Introduction
Hemangiopericytoma is a rare perivascular tumor in
which uncontrolled proliferation of pericytes occurs, which often
involves the extremities, pelvis, head and neck, and meninges, but
rarely occurs in the kidney; renal hemangiopericytoma has been
reported in ≤50 cases since the initial case was reported by Black
and Heinemann in 1955 (1). The
majority of cases have been identified in patients between 20 and
50 years of age, and a considerable proportion of patients present
with hypertension, hypoglycaemia or additional paraneoplastic
syndromes (2). Due to the rarity of
the tumor, the exact diagnosis, effective treatment and prognosis
of the tumor remain unclear. The current study reports a rare case
of hemangiopericytoma with drug refractory hypertension in a
14-year-old female. Written informed consent was obtained from the
patient’s family.
Case report
A 14-year-old female was admitted to Huashan
Hospital, Fudan University (Shanghai, China) with intermittent
dizziness and vomiting for the previous three months. The patient
exhibited hypertension, with a blood pressure of 200/140 mmHg.
However, the blood pressure continued to fluctuate above 150/100
mmHg following treatment with losartan, nifedipine and aldactone
for over six weeks. The levels of renin (1.5 μg/l/h; normal range,
1.0–2.5 μg/l/h) and angiotensin (22 ng/l; normal range, 10–30 ng/l)
were not increased, and the serum creatinine (56 μmol/l; normal
range, 44–133 μmol/l), sodium (139 mmol/l; normal range, 135–147
mmol/l) and potassium (4.1 mmol/l; normal range, 3.5–5.5 mmol/l)
levels, together with C-reactive protein (0.74 mg/l; normal range,
0–3.25 mg/l) levels and erythrocyte sedimentation rate (13 mm/h;
normal range, 0–20 mm/h), were also within normal ranges. Abdominal
ultrasonography revealed an isoechoic solid lesion of 3.5 cm in
diameter in the center of the right kidney, and computed tomography
also showed a mass with abnormal density, particularly in the
arterial and venous phase (Fig. 1).
No tumor infiltration was identified in the renal collecting
system, vessels and perirenal tissue, as well as retroperitoneal
lymph nodes.
Partial nephrectomy with an open, lumbotomic
approach was implemented for this renal lesion with unknown
characteristics. An exophytic and clear, circumscribed tumor was
excised completely. The specimen was 3.5 cm in diameter, and a
homogeneous texture without necrosis or cystic separation was
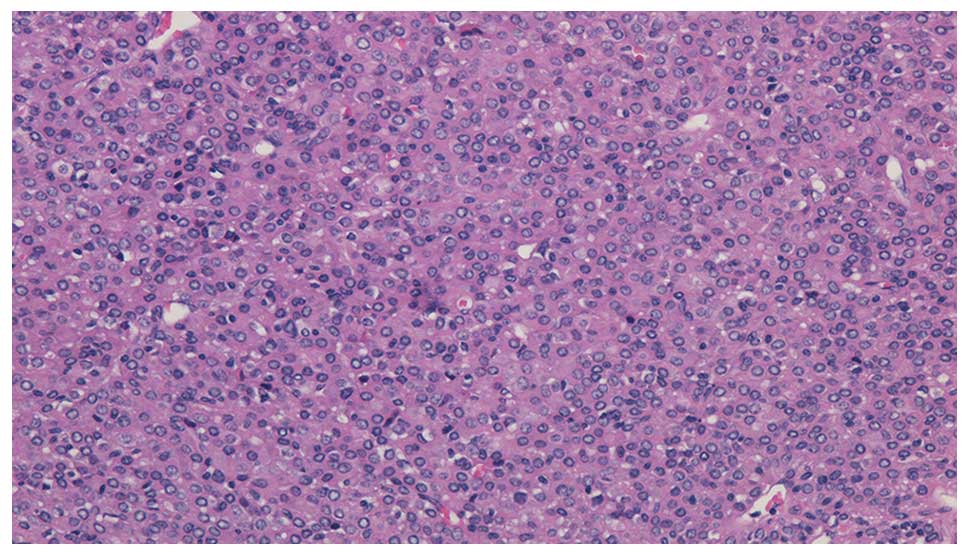
visible on gross examination. On microscopic examination,
monotonous proliferation with no significant variability and
pericytes around the endothelial vascular channels were the
characteristic features, which indicated renal hemangiopericytoma
(Fig, 2). The positive results of
vimentin, Bcl-2 and CD34 by immunohistochemical staining also
supported this diagnosis (Fig.
3).
The duration of hospitalization was six days and no
perioperative complications were observed during that time. After a
follow-up of 12 months, the patient remains well with no evidence
of recurrence or metastasis; the blood pressure has returned to
within the normal range (115/70 mmHg) and no antihypertensive drugs
are in use.
Discussion
Hemangiopericytoma is a rare vascular tumor of the
soft tissue originating from pericytes and was initially described
by Zimmermann in 1923 (3). It has
been demonstrated to be a monotonous cellular proliferation with no
significant variability, and exhibits pericytes around endothelial
vascular channels with collagenization. Immunohistochemical
analysis provides substantial information as positive reactions for
antibodies including CD34 and vimentin are characteristic of cells
of mesenchymal origin and thus, they are widely used to identify
neoplastic progenitor cells surrounding vascular spaces (4). A combination of histological and
immunohistochemical patterns may provide an exact diagnosis.
Previous studies have found that the mean age of
patients at the time of diagnosis and surgery is 40 years (2). In the pressent study, the patient was
14 years old and thus, at present this is the youngest patient
reported. The age distribution indicates that renal
hemangiopericytoma often affects younger patients.
It is difficult to differentiate renal
hemangiopericytoma from RCC using current imaging technology
(2). By contrast to other tumors,
numerous patients present with paraneoplastic syndromes, including
hypertension, hypoglycemia, electrolyte disorders and cachexia
(2). Hypertension is the most
common symptom, however, its association with renal
hemangiopericytoma remains unclear. Robertson et al
(5) hypothesized that it is a
result of the renin produced by the tumor (5). However, in the present case the
patients did not present with a high level of renin. Patients with
juxtaglomerular cell tumors often present hypertension, which is
due to the secretion of renin. Juxtaglomerular cell tumors, also
termed reninoma, are tumors of the renal juxtaglomerular cell
apparatus, which causes hypertension and hypokalemia due to the
hypersecretion of renin (6). The
diagnosis of hemangiopericytoma is usually the result of excluding
the possibility of other vascular and mesenchymal tumors, according
to the histological pattern and the immunohistochemical results
(2). Although this tumor may also
present with hypertension, it is considered to have a different
origin from that of hemangiopericytoma (2).
Although radiotherapy and other modalities may be
performed (7), surgery is
considered the most effective treatment, and has been performed in
every case reported (2). Renal
hemangiopericytoma usually grows insidiously without evident
symptoms, and the majority patients receive radical nephrectomy
(2). As aforementioned, this tumor
is not easily differentiated from RCC, and thus all surgical
procedures must comply with those of RCC. Partial nephrectomy is
recommended, when feasible during surgery, as it may provide
improved renal function and oncological outcomes, when compared
with radical nephrectomy (8,9).
Therefore, patients with renal hemangiopericytoma may experience a
longer disease-free or progression-free survival following surgery
and hypertension associated with the tumor may also recover
(5,10,11).
In conclusion, renal hemangiopericytoma is a rare
perivascular tumor and patients may present with hypertension or
other paraneoplastic syndromes. The results of the present case
indicated that surgery provides satisfactory outcomes for patients
with renal hemangiopericytoma and it appears to be the most
effective modality of treatment for the disease. Furthermore, this
case demonstrated that secondary hypertension may also recover
following surgery.
References
|
1
|
Black HR and Heinemann S:
Hemangiopericytoma: report of a case involving the kidney. J Urol.
74:42–46. 1955.
|
|
2
|
Argyropoulos A, Liakatas I and Lykourinas
M: Renal haemangiopericytoma: the characteristics of a rare tumour.
BJU Int. 95:943–947. 2005.
|
|
3
|
Brescia A, Pinto F, Gardi M, Maria Vecchio
F and Bassi PF: Renal hemangiopericytoma: case report and review of
the literature. Urology. 71:e9–e12. 2008.
|
|
4
|
Zimmermann KW: Der Feinere Bau der Blut
capillaren. Z Anat Entwicklungsgesch. 68:29–109. 1923.
|
|
5
|
Robertson PW, Klidjian A, Harding LK, et
al: Hypertension due to a renin-secreting renal tumor. Am J Med.
43:963–976. 1967.
|
|
6
|
Wong L, Hsu TH, Perlroth MG, Hofmann LV,
Haynes CM and Katznelson L: Reninoma: case report and literature
review. J Hypertens. 26:368–373. 2008.
|
|
7
|
Farrow GM, Harrison EG Jr, Utz DC and
Jones DR: Renal angiomyolipoma. A clinicopathologic study of 32
cases. Cancer. 22:564–570. 1968.
|
|
8
|
Becker F, Siemer S, Humke U, Hack M,
Ziegler M and Stöckle M: Elective nephron sparing surgery should
become standard treatment for small unilateral renal cell
carcinoma: Long-term survival data of 216 patients. Eur Urol.
49:308–313. 2006.
|
|
9
|
Huang WC, Elkin EB, Levey AS, Jang TL and
Russo P: Partial nephrectomy versus radical nephrectomy in patients
with small renal tumors - is there a difference in mortality and
cardiovascular outcomes? J Urol. 181:55–61. 2009.
|
|
10
|
Duprez D, De Smet H, Roels H and Clement
D: Hypertension due to renal renin-secreting tumour. J Hum
Hypertens. 4:59–61. 1990.
|
|
11
|
Sasaki H, Tozuka K, Tanaka O, et al: A
case of renal hemangiopericytoma. Nippon Hinyokika Gakkai Zasshi.
83:2090–2093. 1992.(In Japanese).
|