Introduction
Sinonasal inverted papilloma (SNIP) is derived from
the benign tumors of the epithelial cells and comprises 0.5–7.0% of
all diagnosed sinonasal tumors. SNIP has the potential to recur and
exhibit malignant characteristics, including atypia, dysplasia and
and carcinoma in situ (1).
Although the incidence of SNIP with carcinoma differs widely
according to various reports (2–53%) (2), the incidence has been observed as 11%
in a recent large study (2). To
date, the accurate cause of SNIP is not fully understood. There are
currently no reliable predictor or biological markers for
recurrence or malignancy. Surgery is the main treatment option for
patients with SNIP (2). The SNIP
can progress to squamous cell carcinoma (SCC) with a high degree of
differentiation, and has an improved outcome compared with that of
pure primary SCC following treatment (3,4). SCC
often occurs in the SNIP itself, presenting as atypical hyperplasia
or cancer of various histological stages (5). The present study retrospectively
analyzed the clinical data of 32 cases of malignant SNIP. The
associations between the clinical/histopathological characteristics
of the patients and SNIP malignancy, along with their association
with patient survival, were analyzed in order to improve the
understanding of the prognosis of patients with malignant SNIP.
Patients and methods
Clinical data
A total of 356 SNIP patients received treatment at
the Department of Otorhinolaryngology Head and Neck Surgery,
Tianjin Huanhu Hospital (Tianjin, China) between January 1991 and
January 2008. Of these, 32 cases were pathologically confirmed to
have malignant SNIP. Therefore, the present study retrospectively
analyzed the data of the 32 cases, which included patient age,
gender, disease location, clinical staging and surgical treatment.
The study was approved by the ethics committee of Tianjin Huanhu
Hospital and written informed consent was obtained from all
patients.
Histopathological analysis
All pathological sections were analyzed by three
highly qualified pathologists who were blinded to patient data.
According to the differentiation of malignant cells, tumor sections
were classified into three differentiation levels, well-,
moderately and poorly differentiated according the the
classification by the World Health Organization (6). In a typical tissue section, the
percentage of malignant cells was graded as follows: I, ≤25%
malignant cells; II, 26–50% malignant cells; III, 51–75% malignant
cells; IV, ≥76% malignant cells (6).
Follow-up procedure
All patients were followed up, for periods ranging
between 23 to 212 months, with an interval of three months between
each follow-up, by telephone and letter. The patients’ referral
statuses were obtained, so as to evaluate the current condition and
tumors status of the patients.
Statistical analysis
SPSS 17.0 software (SPSS, Inc., Chicago, IL, USA)
was used for statistical analysis. Kaplan-Meier survival curves and
the log-rank test were utilized to analyze the survival rate of
patients, while the Cox regression model was used for the
multivariate analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
Clinical characteristics
In the same period of continuous treatment of 356
patients with SNIP, 8.99% (32/356) of patients exhibited the
malignant type. These 32 patients were selected for the
retrospective analysis and comprised 25 males and seven females,
with a male to female ratio of 3.6:1. The median age of onset was
56.5 years old. All 32 patients were diagnosed with pathologically
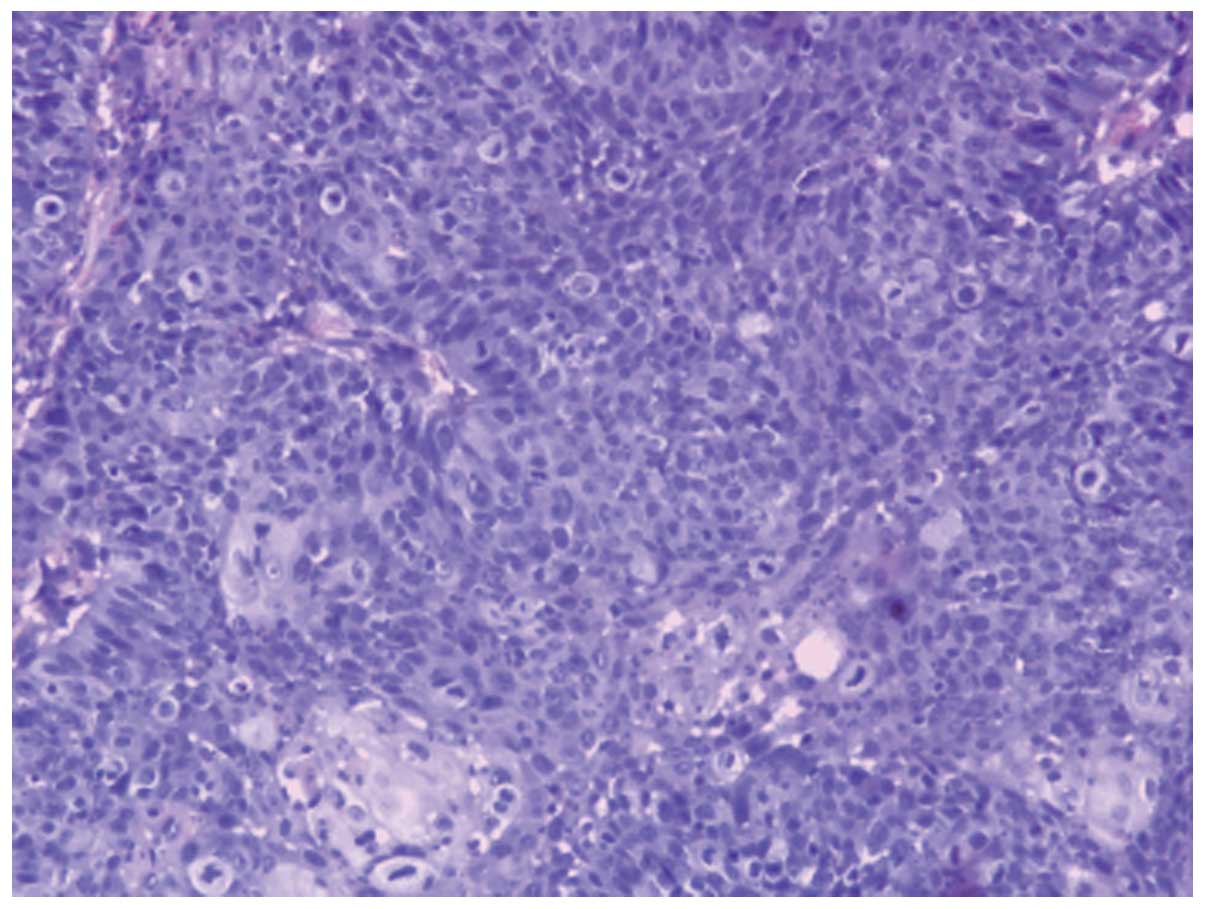
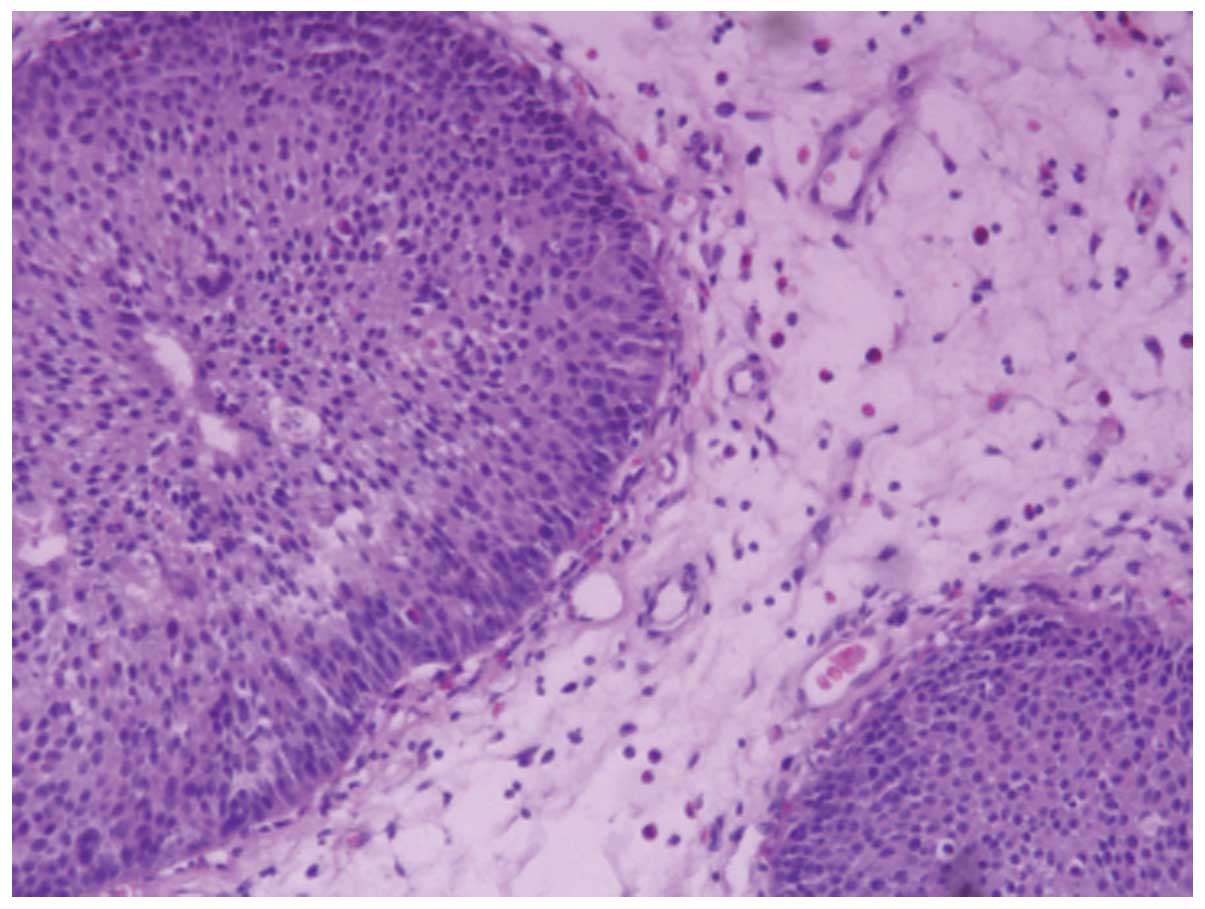
malignant SNIP that had progressed to SCC (Fig. 1). Nasal inverted papilloma was the
diagnosis in 18 patients, which included two cases of pathological
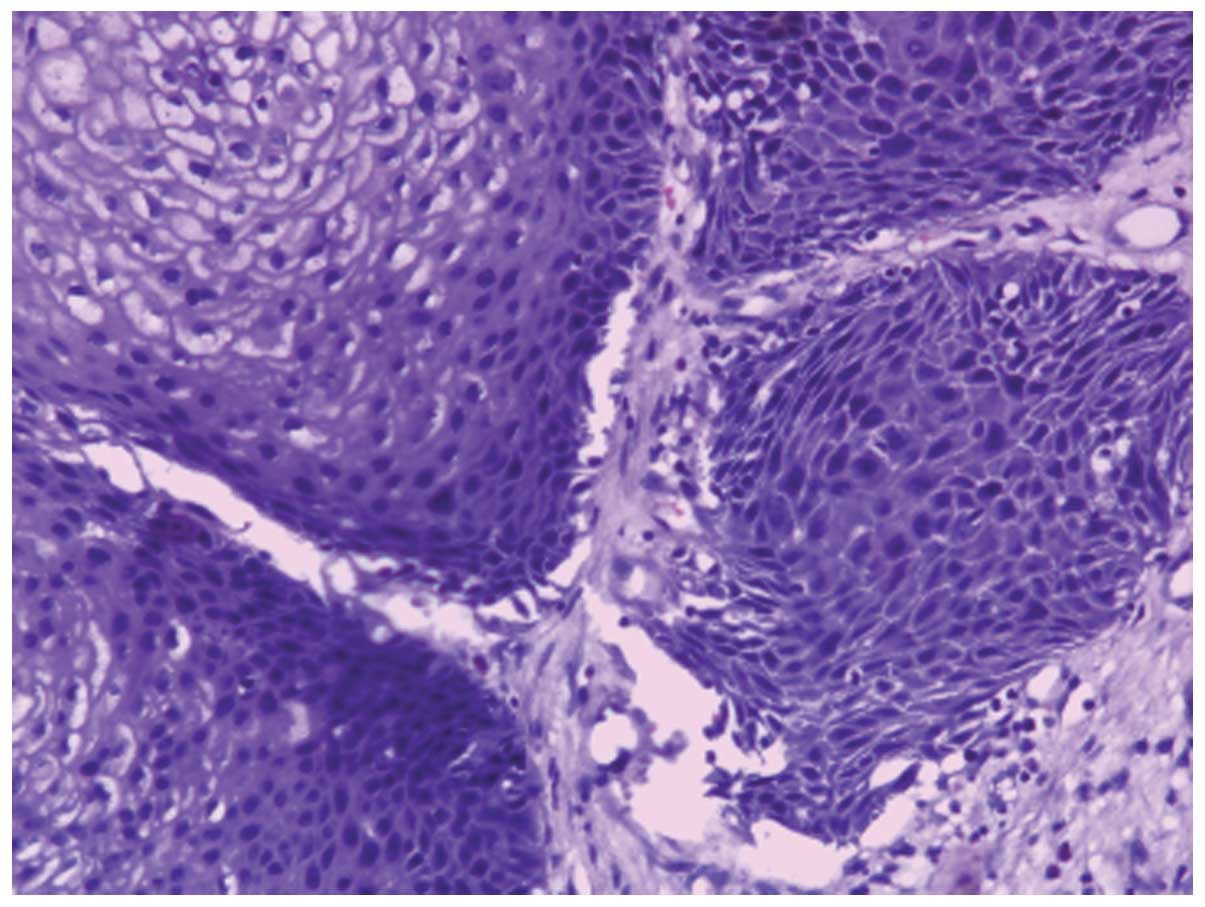
nasal inverted papilloma dysplasia (Fig. 2), and the remaining 16 cases were of
pathological nasal inverted papilloma with atypical hyperplasia
(Fig. 3). In the present study, the
corresponding incidence rates were 3.9% (14/356), and 5.1%
(18/356), respectively.
The site in which the tumor occurred was the
maxillary sinus in 10 cases, and the nasal cavity and sinus in 22
cases. The site had extended to the nasal sinuses or outside in 19
cases, which included 10 cases in the orbit, seven cases in the
skull and two cases in the pterygopalatine fossa. According to the
American Joint Committee on Cancer staging method (7), there were three cases of T1, 10 of T2,
16 of T3 and three of T4 (Table I).
Three patients had distant metastases, including two cases of
metastasis to the brain and one case of metastasis to the lung.
 | Table ILog-rank single-factor analysis for
survival patients. |
Table I
Log-rank single-factor analysis for
survival patients.
| Factor | Number of cases | 5-year survival rate
(%) | χ2
value | P-value |
|---|
| Gender | | | 1.875 | 0.285 |
| Male | 25 | 71.3 | | |
| Female | 7 | 73.3 | | |
| Age of onset
(years) | | | 0.237 | 0.567 |
| ≤60 | 15 | 74.2 | | |
| >60 | 17 | 62.8 | | |
| Diseased part | | | 0.365 | 0.512 |
| Nasal cavity and
sinus | 22 | 67.2 | | |
| Maxillary sinus | 10 | 73.0 | | |
| Pathological
grade | | | 0.056 | 0.728 |
| Poor and moderately
differentiated | 11 | 34.4 | | |
| Well
differentiated | 21 | 65.6 | | |
| Clinical stage | | | 9.782 | 0.002 |
| T1+T2 | 13 | 78.7 | | |
| T3+T4 | 19 | 47.9 | | |
| Orbital
violation | | | 8.765 | 0.005 |
| None | 22 | 72.8 | | |
| All | 10 | 50.8 | | |
| Skull base
violation | | | 5.231 | 0.009 |
| None | 25 | 70.1 | | |
| All | 7 | 45.5 | | |
| Treatment method | | | 7.565 | 0.006 |
| Comprehensive
treatment | 19 | 83.8 | | |
| Monotherapy | 13 | 40.7 | | |
| Malignancy grade | | | 0.436 | 0.486 |
| I+II | 10 | 73.2 | | |
| III+IV | 22 | 70.1 | | |
Among the 32 patients, 10 received surgery alone,
three received radiotherapy alone and 19 underwent both surgery and
radiotherapy (Table I). Surgical
treatment included endoscopic resection in eight cases, combined
endoscopic nasal surgery in 13 cases and simple nasal surgery in
eight cases.
For all patients, the follow-up period ranged from
23 to 212 months, and the median survival time was 74.8 months.
From the follow-up, it was concluded that of the 20 patients who
did not survive, nine cases were of uncontrolled local tumor (time
between end of treatment and recurrence, ≤3 months), eight cases
were of local tumor recurrence (time between end of treatment and
recurrence, >3 months) and three cases involved distant
metastasis.
Histological features
Among the 32 cases, 21 were well-differentiated,
eight were moderately differentiated and three were poorly
differentiated. According to the percentage of malignant areas
throughout the entire tumor tissue, tumor tissue sections were
divided into four stages: Five cases of grade I, five of grade II,
eight of grade III and 14 of grade IV (Table I).
Analysis of survival rate and prognostic
factors
The Kaplan-Meier method was used to calculate the
5-year survival rate of patients, which was determined to be 72.5%.
The median survival time was 62.2 months (Fig. 4A). The 5-year survival rate and
median survival time of patients who received comprehensive
treatment (both surgery and radiotherapy) were 83.8% and 64.2
months, respectively. However, the 5-year survival rate and median
survival time of patients who received a single treatment (either
surgery or radiotherapy) were 40.7% and 27.7 months (Fig. 4B). The difference in 5-year survival
rate and the median survival time between the two treatment groups
was statistically significant (P=0.006 and P=0.005,
respectively).
The effect of the following factors on survival was
then analyzed: Gender, age, clinical stage, disease site, orbital
violation, skull base violation, surgical treatment, the degree of
tumor cell differentiation and the proportion of malignant cells.
According to the Kaplan-Meier method analysis and the log-rank
test, the factors affecting patient survival were the clinical
stage (P=0.002), orbital violation (P=0.005), skull base violation
(P=0.009) and treatment method (P=0.006) (Table I). Additionally stages T3 and T4
(Fig. 4C), orbital violation, skull
base violation and monotherapy were associated with decreased
patient survival rates. However, gender, age, disease site, the
degree of tumor cell differentiation and the proportion of
malignant cells did not affect patient survival (Table I). Multivariate Cox regression
analysis showed that clinical stage (P=0.004) and treatment method
(P=0.032) were independent risk factors for survival (Table II).
 | Table IICox regression multivariate
analysis. |
Table II
Cox regression multivariate
analysis.
| Factor | Partial regression
coefficient | Standard error | Wald
χ2 | DOF | P-value | RR | 95% CI |
|---|
| Gender | 1.231 | 0.236 | 0.030 | 1 | 0.924 | 0.924 | 0.942–8.901 |
| Age | 1.632 | 0.430 | 0.121 | 1 | 0.760 | 1.211 | 0.672–7.099 |
| Diseased part | 1.152 | 0.260 | 2.451 | 1 | 0.248 | 0.912 | 0.661–6.351 |
| Pathological
grade | 0.532 | 0.277 | 1.454 | 1 | 0.432 | 0.852 | 0.872–4.554 |
| Clinical stage | 1.452 | 0.512 | 8.400 | 1 | 0.004 | 4.211 | 1.512–11.321 |
| Orbital
violation | 1.532 | 0.470 | 2.701 | 1 | 0.105 | 3.321 | 1.472–7.211 |
| Skull base
violation | 0.866 | 0.596 | 2.876 | 1 | 0.096 | 3.433 | 1.855–6.462 |
| Treatment method | −1.182 | 0.526 | 4.387 | 1 | 0.032 | 0.312 | 0.121–0.922 |
| Malignancy grade | 1.455 | 1.198 | 1.697 | 1 | 0.291 | 1.122 | 0.635–6.251 |
Discussion
Currently, the specific mechamisms underlying SNIP
malignancy remain unclear. From the perspective of pathogenesis,
SNIPs are borderline tumors, and they can undergo malignant
transformation with disease progression. Most commonly, SNIP
malignancy is associated with SCC, followed by malignant
adenocarcinoma, while small cell carcinoma is rarely seen in the
clinic (8). SCC that originates
from the papilloma often has a high level of differentiation, and
the prognosis of which is improved compared with simple primary
SCC. Even in the late stages of the disease, lymph node metastases
are rare (3,4). All pathological types within the 32
patients of malignant transformation of SNIP were SCC, well
differentiated SCC accounted for 65.6% (21/32) of the malignant
cases. Zhangzong et al (9)
analyzed the clinical data of 146 cases of primary SCC of the nasal
sinus and the overall 5-year survival rate was 49.1%. In the
present study, the overall survival rate of the 32 patients with
malignant SNIP was 72.5%. Therefore, from this data, the prognosis
of patients with malignant SNIP appears to be improved compared
with that of patients with primary SCC.
There are two main ways in which SNIPs may become
malignant: The SNIP and malignancy may occur in the same lesion, or
the malignancy may occur in the site from which an SNIP was
previously resected (6). Mirza
et al (10) followed up 65
patients for 20 years and reported that the incidence rate of SCC
occurring simultaneously with inverted papilloma was 7.1%, while
the incidence rate of SCC occurring independently of the papilloma
was 3.6%. In the present study, the corresponding incidence rates
were 3.9% (14/356), and 5.1% (18/356), respectively.
In this study, the incidence of malignancy among
SNIP cases was 8.99% SNIP (32/356), and this was similar to that
reported in the literature, which reported that the incidence of
malignancy among SNIP cases was 11% (3,11). The
number of males with malignant SNIP was greater than the
corresponding number of females (3.6:1), and the median age of
onset for malignant cases was 56.5 years. There was no significant
difference in the 5-year survival rate between patients with early
(≤60 years) and late (>60 years) onset of disease. In the
present study cohort, gender and age were not significant factors
affecting the prognosis of patients with malignant SNIP (P=0.285
and P=0.567, respectively).
Sinus computed tomography scan and brain magnetic
resonance imaging can show the range of tumor tissue types
preoperatively, and may aid in the clinical classification of the
tumor and the corresponding preoperative preparation. Preoperative
biopsy is an ineffective method of identifying malignant SNIP and
SNIPs mostly become malignant from the center; therefore, multiple
preoperative biopsies should be obtained from different locations
in the tumor tissue, particularly near the base of the central area
of tumor, so as to prevent misdiagnosis (2,3). In
the current study, 27 out of the 32 patients were diagnosed with
concomitant SNIP and SCC, or SCC in situ by preoperative
biopsy. The remaining five cases were diagnosed with SNIP or severe
dysplasia, pathologically confirmed as SCC, by preoperative
biopsy.
The results of this study showed that the main
factors affecting the prognosis of patients with malignant SNIP
were clinical stage and treatment method. Due to the malignant
SNIP, such patients often have a long history of illness and
repeated surgery, and the tumor invades an extensive range. As the
sinonasal cavity is proximal to the important organizational base
of the skull, en bloc resection of the tumor is difficult to
perform safely, and chemotherapy should be administered for local
control following surgery (12). In
the present study of 32 patients, orbit and skull base invasion of
the tumor were identified in 10 and seven cases, and the 5-year
survival rates were 50.8 and 45.5% (64.2 vs. 27.7 months; P=0.006),
respectively, suggesting a poor prognosis.
With the development of endoscopic surgical
techniques for the treatment of malignant SNIP, the traditional
method of open surgical procedures has been replaced by minimally
invasive endoscopic surgery or endoscopic-assisted surgery combined
with chemotherapy, improving survival rates (?). Surgery plus
postoperative radiotherapy and chemotherapy has been found to be
the most effective treatment (6,13). In
the present study, the 19 patients who received surgery plus
postoperative radiotherapy had a significantly improved 5-year
survival rate (83.8%) compared with that of the remaining 13
patients who received monotherapy (either surgery or radiotherapy)
(83.8 vs 40.7%; P=0.006). The median survival time was also
significantly improved in the patients receiving comprehensive
treatment compared with that in the patients receiving monotherapy
(64.2 vs. 27.7 months; P=0.006). We conclude that complete removal
of the tumor, to ensure negative margins and facilitate thorough
histological examination, supplemented with postoperative
radiotherapy, can improve the prognosis of malignant SNP.
SNIP has a low incidence of malignancy, a lack of
specific clinical manifestations and biological indicators;
currently, identification of SNIP mainly relies on the pathological
diagnosis. In the present study, clinical stage and treatment
modality were independent risk factors for prognosis. We propose
that the primary treatment modality for malignant SNIP should
comprise surgical excision with postoperative radiotherapy and
chemotherapy. In further studies, a comphrensive analysis of
patient clinical stage, treatment and other risk factors must be
performed to improve patient survival rates.
Acknowledgements
This study is based on a study first reported in the
Chinese Journal of Otorhinolaryngology Head and Neck Surgery.
References
|
1
|
Sauter A, Matharu R, Hörmann K, et al:
Current advances in the basic research and clinical management of
sinonasal inverted papilloma (review). Oncol Rep. 17:495–504.
2007.
|
|
2
|
Lawson W, Kaufman MR and Biller HF:
Treatment outcomes in the management of inverted papilloma: an
analysis of 160 cases. Laryngoscope. 113:1548–1556. 2003.
|
|
3
|
von Buchwald C and Bradley PJ: Risks of
malignancy in inverted papilloma of the nose and paranasal sinuses.
Curr Opin Otolaryngol Head Neck Surg. 15:95–98. 2007.
|
|
4
|
Yuan H and Wang RG: Management of
sinonasal inverting papilloma with recurrence and malignant
transformation. Zhong Hua Er Bi Yan Hou Ke Za Zhi. 3:45–48.
2002.(In Chinese).
|
|
5
|
Benninger MS, Roberts JK, Sebek BA, et al:
Inverted papillomas and associated squamous cell carcinomas.
Otolaryngol Head Neck Surg. 103:457–461. 1990.
|
|
6
|
Choi JW, Kim SG, Kim YM, et al: Clinical
and histologic features of inverted papilloma-associated
malignancy. Eur Arch Otorhinolaryngol. 269:2349–2354. 2012.
|
|
7
|
Edge SB and Compton CC: The American Joint
Committee on Cancer: the 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474.
2010.
|
|
8
|
Katori H, Nozawa A and Tsukuda M:
Histopathological parameters of recurrence and malignant
transformation in sinonasal inverted papilloma. Acta Otolaryngol.
126:241–218. 2006.
|
|
9
|
Min Zhangzong, Pingzhang Tang, Gang
Xuzhen, et al: Nasal sinus treatment of 146 cases of squamous cell
carcinoma of the analysis. Chinese Journal of Otorhinolaryngology
Head and Neck Surgery. 45:555–559. 2010.
|
|
10
|
Mirza S, Bradley PJ, Acharya A, et al:
Sinonasal inverted papillomas: recurrence, and synchronous and
metachronous malignancy. J Larygol Otol. 121:857–864. 2007.
|
|
11
|
Tanvetyanon T, Qin D, Padhya T, et al:
Survival outcomes of squamous cell carcinoma arising from sinonasal
inverted papilloma: report of 6 cases with systematic review and
pooled analysis. Am J Otolaryngol. 30:38–43. 2009.
|
|
12
|
Hug EB, Wang CC, Montgomery WW and Goodman
ML: Management of inverted papilloma of the nasal cavity and
paranasal sinuses: importance of radiation therapy. Int J Radiat
Oncol Biol Phys. 26:67–72. 1993.
|
|
13
|
Sun WY, Zhao N, Zhai RH, et al: Endoscopic
surgery and endoscopy-assisted surgery for the malignant
transformation of sinonasal inverted papilloma. Zhonghua Er Bi Yan
Hou Tou Jing Wai Ke Za Zhi. 46:1036–1039. 2011.(In Chinese).
|