tumors: evidence from 19 studies. Exp Ther
Med. 3:87–92. 2012.
|
|
7
|
Prives C and Hall PA: The p53 pathway. J
Pathol. 187:112–126. 1999.
|
|
8
|
Melino G: p63 is a suppressor of
tumorigenesis and metastasis interacting with mutant p53. Cell
Death Differ. 18:1487–1499. 2011.
|
|
9
|
Monti P, Perfumo C, Bisio A, et al:
Dominant-negative features of mutant TP53 in germline carriers have
limited impact on cancer outcomes. Mol Cancer Res. 9:271–279.
2011.
|
|
10
|
Schlomm T, Iwers L, Kirstein P, et al:
Clinical significance of p53 alterations in surgically treated
prostate cancers. Mod Pathol. 21:1371–1378. 2008.
|