Introduction
As a result of significant improvements in surgical
methods and techniques used in the treatment of colorectal cancer,
the post-operative outcome of patients has improved. However, in
certain cases, life-threatening complications may occur following
colorectal surgery (1). The
evaluation of the risk factors associated with post-operative
complications in patients with colorectal cancer and the
identification of prognostic indicators is required to reduce the
post-operative mortality rate. Clinically, an increase in
circulating leucocytes, primarily granulocytes, has been observed
in patients with all advanced cancers; furthermore, the cellular
immune reaction has been reported to decrease with disease
progression in these patients (2).
Several studies have demonstrated that the level of the
granulocyte/lymphocyte (G/L) or neutrophil/lymphocyte (N/L) ratio
may predict prognosis following surgery and/or chemotherapy in
patients with colorectal cancer (3–8),
however, no studies investigating the potential associations
between the post-operative complications and pre-operative G/L
ratio have been reported. Therefore, the current study reviewed our
clinical experience with surgical therapy for colorectal cancer and
retrospectively analyzed the clinical relevance of the
pre-operative G/L ratio as a predictive marker of post-operative
complications in patients with colorectal cancer.
Materials and methods
Between January 2011 and June 2013, 85 patients (59
males and 26 females; mean age, 68.9 years) underwent surgery for
colorectal cancer at the Department of Surgery, Ibaraki Medical
Center, Tokyo Medical University (Ami, Japan). No patients had
received pre-operative chemotherapy. The patients were divided into
post-operative complication (n=16) and non-complication (n=69)
groups. The patient medical records were reviewed and clinical
data, including age, gender, body mass index (BMI), tumor
localization, tumor pathological type, cancer staging, surgery time
and volume of surgical bleeding were collected, in addition to
pre-operative laboratory data, including levels of albumin and
C-reactive protein (CRP), white blood cell (WBC) count, G/L ratio
and levels of hemoglobin, creatine kinase (CK), lactate
dehydrogenase (LDH), carcinoembryonic antigen (CEA) and
carbohydrate antigen (CA) 19-9. The cancer staging was classified
according to the degree of differentiation and the International
Union Against Cancer tumor-node-metastasis classification (7th
edition) (9). The Glasgow
Prognostic Score (GPS) was calculated using the serum albumin and
CRP levels (10). These 18
evaluative factors were compared between the groups. Written
informed consent was obtained from all patients and the study was
approved by the ethics committee of Ibaraki Medical Center, Tokyo
Medical University (Ami, Japan).
Data are presented as the mean ± standard deviation
(SD). Stat Mate IV (ATMS Co., Ltd., Tokyo, Japan) was used to
perform the statistical analysis. The Mann-Whitney U test, Fisher’s
exact test and the Pearson product-moment correlation coefficient
were used to evaluate the correlations between variables in the
univariate analysis, and a logistic regression model was used to
perform multivariate analysis. P<0.05 was considered to indicate
a statistically significant difference in all tests.
Results
Of the 85 patients, 16 (18.8%) developed
post-operative complications; six presented with an ileus (7.1%),
five with an anastomotic leak (5.9%), two with surgical site
infection (SSI; 2.4%), two with hepatic insufficiency (2.4%) and
one with disseminated intravascular coagulation (DIC; 1.2%). In
addition, two patients (2.4%) who developed hepatic insufficiency
and DIC, respectively, succumbed to the disease within 60 days of
the surgery.
Table I summarizes
the clinical data for the complication and non-complication groups.
The volume of surgical bleeding was significantly higher in the
complication group (299.8±361.7 ml) compared with the
non-complication group (155.6±268.6 ml; P<0.05). Although the
surgery time was longer in the complication group compared with the
non-complication group (199.8±75.4 vs. 180.2±81.4 min,
respectively), the difference was not statistically significant.
Furthermore, the differences in complications associated with age,
gender, BMI, tumor localization, tumor pathological type and cancer
staging were not statistically significant (Table I).
 | Table IClinical data between post-operative
complication and non-complication groups. |
Table I
Clinical data between post-operative
complication and non-complication groups.
| Variable | Complication
(n=16) | Non-complication
(n=69) | P-value |
|---|
| Age, years | 67.6±12.3 | 69.2±10.3 | NSa |
| Male gender, n | 13 | 46 | NSb |
| BMI,
kg/m2 | 21.9±4.7 | 22.5±3.9 | NSa |
| Tumor localization,
n | | | NSb |
| Colon | 7 | 41 | |
| Rectum | 9 | 28 | |
| Pathological tumor
type, n | | | NSb |
| Well- to
moderately-differentiated | 16 | 64 | |
|
Poorly-differentiated | 0 | 5 | |
| Cancer staging,
n | | | NSa |
| 0–I | 2 | 20 | |
| II | 4 | 23 | |
| III | 3 | 10 | |
| IV | 7 | 16 | |
| Surgery time,
min | 199.8±75.4 | 180.2±81.4 | NSa |
| Surgical bleeding,
ml | 299.8±361.7 | 155.6±268.6 | <0.05a |
Table II reveals
the comparison of the pre-operative laboratory data, including
levels of albumin and CRP, WBC count, GPS, G/L ratio and levels of
hemoglobin, CK, LDH, CEA, and CA19-9, between the complication and
non-complication groups. The G/L ratio was significantly higher in
the complication group compared with the non-complication group
(6.73±10.38 vs. 3.49±2.78, respectively; P<0.05). However, no
statistically significant difference was identified in the
complications associated with differences in levels of
pre-operative albumin and CRP, WBC count, GPS and levels of
hemoglobin, CK, LDH, CEA and CA19-9 (Table II).
 | Table IIPre-operative laboratory data (mean ±
standard deviation) between post-operative complication and
non-complication groups. |
Table II
Pre-operative laboratory data (mean ±
standard deviation) between post-operative complication and
non-complication groups.
| Variable | Complication
(n=16) | Non-complication
(n=69) | P-valuea |
|---|
| Albumin, g/dl | 3.63±0.63 | 3.91±0.60 | NS |
| CRP, mg/dl | 2.42±3.28 | 1.15±3.02 | NS |
| GPS | 0.68±0.87 | 0.46±0.81 | NS |
| WBC count, per
μl | 7143±1969 | 6462±1912 | NS |
| G/L ratio | 6.73±10.38 | 3.49±2.78 | <0.05 |
| Hemoglobin,
g/dl | 12.5±10.4 | 11.9±2.4 | NS |
| CK, IU/l | 94.0±89.2 | 90.9±71.2 | NS |
| LDH, IU/l | 270.5±178.7 | 227.8±164.9 | NS |
| CEA, ng/ml | 393.7±1089.8 | 111.3±464 | NS |
| CA19-9, U/ml | 165.6±527.6 | 627.2±2799.3 | NS |
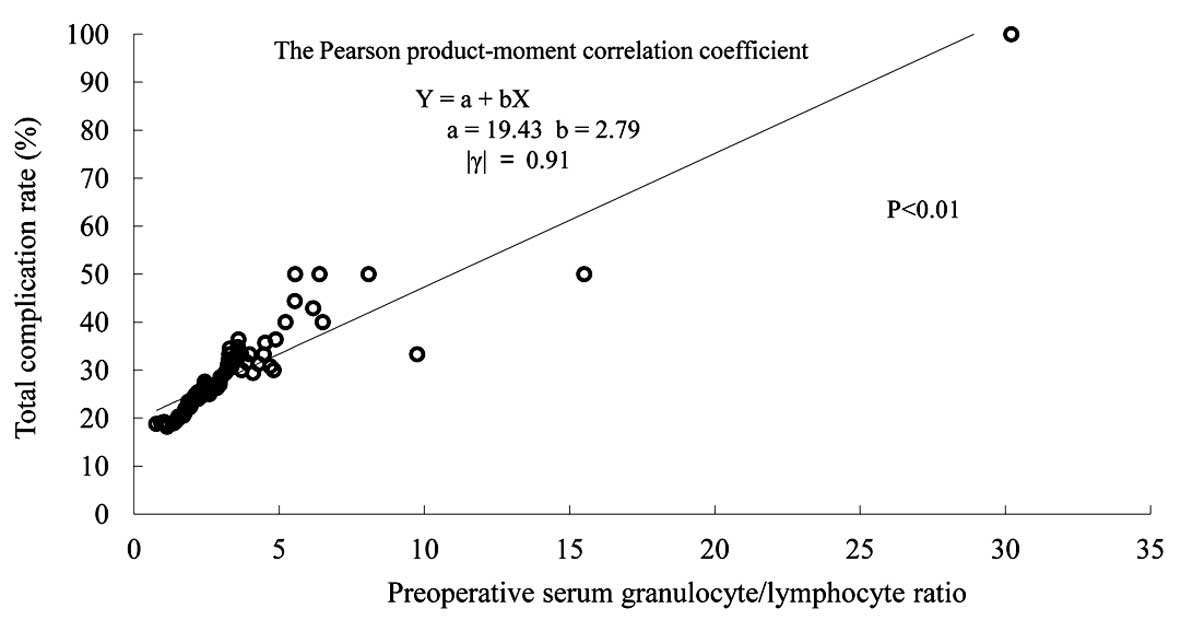
The multivariate logistic regression analysis,
conducted using the complication risk factors determined by
univariate analysis (the amount of surgical bleeding and the G/L
ratio), revealed that the volume of surgical bleeding and the G/L
ratio were independent risk factors of post-operative complications
in patients with colorectal cancer (surgical bleeding: Odds ratio,
1.912; 95% confidence interval, 1.018–3.587; P=0.043; and G/L
ratio: Odds ratio, 2.180; 95% confidence interval, 1.112–4.274;
P=0.023; Table III). Fig. 1 shows the statistical regression
line between the pre-operative G/L ratio levels and the total
post-operative complication rate, with a statistically significant
correlation (P<0.01; Fig. 1).
The post-operative complication rate could be predicted from the
pre-operative G/L ratio level.
 | Table IIIMultivariate analysis of the
independent risk factors for post-operative complications. |
Table III
Multivariate analysis of the
independent risk factors for post-operative complications.
| Variables | Odds ratio | 95% Confidence
interval | P-valuea |
|---|
| Surgical bleeding,
ml (<100, 100–200, 200<) | 1.912 | 1.018–3.587 | 0.043 |
| G/L ratio (<2.5,
2.5–3.5, 3.5<) | 2.180 | 1.112–4.274 | 0.023 |
Discussion
Post-operative complications in colorectal cancer
may result in functional impairments or even fatal outcomes for the
patient, and also lead to an increase in medical costs associated
with an extension of the hospital stay (11–13).
Predicting the development of post-operative complications is
useful in the perioperative management of patients, beginning
pre-operatively and continuing into the post-operative period, and
an early response to post-operative complications has contributed
to a decrease in post-operative mortality rates (14,15).
The three most frequent post-operative complications
of surgery for colorectal cancer are ileus, anastomotic leak and
SSI. Chapuis et al (16)
reported that the incidence of a post-operative ileus was 14.0% and
that the risk factors included male gender, comorbidity with
respiratory diseases, emergency surgery and if the surgery had been
performed in >3 h. In addition, the incidence of anastomotic
leaks and SSI have been reported to be 1.5–11.5% and 11.7–15.7%,
respectively, with risk factors including high BMI, history of
laparotomy, advanced-stage cancer and malnutrition (17–21).
Yasunaga et al (22)
reported that the incidence of complications in Japanese subjects
following gastrointestinal surgery was at its lowest when the BMI
was ~23.0 kg/m2, but that it was high when the BMI was
≤18.5 or ≥30.0 kg/m2. In the current study, the mean BMI
of the subjects in the complication and non-complication groups was
~22.0 kg/m2, therefore indicating that there was no
association between BMI and the development of post-operative
complications. The nutritional assessment of patients with cancer
is significant in improving the prognosis. Ishizuka et al
(23,24) reported the GPS to be a
post-operative prognostic factor in patients with colorectal
cancer. However, in the current study, no association between the
GPS and post-operative complications was identified. This is
possibly due to the fact that the study was comprised of patients
with a wide range of colorectal cancers, from early-stage to
advanced-stage cancers with distant metastasis. A comparison
between the complication group and non-complication group showed no
statistically significant difference in GPS, as although the levels
of CRP tended to be high in the complication group, there was
almost no difference in the albumin levels. An albumin level of
≤3.5 g/dl is defined as low (and thus associated with increased
risk) by GPS (10). In patients
with colorectal cancer, problems associated with oral intake due to
intestinal transit disorders, advanced-stage cancer or cachexia
associated with distant metastases may result in hypoalbuminemia
(25). Therefore, this indicates
that if the control group was comprised of only patients with
highly-advanced colorectal cancers, the GPS may be a risk factor
for post-operative complications (26).
The present study examined 18 factors and focused on
the pre-operative G/L ratio in the blood of patients with
colorectal cancer, and further determined the correlation between
the G/L ratio and post-operative complications. A correlation
between the prognosis and the G/L or N/L ratios has been reported
in various types of cancers (27–29).
Clinically, patients with cancer occasionally present with an
elevated WBC count, particularly an elevated granulocyte count, and
a decreased lymphocyte count. When the progression and
proliferation of the cancer is chronic and biologically invasive,
it is accompanied by functional impairments due to localized tissue
hemorrhage, ischemia or necrosis and causes various types of immune
inflammatory responses. These responses include an elevated WBC
count, particularly an elevated granulocyte count, the
immunosuppression of lymphocytes, elevated levels of inflammatory
cytokines, such as interleukin (IL)-6, and acute phase reactants,
such as CRP, a negative nitrogen balance due to increased
decomposition of muscle proteins, and the inhibition of albumin
synthesis in the liver. The reactions are caused by a cytokine
network composed of IL-6, IL-1 and tumor necrosis factor-α
(30,31). IL-6 is a lectin, which is produced
by T-cells, neutrophils, macrophages and tumor cells, and a
cytokine that controls humoral immunity (32,33).
The extent of biological invasion can be determined by the IL-6
levels; in colorectal cancers, IL-6 is reportedly associated with
the progression of cancer and prognosis (34,35).
We previously reported that a high G/L ratio prior to surgery is a
risk factor associated with the prognosis of patients with
colorectal cancer, and that a correlation exists between the G/L
ratio prior to surgery and the IL-6 concentration (8,36). The
findings of the present study suggest that a high G/L ratio prior
to surgery is a risk factor for post-operative complications in
patients with colorectal cancer. Taking the previous findings into
consideration, a high G/L ratio prior to surgery in patients with
colorectal cancer indicates high pre-operative IL-6 levels, i.e., a
biological invasion, which is believed to cause post-operative
complications. In addition, the present study also confirmed that
the amount of surgical bleeding is a risk factor for post-operative
complications. The volume of surgical bleeding reflects the damage
to the biological tissue, which is accompanied by IL-6 production,
and is considered to be strongly associated with post-operative
complications (37,38).
Among the 18 factors that were examined in the
present study, only the pre-operative G/L ratio and the volume of
surgical bleeding were confirmed as risk factors for post-operative
complications. Of these two factors, the G/L ratio allows for the
pre-operative prediction of post-operative complications;
furthermore, the G/L ratio is simple, easy to measure and is likely
to aid in the future surgical management of patients with
colorectal cancer. The findings of this study raise issues that
remain to be discussed, particularly those pertaining to the types
of post-operative complications for which the G/L ratio has
specificity as a risk factor. To address these issues, further
studies comprising a larger number of patients are required in the
future.
In conclusion, to reduce the post-operative
complications in patients with colorectal cancer, it is essential
to reduce the possible amount of surgical bleeding. The
pre-operative G/L ratio may be a clinically relevant pre-operative
predictive marker in these patients.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for reviewing the English language of
the original manuscript.
References
|
1
|
Whistance RN, Forsythe RO, McNair AG, et
al; Core Outcomes and iNformation SEts iN SUrgical
Studies-ColoRectal Cancer Working Group. A systematic review of
outcome reporting in colorectal cancer surgery. Colorectal Dis.
15:e548–e560. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Coussens LM and Werb Z: Inflammation and
cancer. Nature. 420:860–867. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Walsh SR, Cook EJ, Goulder F, Justin TA
and Keeling NJ: Neutrophil-lymphocyte ratio as a prognostic factor
in colorectal cancer. J Surg Oncol. 91:181–184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Halazun KJ, Aldoori A, Malik HZ, et al:
Elevated preoperative neutrophil to lymphocyte ratio predicts
survival following hepatic resection for colorectal liver
metastases. Eur J Surg Oncol. 34:55–60. 2008. View Article : Google Scholar
|
|
5
|
Chua W, Charles KA, Baracos VE and Clarke
SJ: Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in
patients with advanced colorectal cancer. Br J Cancer.
104:1288–1295. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ding PR, An X, Zhang RX, et al: Elevated
preoperative neutrophil to lymphocyte ratio predicts risk of
recurrence following curative resection for stage IIA colon cancer.
Int J Colorectal Dis. 25:1427–1433. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hung HY, Chen JS, Yeh CY, et al: Effect of
preoperative neutrophil-lymphocyte ratio on the surgical outcomes
of stage II colon cancer patients who do not receive adjuvant
chemotherapy. Int J Colorectal Dis. 26:1059–1065. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shimazaki J, Goto Y, Nishida K, et al: In
patients with colorectal cancer, preoperative serum interleukin-6
level and granulocyte/lymphocyte ratio are clinically relevant
biomarkers of long-term cancer progression. Oncology. 84:356–361.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sobin LH, Gospodarowicz MK and Wittekind
C: TNM Classification of Malignant Tumors. 7th edition.
Wiley-Blackwell; Oxford: 2009
|
|
10
|
Forrest LM, McMillan DC, McArdle CS,
Angerson WJ and Dunlop DL: Evaluation of cumulative prognostic
scores based on the systemic inflammatory response in patients with
inoperable non-small-cell lung cancer. Br J Cancer. 89:1028–1030.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jean-Claude M, Emmanuelle P, Juliette H,
et al: Clinical and economic impact of malnutrition per se on the
postoperative course of colorectal cancer patients. Clin Nutr.
31:896–902. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lee L, Li C, Landry T, Latimer E, Carli F,
Fried GM and Feldman LS: A systematic review of economic
evaluations of enhanced recovery pathways for colorectal surgery.
Ann Surg. 259:670–676. 2014. View Article : Google Scholar
|
|
13
|
Damle RN, Cherng NB, Flahive JM, Davids
JS, Maykel JA, Sturrock PR, Sweeney WB and Alavi K: Clostridium
difficile Infection After Colorectal Surgery: A Rare but Costly
Complication. J Gastrointest Surg. Aug;2014.(Epub ahead of print).
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kwag SJ, Kim JG, Kang WK, Lee JK and Oh
ST: The nutritional risk is a independent factor for postoperative
morbidity in surgery for colorectal cancer. Ann Surg Treat Res.
86:206–211. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pommergaard HC, Gessler B, Burcharth J,
Angenete E, Haglind E and Rosenberg J: Preoperative risk factors
for anastomotic leakage after resection for colorectal cancer: a
systematic review and meta-analysis. Colorectal Dis. 16:662–671.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chapuis PH, Bokey L, Keshava A, et al:
Risk factors for prolonged ileus after resection of colorectal
cancer: an observational study of 2,400 consecutive patients. Ann
Surg. 257:909–915. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Telem DA, Chin EH, Nguyen SQ and Divino
CM: Risk factors for anastomotic leak following colorectal surgery:
a case-control study. Arch Surg. 145:371–376. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Aytac E, Lavery IC, Kalady MF and Kiran
RP: Impact of obesity on operation performed, complications, and
long-term outcomes in terms of restoration of intestinal continuity
for patients with mid and low rectal cancer. Dis Colon Rectum.
56:689–697. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Itatsu K, Sugawara G, Kaneoka Y, et al:
Risk factors for incisional surgical site infections in elective
surgery for colorectal cancer: focus on intraoperative meticulous
wound management. Surg Today. 44:1242–1252. 2014. View Article : Google Scholar
|
|
20
|
Takakura Y, Hinoi T, Egi H, et al:
Procalcitonin as a predictive marker for surgical site infection in
elective colorectal cancer surgery. Langenbecks Arch Surg.
398:833–839. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bot J, Piessen G, Robb WB, Roger V and
Mariette C: Advanced tumor stage is an independent risk factor of
postoperative infectious complications after colorectal surgery:
arguments from a case-matched series. Dis Colon Rectum. 56:568–576.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yasunaga H, Horiguchi H, Matsuda S, et al:
Body mass index and outcomes following gastrointestinal cancer
surgery in Japan. Br J Surg. 100:1335–1343. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ishizuka M, Nagata H, Takagi K, Horie T
and Kubota K: Inflammation-based prognostic score is a novel
predictor of postoperative outcome in patients with colorectal
cancer. Ann Surg. 246:1047–1051. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ishizuka M, Nagata H, Takagi K, Iwasaki Y
and Kubota K: Inflammation-based prognostic system predicts
postoperative survival of colorectal cancer patients with a normal
preoperative serum level of carcinoembryonic antigen. Ann Surg
Oncol. 19:3422–3431. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lai CC, You JF, Yeh CY, Chen JS, Tang R,
Wang JY and Chin CC: Low preoperative serum albumin in colon
cancer: a risk factor for poor outcome. Int J Colorectal Dis.
26:473–481. 2011. View Article : Google Scholar
|
|
26
|
Ishizuka M, Nagata H, Takagi K, Iwasaki Y
and Kubota K: Inflammation-based prognostic system predicts
survival after surgery for stage IV colorectal cancer. Am J Surg.
205:22–28. 2013. View Article : Google Scholar
|
|
27
|
Mohri Y, Tanaka K, Ohi M, Yokoe T, Miki C
and Kusunoki M: Prognostic significance of host- and tumor-related
factors in patients with gastric cancer. World J Surg. 34:285–290.
2010. View Article : Google Scholar
|
|
28
|
Sarraf KM, Belcher E, Raevsky E, Nicholson
AG, Goldstraw P and Lim E: Neutrophil/lymphocyte ratio and its
association with survival after complete resection in non-small
cell lung cancer. J Thorac Cardiovasc Surg. 137:425–428. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Cho H, Hur HW, Kim SW, Kim SH, Kim JH, Kim
YT and Lee K: Pre-treatment neutrophil to lymphocyte ratio is
elevated in epithelial ovarian cancer and predicts survival after
treatment. Cancer Immunol Immunother. 58:15–23. 2009. View Article : Google Scholar
|
|
30
|
Dinarello CA: Proinflammatory and
anti-inflammatory cytokines as mediators in the pathogenesis of
septic shock. Chest. 112:321S–329S. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Malicki S, Winiarski M, Matlok M, et al:
IL-6 and IL-8 responses of colorectal cancer in vivo and in vitro
cancer cells subjected to simvastatin. J Physiol Pharmacol.
60:141–146. 2009.
|
|
32
|
Ardestani SK, Inserra P, Solkoff D and
Watson RR: The role of cytokines on tumor progression: A review.
Cancer Detect Prev. 23:215–225. 1999. View Article : Google Scholar
|
|
33
|
Esfandi F, Mohammadzadeh Ghobadloo S and
Basati G: Interleukin-6 level in patients with colorectal cancer.
Cancer Lett. 244:76–78. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Galizia G, Orditura M, Romano C, et al:
Prognostic significance of circulating IL-10 and IL-6 serum levels
in colon cancer patients undergoing surgery. Clin Immunol.
102:169–178. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Belluco C, Nitti D, Frantz M, et al:
Interleukin-6 blood level is associated with circulating
carcinoembryonic antigen and prognosis in patients with colorectal
cancer. Ann Surg Oncol. 7:133–138. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Tabuchi T, Shimazaki J, Satani T, et al:
The perioperative granulocyte/lymphocyte ratio is a clinically
relevant marker of surgical stress in patients with colorectal
cancer. Cytokine. 53:243–248. 2011. View Article : Google Scholar
|
|
37
|
Kvarnström A, Swartling T, Kurlberg G,
Bengtson JP and Bengtsson A: Pro-inflammatory cytokine release in
rectal surgery: comparison between laparoscopic and open surgical
techniques. Arch Immunol Ther Exp (Warsz). 61:407–411. 2013.
View Article : Google Scholar
|
|
38
|
Tang Y, Xia XF, Zhang Y, et al:
Establishment of an experimental mouse model of trauma-hemorrhagic
shock. Exp Anim. 61:417–425. 2012. View Article : Google Scholar : PubMed/NCBI
|