Introduction
Schwannomas or neurilemmomas are rare neoplasms that
typically occur in the peripheral nerve sheath of the extremities.
However, visceral localization of these tumors, specifically
pancreatic schwannomas that arise from either sympathetic or
parasympathetic fibers of the pancreas, is particularly rare
(1). Pancreatic schwannomas affect
adults with an equal gender distribution. In the majority of cases,
these tumors are well-defined, encapsulated solid masses with
hemorrhage or cystic degeneration, calcification, hyalinization and
xanthomatous infiltration (1–3).
Imaging findings of pancreatic schwannomas with cystic degeneration
may present a cystic pancreatic lesion. The present study reports a
patient with a pancreatic head tumor presenting with weight loss
and abdominal pain. The pancreatic head tumor was diagnosed as a
schwannoma, which was considered to be a rare case with an unusual
localization. The patient provided written informed consent.
Case report
A 30-year-old male was admitted to the Ankara
Oncology Research and Education Hospital (Ankara, Turkey)
presenting with weight loss and abdominal pain. The patient
exhibited no other systemic symptoms. On physical examination, a
tender mass in the epigastrium was palpated. The laboratory
examination results, including hemoglobin, liver function tests,
amylase and tumor marker levels (carbohydrate antigen 19-9 and
carcinoembryonic antigen) were in the normal ranges.
Abdominal ultrasonography revealed a hypoechoic mass
measuring 7.6×3 cm in the pancreatic head. Upper abdominal computed
tomography (CT) showed a hypodense mass measuring 10×7 cm arising
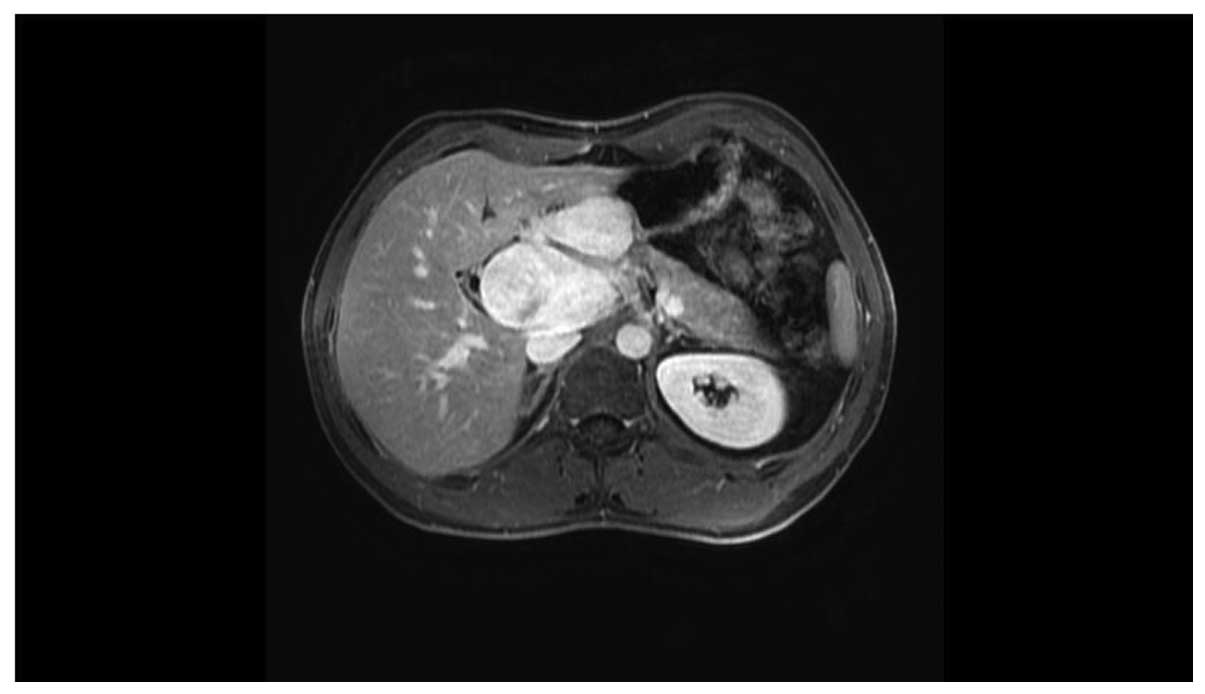
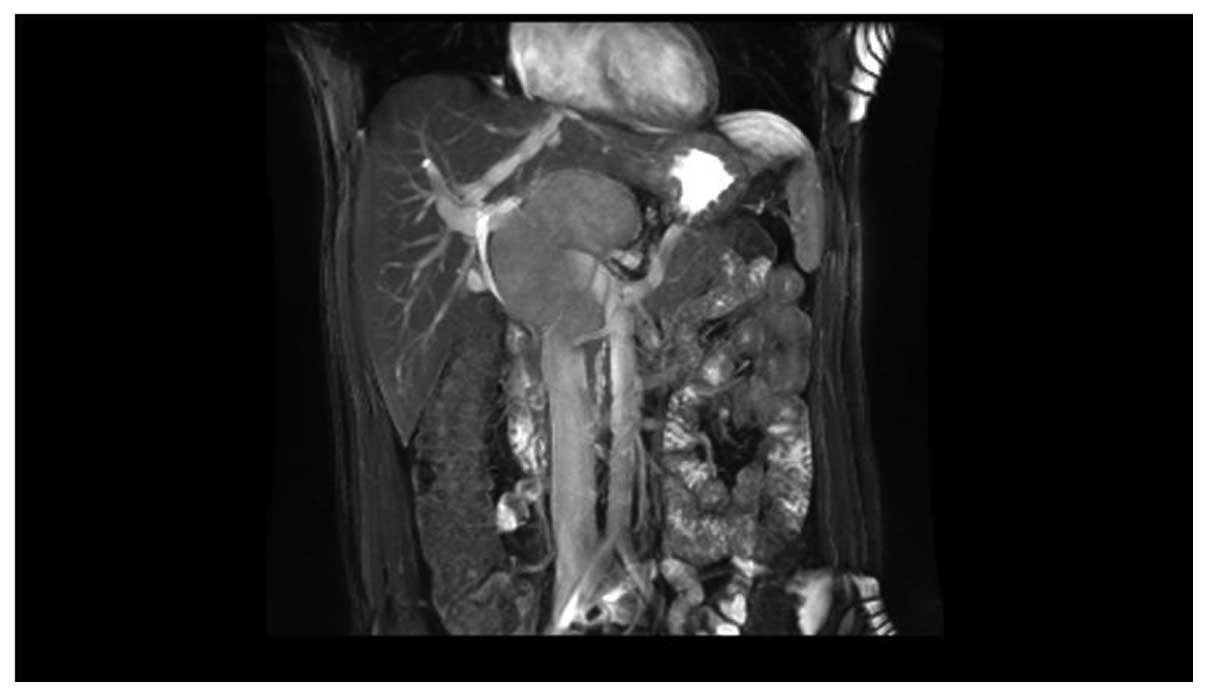
from the head of the pancreas. Upper abdominal T1-weighted dynamic
magnetic resonance imaging (MRI) revealed a hypointense, bilobular,
contoured, encapsulated mass measuring 8.7×9 cm, which exhibited
cystic components arising from the head and the uncinate process of
the pancreas and portal hilus; the mass encased the superior
mesenteric artery and laterally replaced the portal vein. Following
the administration of gadolinium, an early and persistent enhanced
signal was noted in the T2-weighted fat saturation sequences
(Figs. 1 and 2), and the lesion was markedly
hyperintense (Figs. 3 and 4). Based on the patient’s history, and the
clinical and imaging findings, an ultrasonography-guided Tru-cut
needle (WestCott 16G, Beckton Dickinson, Downers Grove, IL, USA)
biopsy was performed and pathological evaluation showed
characteristic spindle cells and strong positive immunoperoxidase
staining for S-100 protein, which was consistent with schwannoma.
Therefore, a duodenopancreatectomy was performed.
Discussion
Schwannoma or neurilemmoma are rare, well-defined,
benign encapsulated, slow growing tumors arising from Schwann cells
that encase the peripheral nerves (1–3).
Extracranial schwannomas typically occur in the extremities,
however, are also found in the trunk, head and neck, pelvis and
rectum (4–10). Intra-abdominal, retroperitoneal and
particularly intra-pancreatic presentation of schwannoma is
extremely rare (9,10). The number of cases of schwannoma
located in the small bowels, bile ducts, pelvis and sacrum are
currently limited (6,11) with <26 cases of pancreatic
schwannoma reported in the literature to date. These tumors vary
considerably in size, ranging from 1.5 to 20.0 cm in diameter and
the majority of the tumors are located in the head (38%) and body
(25%) of the pancreas. Half of the reported schwannomas are cystic
and 5% of schwannomas are associated with neurofibromatosis type
1.
Typical CT findings of pancreatic schwannomas are
similar to non-pancreatic schwannomas and demonstrate a
well-defined, encapsulated, hypointense solid mass with hemorrhage
or cystic degeneration, calcification or hyalinization (1–3,12).
Cystic formation may mimic cystic pancreatic lesions, such as
neuroendocrine tumors, cystadenoma, cystadenocarcinoma, intraductal
papillary mucinous tumor, lymphangiomas and pancreatic pseudocysts
(13).
Characteristic MRI findings of these tumors include
typical encapsulation, hypointensity on T1-weighted images and
hyperintensity on T2-weighted images (13). MRI may also differentiate pancreatic
schwannoma from adenocarcinoma due to the characteristic
hyperintensity on T2-weighted images and marked enhancement of the
lesion in comparison with the remainder of the pancreas.
In the present case, the tumor was an encapsulated
pancreatic mass with cystic components. Although CT and MRI may aid
in the differential diagnosis, a definitive diagnosis of pancreatic
schwannoma requires histopathological examination. Microscopically,
schwannomas are strongly positive for S-100 protein, vimentin and
cluster of differentiation 56, however, are negative for other
tumor markers (14). Surgical
excision with a close follow-up and surveillance remain the
mainstay treatment method for pancreatic schwannomas.
In conclusion, the diagnosis of pancreatic
schwannomas, although they are rare, must be considered in the
differential diagnosis of well-defined, encapsulated cystic lesions
of the pancreas.
References
|
1
|
Tofigh AM, Hashemi M, Honar BN and Solhjoo
F: Rare presentation of pancreatic schwannoma: a case report. J Med
Case Rep. 2:2682008.
|
|
2
|
Di Benedetto F, Spaggiari M, De Ruvo N, et
al: Pancreatic schwannoma of the body involving the splenic vein:
case report and review of the literature. Eur J Surg Oncol.
33:926–928. 2007.
|
|
3
|
Okuma T, Hirota M, Nitta H, et al:
Pancreatic schwannoma: report of a case. Surg Today. 38:266–270.
2008.
|
|
4
|
Jayaraj SM, Levine T, Frosh AC and Almeyda
JS: Ancient schwannoma masquerading as parotid pleomorphic adenoma.
J Laryngol Otol. 111:1088–1090. 1997.
|
|
5
|
Dayan D, Buchner A and Hirschberg A:
Ancient neurilemmoma (Schwannoma) of the oral cavity. J
Craniomaxillafac Surg. 17:280–282. 1989.
|
|
6
|
Hide IG, Baudouin CJ, Murray SA and
Malcolm AJ: Giant ancient schwannoma of the pelvis. Skeletal
Radiol. 29:538–542. 2000.
|
|
7
|
Graviet S, Sinclair G and Kajani N:
Ancient schwannoma of the foot. J Foot Ankle Surg. 34:46–50.
1995.
|
|
8
|
McCluggage WG and Bharucha H: Primary
pulmonary tumours of nerve sheath origin. Histopathology.
26:247–254. 1995.
|
|
9
|
Loke TH, Yuen NW, Lo KK, Lo J and Chan JC:
Retroperitoneal ancient schwannoma: review of clinico-radiological
features. Australas Radiol. 42:136–138. 1998.
|
|
10
|
Giglio M, Giasotto V, Medica M, Germinale
F, Durand F, Queirolo G and Carmignani G: Retroperitoneal ancient
schwannoma: case report and analysis of clinico-radiological
findings. Ann Urol (Paris). 36:104–106. 2002.
|
|
11
|
Toh LM and Wong SK: A case of cystic
schwannoma of the lesser sac. Ann Acad Med Singapore. 35:45–48.
2006.
|
|
12
|
Tortorelli AP, Rosa F, Papa V, et al:
Retroperitoneal schwannomas: diagnostic and therapeutic
implications. Tumori. 93:312–315. 2007.
|
|
13
|
Ferrozzi F, Bova D and Garlaschi G:
Pancreatic schwannoma: report of three cases. Clin Radiol.
50:492–495. 1995.
|
|
14
|
Tan G, Vitellas K, Morrison C and Frankel
WL: Cystic schwannoma of the pancreas. Ann Diagn Pathol. 7:285–291.
2003.
|