Introduction
Osteoma is a rare but benign tumor, which is caused
by abnormal growth of bone or excessive proliferation of other
tissues. Microscopically, osteoma consists of compact and spongy
bone. Osteoma exhibits continuous growth during childhood rather
than exhibiting growth cessation during adulthood. This is the
major feature that distinguishes osteoma from other bony exostosis,
including tori (1–4). During their slow and steady increase
in size, osteomas remains asymptomatic until they reach a size that
is sufficient to cause disfigurement and/or direct interference
with the normal function of its anatomical location. Excision of
osteoma is often unnecessary, however, surgery is required in the
presence of apparent symptoms.
Various theories have been suggested to explain the
pathological mechanism of osteoma. For example, these lesions have
been associated with the abnormal enlargement of the fetal
periosteum or residual cartilage, reactive lesions due to trauma,
muscle traction and infection, as well as true neoplasms. However,
a specific cause-effect association is difficult to establish
(5–7).
In this study, a case of a patient with bone marrow
osteoma located in tibia who underwent surgical excision of the
lesion is presented. This study was approved by the ethics
committee of Guangzhou General Hospital of Guangzhou Military
Command (Guangzhou, China) and written informed consent was
obtained from the patient’s family.
Case report
An eight-year-old male was referred to the 458th
Hospital of PLA (Guangzhou, China). The patient had complained of
discontinuous discomfort in the right distal calf for six months.
The discomfort worsened at night and was not improved by aspirin
administration. Physical examination was normal with the exception
of a pressing pain at the distal calf. Plain radiographies showed
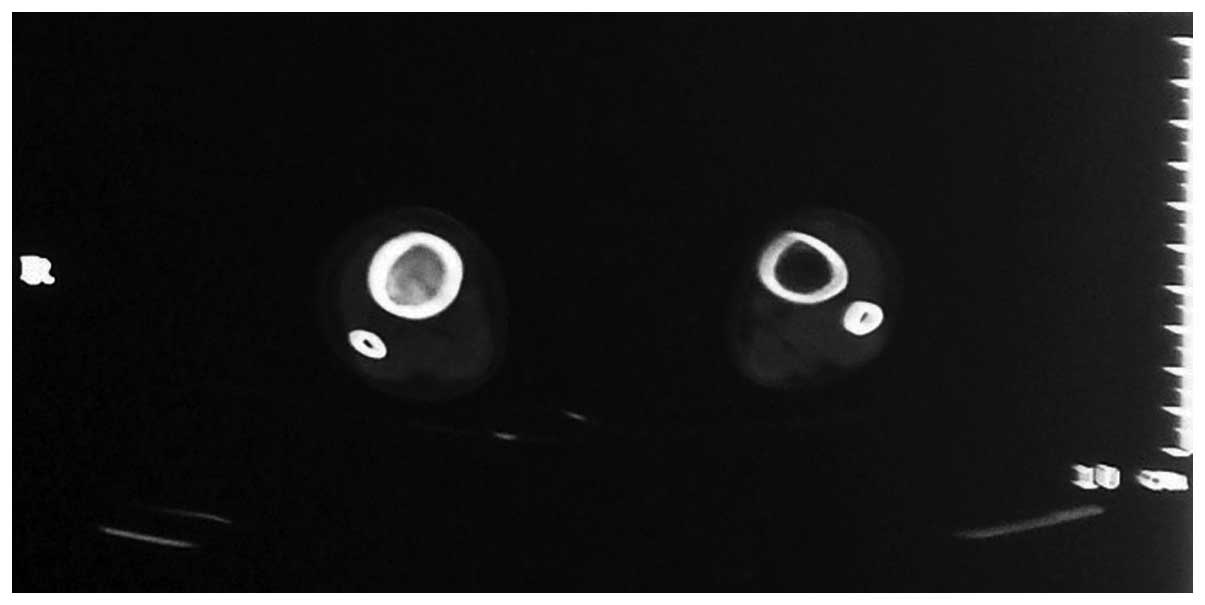
increased bony density in the distal tibia (Fig. 1). Computed tomography (CT) scans of
the distal tibia revealed that medullary cavity was narrow and
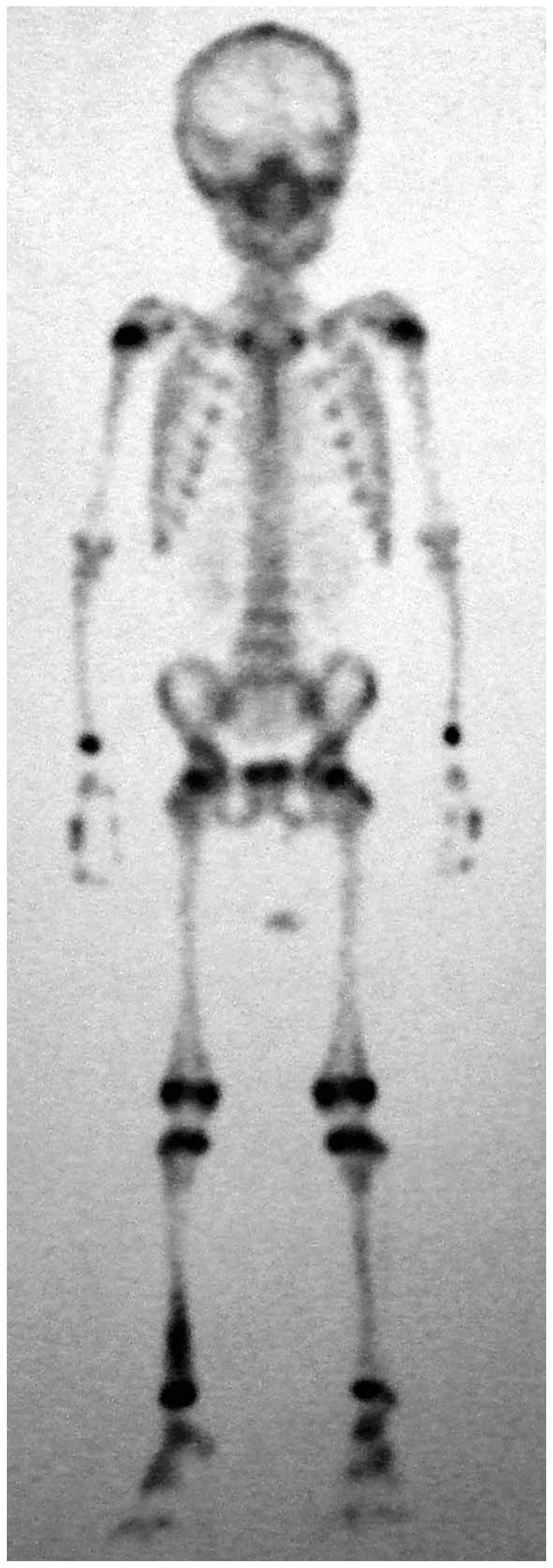
packed with high-density osteoid tissue (Fig. 2). A technetium-99m bone scan showed
focally increased uptake in the same region (Fig. 3). Collectively, these observations
indicated that the patient may have suffered from bone disease.
The patient subsequently underwent surgical excision
of the lesion. The lesion size was measured according to the
preoperative X-ray and CT results. The lesion site with an 3 cm
diameter, marginally larger than the preoperative measurements, was
opened at the middle of tibia cortex. Surgical findings revealed a
hard bone substance that had formed in the medullary cavity. A
small section of diseased tissue was subsequently subjected to
intraoperative frozen sectioning for pathological examination. The
examination results indicated the presence of a benign tumor. The
lesion was then completely removed using a spatula and power drill.
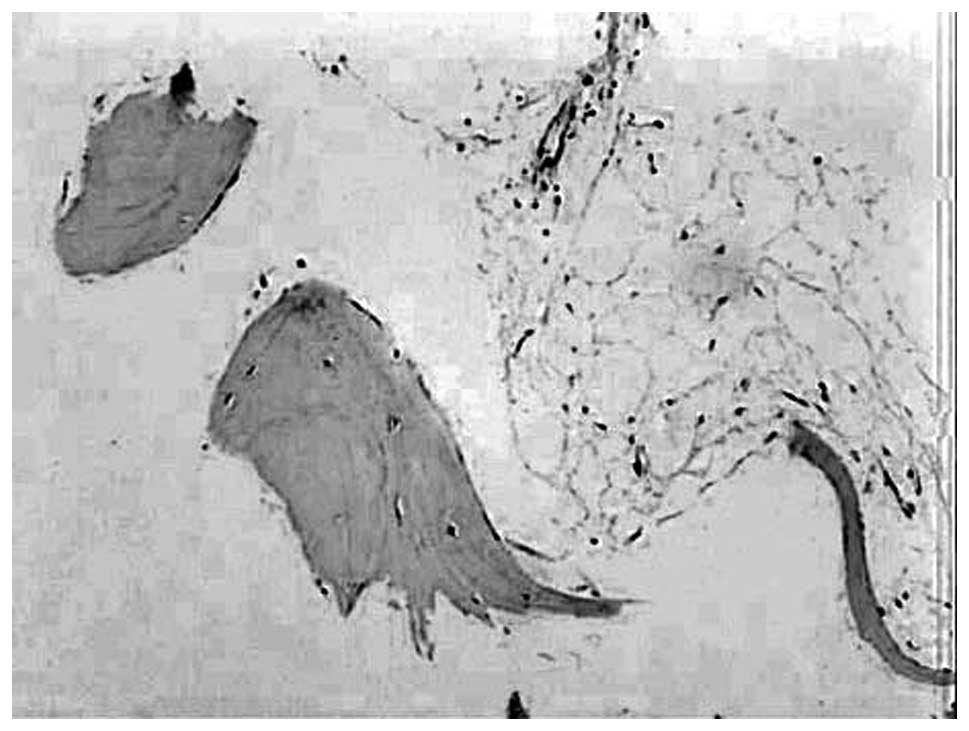
Histological examination revealed that the excised mass was a bone
marrow osteoma. (Fig. 4). Following
surgery, the symptoms were eradicated. The patient was followed up
for 24 months without any recurrence.
Discussion
Osteoma often occurs in the skull and facial bones,
however, it may also occur in the limbs and other body parts. Based
on its location, osteoma is divided into peripheral, central and
extraskeletal osteomas. Peripheral osteomas arise from the cortical
plate, whereas central osteomas develop as masses on endosteal bone
surfaces and extraskeletal osteomas have rarely been reported
(8,9). Osteoma in the bone marrow cavity is
termed bone marrow osteoma. Various studies have reported that
osteomas may exist in multiple unusual regions, including the
acoustic meatus (10), middle ear
ossicles (11) and false vocal
folds (12). Notably, whether
osteoma may occur in the bone marrow remains unclear, however, this
study presented the case of a patient with bone marrow osteoma
located in the tibia that underwent surgical excision of the
lesion.
The primary differential diagnosis includes other
radiopaque masses, including osteoblastoma, osteoid osteoma,
fibro-osseous lesions, cementoblastoma, osteosarcoma, exostosis,
complex odontoma, sessile osteochondroma and end-stage
osteomyelitis (13,14).
Patients with osteoblastoma or osteoid osteoma
usually exhibit a medical history of pain, a characteristic
clinical symptom, which is not often directly associated with
osteomas. Furthermore, the pain caused by an osteoid osteoma is
distinguished symptomatically from osteoma and osteoblastoma by the
presence of a history of pain ameliorated by non-steroidal
anti-inflammatory drugs. In addition, osteoblastomas and osteoid
osteomas grow more rapidly than osteomas (15). Radiographical features of an
osteoblastoma or osteoid osteoma generally exhibit a round or oval
well-delineated radiolucent defect. However, an osteoma exhibits a
round or oval well-circumscribed radiopaque mass with a broad base
(16). An osteoid osteoma is
further distinguished radiographically from osteomas and
osteoblastoma in the presence of a distinct rim of sclerosis, as
well as an identifiable radiopaque nidus (16). Microscopically, osteoblastoma and
osteoid osteoma exhibit abundant osteoid trabeculae anastomosing in
a loose fibrovascular connective stroma. The osteoid trabeculae in
osteoblastoma and osteoid osteoma usually exhibits prominent
osteoblastic rimming and a characteristic basophilic appearance.
Osteoclastic giant cells are also often present in osteoblastoma
and osteoid osteoma in addition to extravasated red cells, however,
these latter features are absent in osteomas (17). By contrast, osteoma resembles normal
compact or cancellous bone with variable amounts of fibrofatty bone
marrow.
The clinical symptom of fibro-osseous lesions is
painless swelling, which is similar to osteoma. On radiological
examination, early fibro-osseous lesions are radiolucent, however,
as they progress they appear as ill-defined ground-glass
opacifications. In addition, for the majority of fibro-osseous
lesions, growth is stabilized or restrained following the growth
period, which allows them to be distinguished from osteoma
(18).
Cementoblastoma may be excluded as an option if the
lesion is not connected to the tooth at the time of diagnosis
(19). Osteosarcomas grow rapidly
and exhibit high recurrence rates, occurring preferentially in
young adults aged between 10 and 20 years old, and the serum
alkaline phosphatase level is elevated (20).
Exostosis is a hamartoma that grows in specific
areas, including the lingual and buccal regions of the mandible,
midline of hard palate, and buccal and hard palate regions of the
maxilla, and growth stops following puberty (21). A peripheral osteoma may be
differentiated from an exostosis in accordance with an accurate
medical history and clinical features, however, no histological
differences have been identified (22). Exostosis occurs more commonly than
osteoma. It is a bony growth in the lingual plate of the maxillary
bones, which is usually symmetrical, well circumscribed and
associated with inflammatory or traumatic phenomena. An exostosis
usually stops growing following puberty, whereas osteomas exhibit
independent growth (22,23).
Complex odontoma is a clearly circumscribed
radiopaque mass, with a density greater than that of bone, and it
is surrounded by a narrow radiolucent rim (24). In sessile osteochondroma, the cortex
of the lesion merges imperceptibly with the cortex of the host bone
(25).
This case of bone marrow osteoma identified in the
distal tibia provides an example of atypical presentation.
Successful diagnosis and differential diagnosis may be obtained
through clinical appearance, plain radiography, CT scan, emission
computed tomography and histopathological examination. In
conclusion, a diagnosis of bone marrow osteoma should be considered
when a patient exhibits discontinuous and unexplained limb
discomfort.
References
|
1
|
Cutilli BJ and Quinn PD: Traumatically
induced peripheral osteoma. Report of a case. Oral Surg Oral Med
Oral Pathol. 73:667–669. 1992.
|
|
2
|
Richards HE, Strider JW Jr, Short SG,
Theisen FC and Larson WJ: Large peripheral osteoma arising from the
genial tubercle area. Oral Surg Oral Med Oral Pathol. 61:268–271.
1986.
|
|
3
|
Seward MH: An Osteoma of the Maxilla. Br
Dent J. 118:27–30. 1965.
|
|
4
|
Swanson KS, Guttu RL and Miller ME:
Gigantic osteoma of the mandible: report of a case. J Oral
Maxillofac Surg. 50:635–638. 1992.
|
|
5
|
Larrea-Oyarbide N, Valmaseda-Castellón E,
Berini-Aytés L and Gay-Escoda C: Osteomas of the craniofacial
region. Review of 106 cases. J Oral Pathol Med. 37:38–42. 2008.
|
|
6
|
Johann AC, de Freitas JB, de Aguiar MC, de
Araújo NS and Mesquita RA: Peripheral osteoma of the mandible: case
report and review of the literature. J Craniomaxillofac Surg.
33:276–281. 2005.
|
|
7
|
Rodriguez Y, Baena R, Rizzo S, Fiandrino
G, Lupi S and Galioto S: Mandibular traumatic peripheral osteoma: a
case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
112:e44–e48. 2011.
|
|
8
|
Kaplan I, Calderon S and Buchner A:
Peripheral osteoma of the mandible: a study of 10 new cases and
analysis of the literature. J Oral Maxillofac Surg. 52:467–470.
1994.
|
|
9
|
Woldenberg Y, Nash M and Bodner L:
Peripheral osteoma of the maxillofacial region. Diagnosis and
management: a study of 14 cases. Med Oral Patol Oral Cir Bucal.
10(Suppl 2): E139–E142. 2005.
|
|
10
|
Kovacić J, Subarić M, Lajtman Z and Curcić
I: Osteoma of the internal auditory canal. Acta Med Croatica.
55:215–218. 2001.
|
|
11
|
Sente M and Topolac R: Osteomas of the
middle ear. Med Pregl. 57:181–185. 2004.(In Serbian).
|
|
12
|
Angelillo M, Mazzone S, Costa G, Mazzone A
and Barillari U: The first case of osteoma in the false vocal fold.
Auris Nasus Larynx. 36:235–238. 2009.
|
|
13
|
Han SH, Kwon H and Jung SN: Peripheral
osteoma on the buccal aspect of mandible angle: a review of
radiopaque masses and differential diagnosis. J Craniofac Surg.
24:1842–1844. 2013.
|
|
14
|
Seidl T, Maier M, Refior HJ and Veihelmann
A: Chronic recurrent multifocal osteomyelitis. Orthopade.
32:535–540. 2003.(In German).
|
|
15
|
Sayan NB, Uçok C, Karasu HA and Günhan O:
Peripheral osteoma of the oral and maxillofacial region: a study of
35 new cases. J Oral Maxillofac Surg. 60:1299–1301. 2002.
|
|
16
|
Oner AY and Pocan S: Gardner’s syndrome: a
case report. Br Dent J. 200:666–667. 2006.
|
|
17
|
Ogbureke KU, Nashed MN and Ayoub AF: Huge
peripheral osteoma of the mandible: a case report and review of the
literature. Pathol Res Pract. 203:185–188. 2007.
|
|
18
|
Waldron CA: Fibro-osseous lesions of the
jaws. J Oral Maxillofac Surg. 51:828–835. 1993.
|
|
19
|
Hirai E, Yamamoto K, Kounoe T, Kondo Y,
Yonemasu H and Kurokawa H: Benign cementoblastoma of the anterior
maxilla. J Oral Maxillofac Surg. 68:671–674. 2010.
|
|
20
|
Wang GD, Zhao YF, Liu Y, Jiang L and Jiang
XZ: Periosteal osteosarcoma of the mandible: case report and review
of the literature. J Oral Maxillofac Surg. 69:1831–1835. 2011.
|
|
21
|
Zavaros G and Ujpál M: Symmetrical
exostosis on the mandible. Fogorv Sz. 90:273–275. 1997.(In
Hungarian).
|
|
22
|
Del Vecchio A, Agrestini C, Salucci P,
Manicone AM and Della Rocca C: Osteomas and exostoses of the facial
structures: a morphological study and the etiopathogenetic
considerations. Minerva Stomatol. 42:533–540. 1993.(In
Italian).
|
|
23
|
DelBalso AM and Werning JT: The role of
computed tomography in the evaluation of cemento-osseous lesions.
Oral Surg Oral Med Oral Pathol. 62:354–357. 1986.
|
|
24
|
Litonjua LA, Suresh L, Valderrama LS and
Neiders ME: Erupted complex odontoma: a case report and literature
review. Gen Dent. 52:248–251. 2004.
|
|
25
|
Zhang J, Wang H, Li X, et al:
Osteochondromas of the mandibular condyle: variance in radiographic
appearance on panoramic radiographs. Dentomaxillofac Radiol.
37:154–160. 2008.
|