Introduction
Systemic sclerosis is a diffuse connective tissue
disorder, which affects the skin and internal organs. Its
pathological-anatomical basis is the fibrotic sclerotization of the
peripheral and internal organ blood vessels. The disease has a
chronic, progressive nature and primarily affects females. The skin
of the fingers is often the first area to be affected, which may
present with atrophy and edema. The skin of the fingers
progressively thickens (sclerodactyly) and the skin on the fingers
and other parts of the body becomes stiff and shiny. It is also
typical for patients to present with a mask-like face, limited
facial expressions and perioral furrows. Vascular afflictions
manifest as Raynaud’s phenomenon, which affects the fingers, ears,
tip of the nose and internal organs.
When compared with the general population, patients
with systemic sclerosis are at increased risk of developing
malignant tumors, particularly lung, breast, skin and hematological
malignancies (1–4). The areas most commonly affected in the
head and neck region include the oral cavity, oropharynx and
esophagus (5–6). The diagnosis and treatment of
malignancies in this area are accompanied by various problems, and
thus increased awareness may aid clinicians. Written informed
consent was obtained from the patient.
Case report
In March 2012, a 47-year-old female, with a
regularly monitored five-year history of rapidly progressing
systemic sclerosis, was examined at Charles University Third
Medical School and Královské Vinohrady Teaching Hospital (Prague,
Czech Republic). The patient presented with a one-month history of
firm, sensitive lumps (nodule-like structures) on the right side of
the neck (level III cervical lymph nodes). Sonography revealed a
structure with a nodular malignant appearance. The patient
underwent a panendoscopic exam without the identification of an
evident primary tumor, however, the exam was extremely difficult to
perform due to contracture of the masticatory muscles, which
resulted in reduced access to the oral cavity. Therefore, the
examining physician extirpated the enlarged cervical lymph
node.
A histological examination confirmed the presence of
metastatic squamous cell carcinoma. The patient underwent magnetic
resonance imaging (MRI), which revealed only postoperative changes.
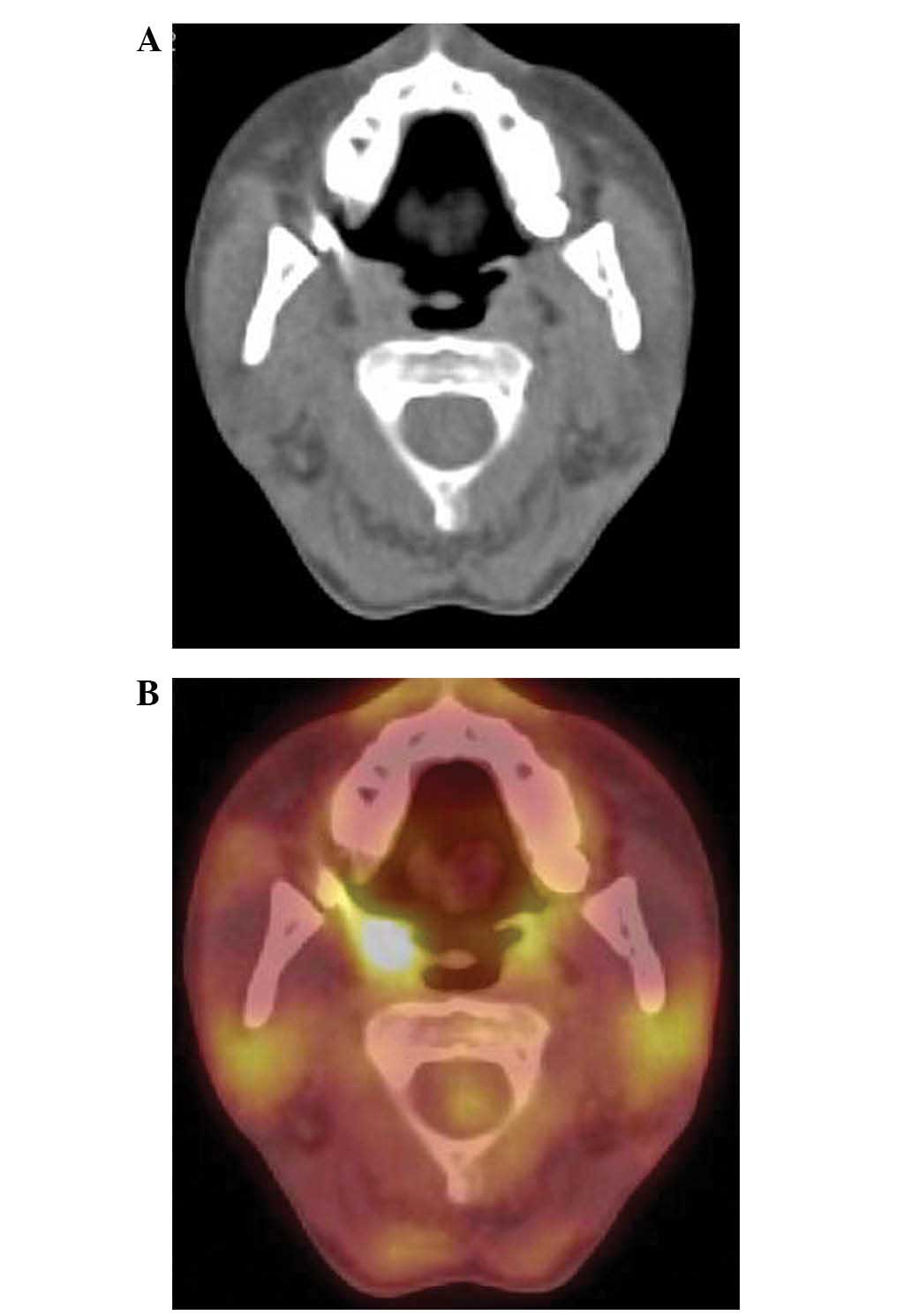
Based on positron emission tomography (PET)-computed tomography
(CT) scans, a suspected primary tumor in the right tonsil was
included in the differential diagnosis (Fig. 1). As it was impossible to collect a
useful sample for histological examination, additional medical
treatment was considered.
Subsequently, a right-sided bucopharyngectomy was
performed via a lateral pharyngotomy using an ablation clamp with
angled jaws, with perioperative verification of the primary tumor.
A neck dissection of the right side (level I–V cervical lymph
nodes) was performed simultaneously.
Postoperatively, the patient was ventilated via
endotracheal intubation to avoid a tracheostomy. The patient was
extubated on the second postoperative day. A definitive
histological examination confirmed squamous cell carcinoma of the
right tonsil. The resection of the tumor was radical and on
examination, angioinvasion was evident. The tumor was graded as pT2
(R0) pN2a M0 according to the International Union Against Cancer’s
TNM classification system (7). One
month following surgery, the patient underwent linear accelerator
radiotherapy (60 Gy in 2 Gy fractions for five weeks). The patient
tolerated the radiotherapy treatment well.
Four months following the completion of treatment,
the patient visited Charles University Third Medical School and
Královské Vinohrady Teaching Hospital with a two-week history of
dysphagia progressing toward aphagia, weight loss, painless
swelling of the right half of the tongue and dyspnea. A
fibrolaryngoscopic examination detected lymphedema of the
arytenoids and limited mobility of the vocal cords with limited
glottic space. Additionally, swelling of the anterior parts of the
right tongue was identified, which extended onto the base of the
tongue. The tongue was free of exulceration and with regard to
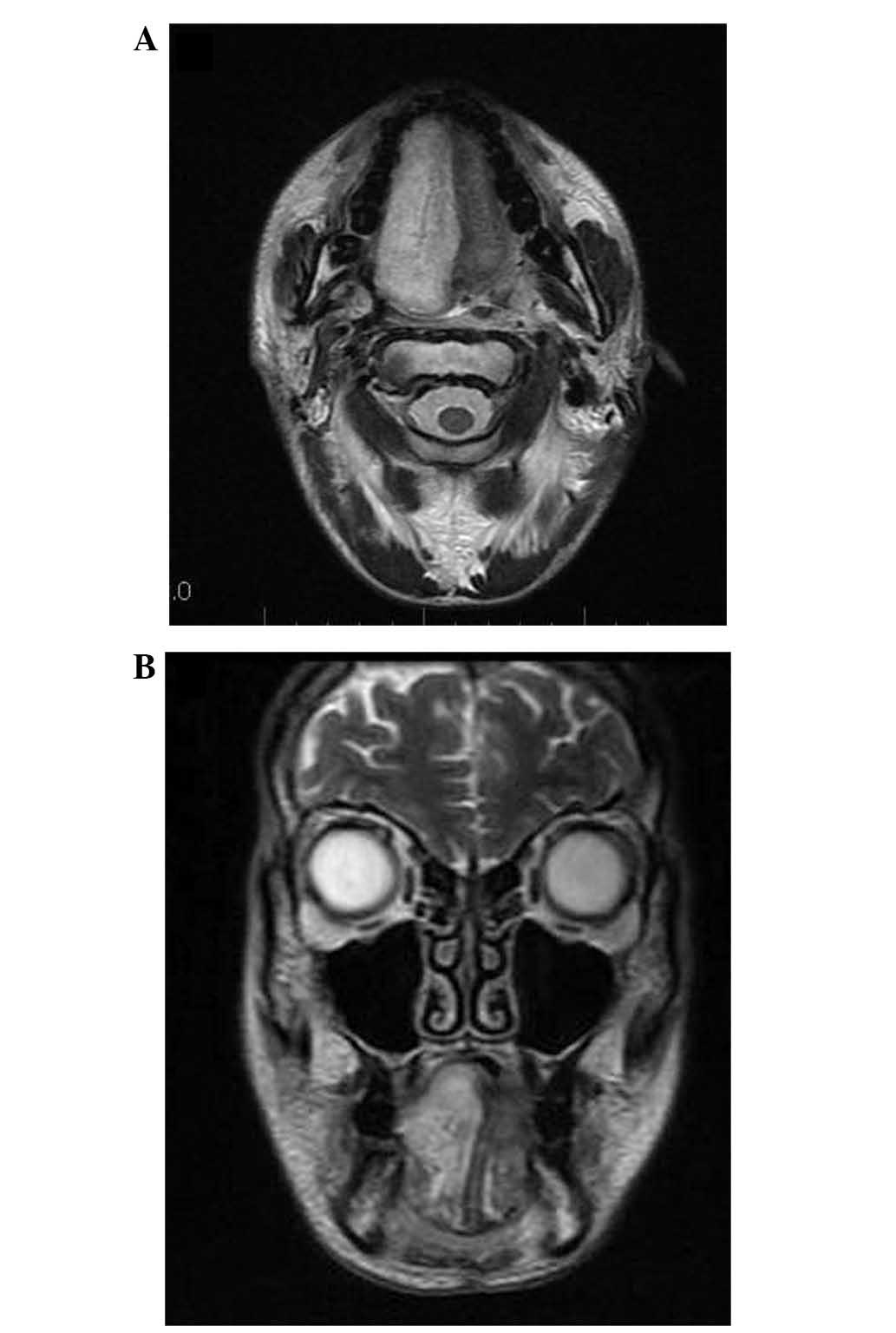
malignancy, the results of a probe excision were negative. MRI
scans indicated local disease recurrence (Fig. 2).
Due to the dyspnea and rapid deterioration in the
overall condition of the patient, a tracheostomy was performed and
a thin nasogastric tube was introduced. The malnutrition was
treated with intensive realimentation. The patient was consulted
with regard to further treatment. One month following stabilization
and an overall improvement in nutrition, an additional MRI was
performed and the results revealed that the infiltration remained
unchanged. Based on this information, the possibility of a
transmandibular biopsy was proposed, with perioperative
histological verification. However, the patient refused
transmandibular biopsy due to postoperative morbidity rates and the
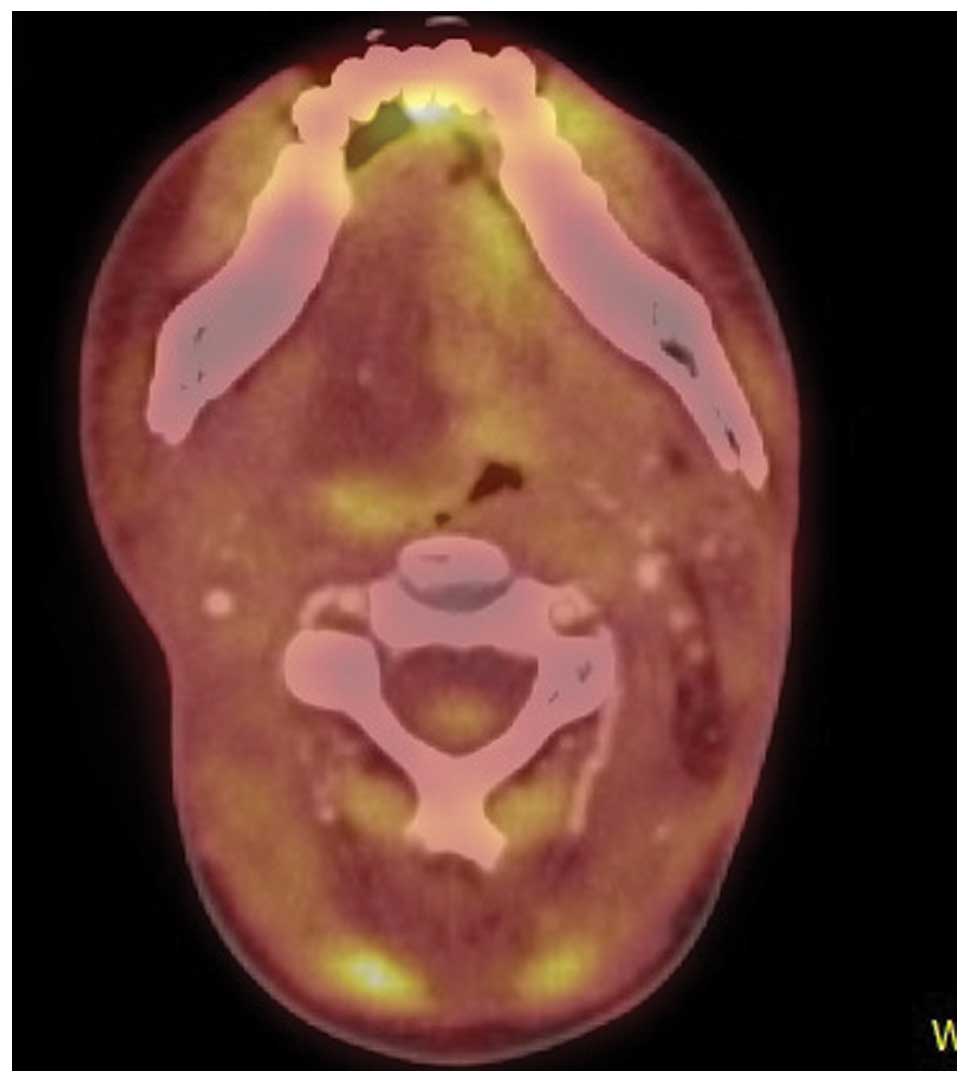
rapid progression of systemic disease. Another PET-CT was performed
(Fig. 3), however, the results did
not indicate a malignancy. Nasogastric intubation was discontinued
and a gastrostomy was performed. The patient has remained in a
stable condition for 12 months; weight gain has been observed and
the patient is healthy.
Discussion
Systemic sclerosis is a serious disease with
progressive involvement of the skin and organs, in particular the
esophagus and lungs (8–10). Currently, sclerosis patients are
treated symptomatically. Overall, the prognosis is extremely poor
and patients usually succumb to complications of the disease. A
number of signs and symptoms are associated with the disease and
initial symptoms include fatigue, weight loss and reactive
depression. Damage to individual organs also begins to occur
simultaneously, although initial findings are dominated by changes
to the skin (8,9,11).
With regard to otolaryngology, changes in the skin of the face are
highly significant as the skin undergoes scleroderma thickening,
becomes stiff and shiny, and forms radial furrows around the mouth.
These changes eventually result in impaired facial expressions and
a mask-like facial appearance (8–12).
Additionally, access to the oral cavity may deteriorate markedly,
which causes difficulty for examinations of the mouth and
oropharynx (8–10).
Certain scleroderma organ-associated symptoms may
mask symptoms of a malignancy in the head and neck region and may
lead to diagnostic uncertainty (11). As two-thirds of the distal esophagus
may be affected, patients may present with dysphagia, as well as
gastroesophageal reflux, which may lead to erosive inflammation of
the esophagus and the formation of adhesions (8–11).
Autoimmune alveolitis may gradually develop and progress into
pulmonary fibrosis, which may manifest as dyspnea. Pulmonary
fibrosis may then lead to pulmonary hypertension and right-sided
heart failure, the latter of which is the leading cause of
mortality in patients with systemic sclerosis. Additionally, the
heart and kidneys may be directly affected by the condition,
leading to myocardial inefficiencies or scleroderma renal crisis
presenting with rapidly progressive oliguria and renal failure,
respectively (8–12).
In patients with systemic sclerosis, there is a
markedly greater incidence of malignant disease, particularly those
involving the lungs and breasts, when compared with that of the
general population. However, the association between systemic
sclerosis and malignancy remains unclear. Hypotheses have been
proposed, which suggest that systemic sclerosis and malignancy
manifest as a result of alterations in the immune response or
genetic background. In a study by Siau et al (3), the average time between initial
diagnosis of systemic sclerosis and malignancy was observed to be
seven years (3).
Conversely, systemic sclerosis is regarded as a
paraneoplastic phenomenon (13),
which may develop much more rapidly than primary systemic sclerosis
(14). Radiotherapy may be a
trigger for pre-existing (asymptotic) systemic sclerosis,
particularly when undergoing radiotherapy for breast cancer
(15), as can treatment with
certain chemotherapeutics (14).
During the development of a malignancy in the head
and neck region, diagnostic, differential diagnostic and
therapeutic difficulties may occur at almost every stage. In the
present case, even at the initiation of treatment, numerous
problems were exhibited. Furthermore, examination was extremely
difficult due to the patient’s limited ability to open the mouth,
and the panendoscopy was also difficult to perform. In addition,
diagnostic tonsillectomy was impossible due to the condition of the
oropharynx. Therefore, formulating a diagnostic assessment was
extremely challenging and the primary carcinoma was confirmed
during the perioperative histological processing of tissue samples
obtained via a lateral pharyngotomy. Four months following the
completion of what had been considered to be successful treatment,
greater diagnostic and differential diagnostic difficulties
occurred, as the patient’s overall condition deteriorated rapidly
with dyspnea and severe dysphagia progressing toward aphagia. A
fibrolaryngoscopic examination revealed edematous arytenoids,
limited mobility of the vocal cords with a narrowed glottis,
swelling of the right-anterior sections of the tongue, which
continued onto the base of the tongue without exulceration.
When determining a differential diagnosis, the
possibility of local disease recurrence was initially considered,
however, a biopsy examination failed to confirm recurrence.
Conducting a probe excision was challenging and was therefore,
performed under general anesthesia with relaxation following a
tracheostomy (performed under local anesthesia), which was required
to protect the airway. Despite the relaxation, the examination of
the oral cavity and oropharynx was impossible. MRI analysis
(Fig. 2) revealed a recurrence of
the tumor in the body and base of the tongue. Infiltration,
however, was without exulceration. PET-CT (Fig. 3) scan revealed a post-irradiation
tissue reaction. With regard to the dyspnea, the progression of
pulmonary disease may have contributed, however, an X-ray
examination did not reveal any changes in the lungs.
A gastrostomy was performed for dysphagic
difficulties, which were associated with peroral diet
complications, however, questions remain with regard to the changes
in the distal part of the esophagus as they are associated with the
progression and complications of the disease. A duplicate tumor in
the esophagus may have caused the patient’s dysphagic difficulties.
A transmandibular biopsy with surgical management of the tumor of
the tongue was refused by the patient. This was due to the
progressive course of sclerosis and the uncertainty of disease
recurrence, as well as the uncertain outcome and the disfiguring
nature of the procedure.
The patient’s tissue reactions to surgical and
oncological treatment caused concern. Previous studies are
contradictory with regard to treatment methods (16–18),
however, the risk of toxicity is a constant, particularly that of
late toxicity (19). In the present
case, the patient recovered from all surgical procedures and also
tolerated radiotherapy well. However, whether the infiltrate on the
right-side (ipsilateral) of the tongue was a reaction to
radiotherapy remains unclear, as the patient exhibited
post-irradiative lymphedema of the proximal larynx.
In conclusion, systemic sclerosis is a chronic,
progressive disease with an extremely poor prognosis. The incidence
of malignant tumors in patients with this disease is greater than
that of the general population, and certain malignancies may occur
as a paraneoplastic process in individuals with systemic sclerosis.
The symptoms of sclerosis, which are associated with certain
organs, may overlap with the symptoms of malignant diseases of the
head and neck and thus, lead to difficulties with the differential
diagnosis. Sclerosis may also result in problems associated with
the standard examination process, caused by poor access to the oral
cavity and oropharynx. On consideration of treatment procedures,
the possibility that reactions in the soft tissues of the head and
neck may occur during surgical and oncological treatment must be
considered. Similarly, the poor prognoses of the two diseases
(malignant tumor and systemic sclerosis) must also be considered.
The patient presented in the current study tolerated the surgical
procedures and radiotherapy well, however, the post-radiotherapy
complications appear to have been the result of late toxicity.
Further studies are required to increase knowledge regarding
treatment course and patient tolerance.
References
|
1
|
Kuo CF, Luo SF, Yu KH, Chou IJ, Tseng WY,
Chang HC, Fang YF, Chiou MJ and See LC: Cancer risk among patients
with systemic sclerosis: a nationwide population study in Taiwan.
Scand J Rheumatol. 41:44–49. 2012. View Article : Google Scholar
|
|
2
|
Kang KY, Yim HW, Kim IJ, Yoon JU, Ju JH,
Kim HY and Park SH: Incidence of cancer among patients with
systemic sclerosis in Korea: results from a single centre. Scand J
Rheumatol. 38:299–303. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siau K, Laversuch Cj, Creamer P and
O’Rourke KP: Malignancy in scleroderma patients from south west
England: a population-based cohort study. Rheumatol Int.
31:641–645. 2011. View Article : Google Scholar
|
|
4
|
Szekanecs E, Szamosi S, Horvath A, Nemeth
A, Juhasz B, Szanto J, Szücs G and Szekanecz Z: Malignancies
associated with systemic sclerosis. Autoimmun Rev. 11:852–855.
2012. View Article : Google Scholar
|
|
5
|
Derk CT, Rasheed M, Artlett CM and Jimenez
SA: A cohort study of cancer incidence in systemic sclerosis. J
Rheumatol. 33:1113–1116. 2006.PubMed/NCBI
|
|
6
|
Derk CT, Rasheed M, Spiegel JR and Jimenez
SA: Increased incidence of carcinoma of the tongue in patients with
systemic sclerosis. J Rheumatol. 32:637–641. 2005.PubMed/NCBI
|
|
7
|
Sobin LH, Gospodarowicz MK and Wittekind
Ch; International Union Against Cancer (UICC). TNM Classification
of Malignant Tumours. 7th edition. Wiley-Blackwell; New York, NY:
2009
|
|
8
|
Clements PJ and Furst DE: Systemic
Sclerosis. 1st edition. Williams & Wilkins; Baltimore, MD:
1996
|
|
9
|
Kumar P, Galarraga B and Belch JJF:
Connective tissues disorders. Rheumatology. Hochberg MC, Silman AJ,
Smolen JS, Weinblatt ME and Weisman MH: 5th edition. Mosby
Elsevier; Philadelphia, PA: pp. 1361–1437. 2011
|
|
10
|
Wigley FM: Systemic sclerosis
(scleroderma) is unique among our rheumatic diseases. Preface.
Rheum Dis Clin North Am. 34:xi–xiiii. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Štork J: Sklerodermie. 1st edition. Galén;
Prague: 1996
|
|
12
|
LeRoy EC, Black CM, Fleischmajer R, et al:
Scleroderma (systemic sclerosis): clasification, subsets and
pathogenesis. J Rheumatol. 15:202–205. 1988.PubMed/NCBI
|
|
13
|
Orphanos G, Ardavanis A, Charalambous P,
Stavrakakis J and Rigatos G: Systemic sclerosis associated with
rectal cancer. Case report and a brief review of the literature. In
vivo. 22:825–830. 2008.
|
|
14
|
Szabolcsi O, Nagy-Toldi A, Zeher M and
Vegh J: Systemic sclerosis in a patient suffering from breast
cancer. Magy Onkol. 56:50–54. 2012.PubMed/NCBI
|
|
15
|
Marasini B, Conciato L, Belloli L and
Massarotti M: Systemic sclerosis and cancer. Int J Immunopathol
Pharmacol. 22:573–578. 2009.PubMed/NCBI
|
|
16
|
Dragun AE, Harper JL, Olyejar SE,
Zunzunegui RG and Wazer DE: The use of adjutant high-dose-rate
breast brychytherapy in patients with collagen vascular dinase: a
collaborative experience. Brachytherapy. 10:121–127. 2011.
View Article : Google Scholar
|
|
17
|
Kounalakis N, Pezner R, Staud CL and
Kruper L: Partial breast irradiation in a patient with bilateral
breast cancers and CREST syndrome. Brachytherapy. 10:486–490. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lowell D, Tatter S, Bourland JD, deGuzman
AF, Ekstrand KF, Ellis TL, Lovato JF, McMullen K, Munley MJ, Shaw
EG, et al: Toxicity of gamma knife radiosurgery in the treatment of
intracranial tumors in patients with collagen vascular diseases or
multiple sclerosis. Int J Radiat Oncol Biol Phys. 81:e519–e524.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lin A, Abu-Isa E, Griffith KA and
Ben-Josef E: Toxicity of radiotherapy in patients with collagen
vascular disease. Cancer. 113:648–653. 2008. View Article : Google Scholar : PubMed/NCBI
|