Introduction
Peripheral primitive neuroectodermal tumor/Ewing’s
sarcoma (pPNET/EWS) is an aggressive type of sarcoma characterized
by the t(11; 22)(q24;q12) translocation and overexpression of the
cluster of differentiation (CD)99/MIC2 gene (1). pPNET is predominantly considered to be
a malignant bone or soft tissue tumor of children and young adults
that is uncommon in individuals aged >30 years (2). pPNET of the kidney is very rare, and
is even rarer in older patients or in patients who have received
treatment for a different type of cancer. The current study
presents the first known case of renal pPNET following breast
adenocarcinoma in a 51-year-old female. Written informed consent
was obtained from the patient’s family.
Case report
Patient presentation
In December 2013, a 51-year-old female complaining
of right flank pain was admitted to the West China Hospital of
Sichuan University (Chengdu, China). Urine examination determined
positive occult blood; however, all other laboratory analyses were
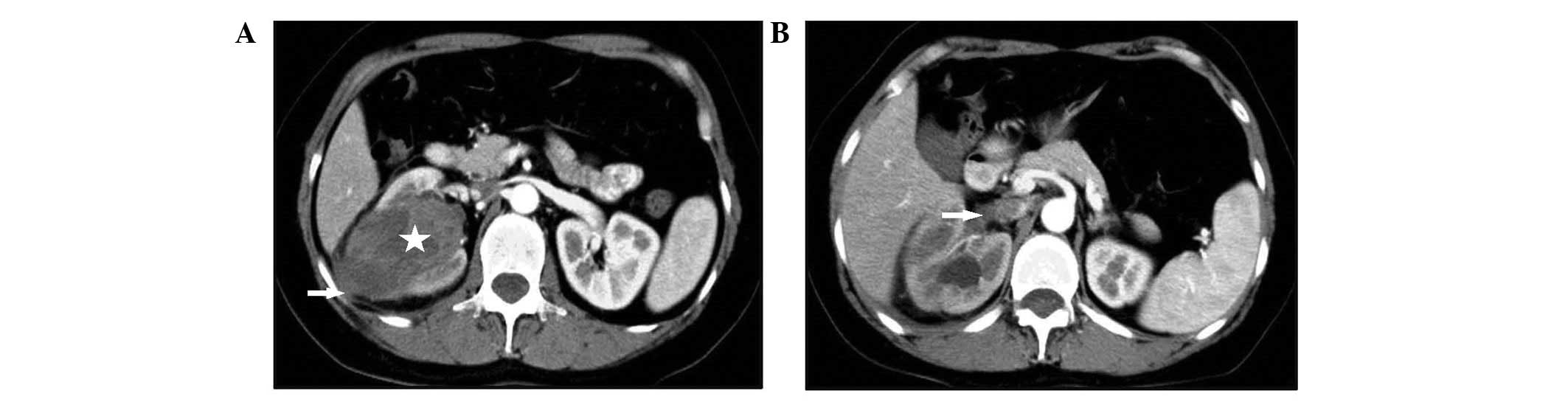
unremarkable. Ultrasonography (USG) and computerized tomography
(CT) scans revealed a 7×4-cm mass with an irregular contour in the
lower pole of the right kidney, which involved the renal vein and
the inferior vena cava (IVC). Enhanced CT scans identified
extension of the tumor into the perirenal space and Gerota’s fascia
(Fig. 1). The patient had been
treated by radical mastectomy and adjuvant chemotherapy for a left
breast adenocarcinoma five years prior to the current
hospitalization. No evidence of breast cancer recurrence was
observed.
Pathological observations
The patient received radical nephrectomy with
resection of tumor thrombi in the IVC and right renal vein.
Grossly, the kidney measured 11.5×8.5×4.6 cm and protruded from the
kidney surface. On cut surface, the nodular, solid tumor measured
7.0×4.5×3.5 cm, with areas of hemorrhage and necrosis, as well as
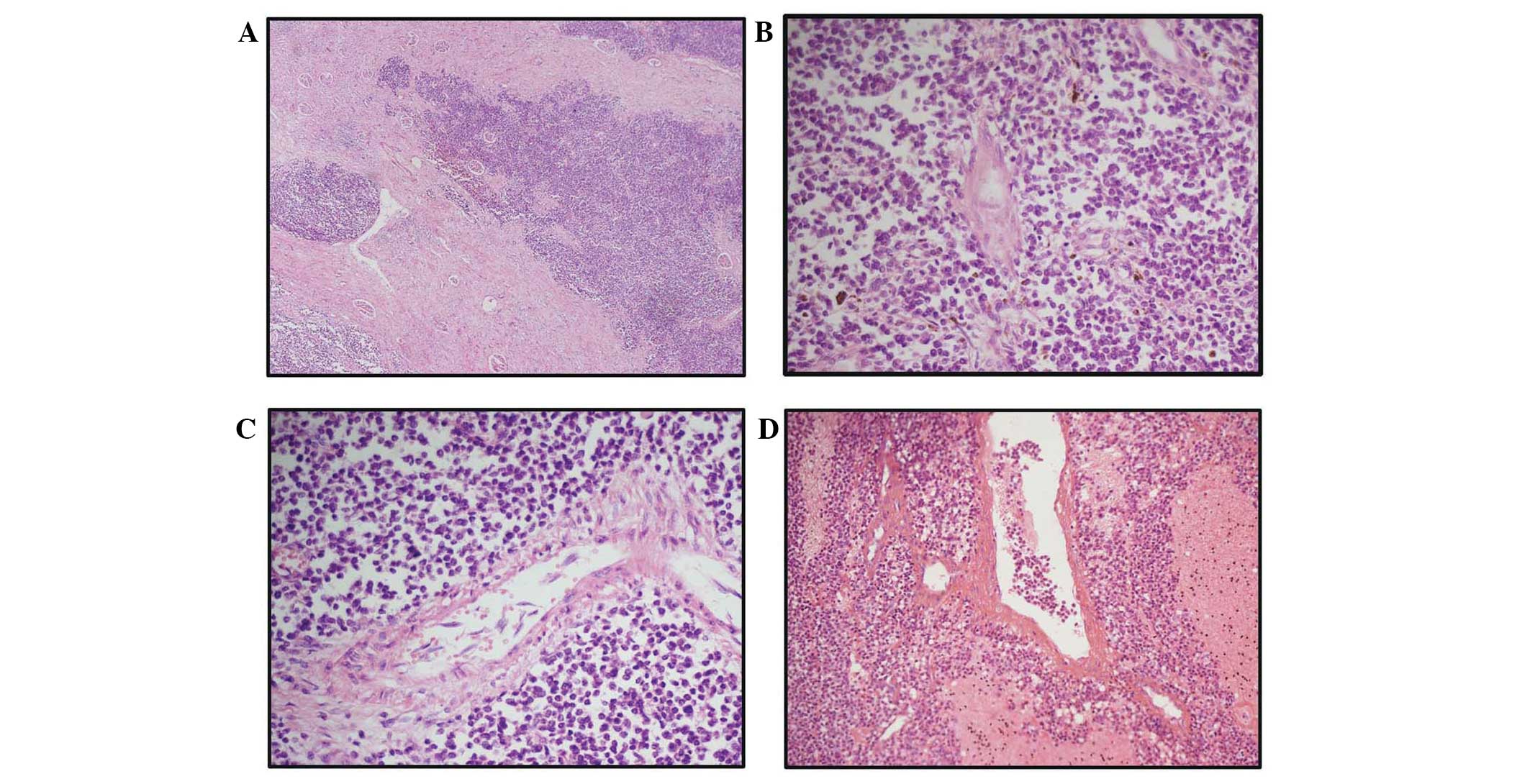
infiltration into the medulla and cortex. Analysis of hematoxylin
and eosin-stained sections revealed that the tumor was composed of
monotonous, small, blue round cells, two to three times the size of
lymphocytes, with hyperchromatic nuclei and scanty cytoplasm.
Furthermore, vague rosette-like patterns or perivascular
concentrations of tumor cells were observed (Fig. 2).
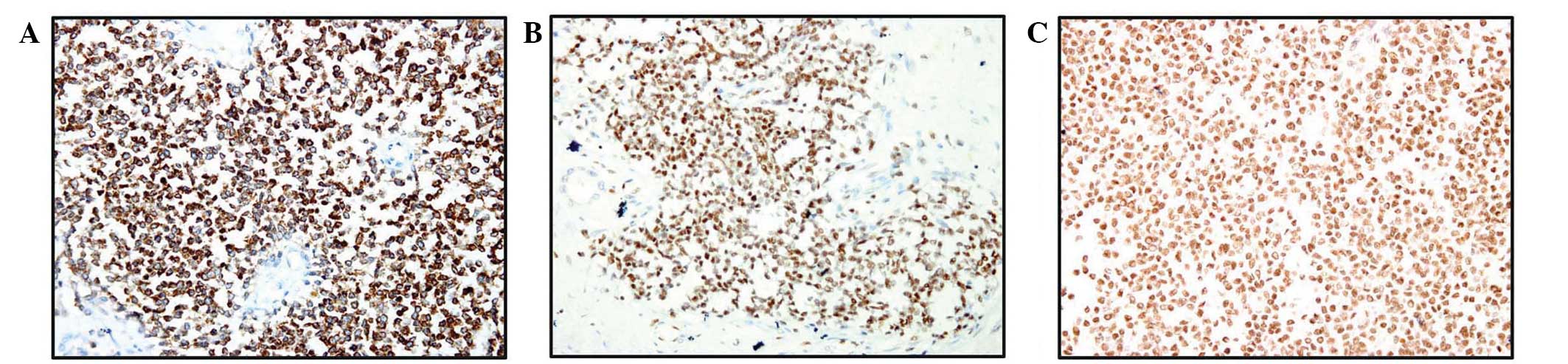
An immunohistochemical panel demonstrated strong,
diffuse membranous positivity for CD99 and nuclear staining for
friend leukemia integration 1 (FLI1) in the tumor sections
(Fig. 3A and B, respectively). No
loss of integrase interactor-1 (INI-1) protein expression levels
were observed, as determined by the nuclear positivity for INI-1
(Fig. 3C), and the Ki-67 nuclear
labeling index was ~10%. Additionally, the tumor cells were
negative for desmin, myogenin, leukocyte common antigen (LCA),
CD20, CD3, cytokeratin, P63 and Wilms’ tumor 1 (WT-1).
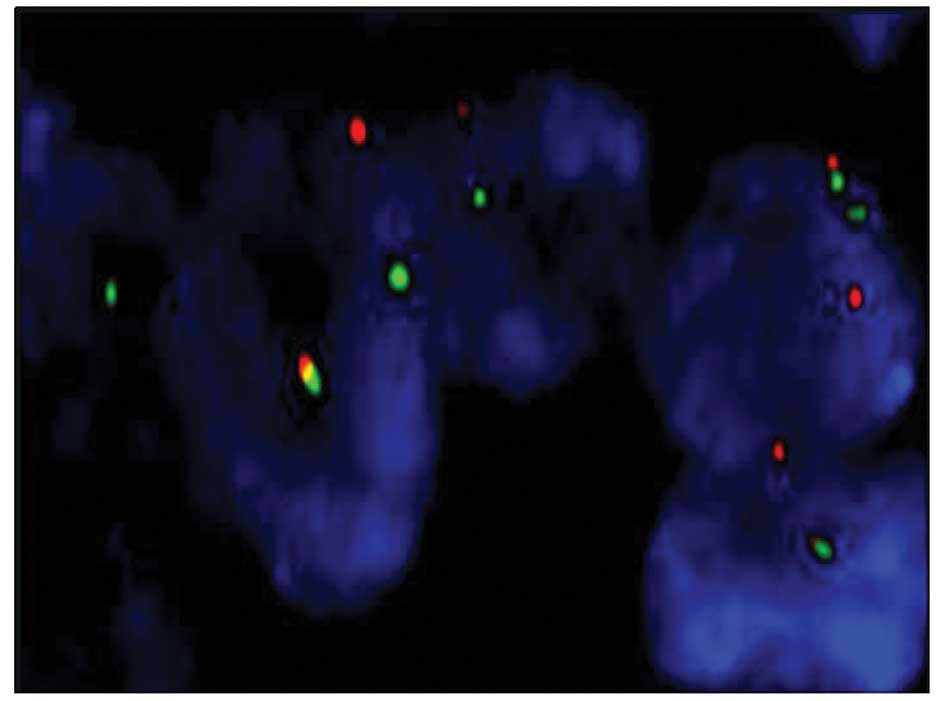
Fluorescence in situ hybridization (FISH)
analysis using a Vysis LSI EWSR1 (22q12) Dual Color, Break Apart
Rearrangement probe (Abbott Molecular, Inc., Des Plaines, IL, USA)
was performed and revealed the characteristic EWSR1 translocation,
confirming the diagnosis of pPNET of the kidney (Fig. 4).
Follow-up
The patient declined chemotherapy following surgery
but accepted traditional Chinese medicine (six ingredient rehmannia
pill). The patient has been followed up for the previous eight
months with scheduled CT and USG scans, and periodic tumor marker
monitoring. No evidence of recurrence or metastasis has been
observed thus far.
Discussion
pPNET is a small round-cell tumor that predominantly
occurs in bone and soft tissue; however, pPNET is occasionally
reported in visceral organs, such as urogenital, intra-abdominal
and intrathoracic organs. pPNET of the kidney is uncommon (3–5) and
was first reported in 1975 (6).
Since the first report, ~150 cases have been published in the
medical literature, with the largest series of 24 cases reported by
Zöllner et al (7). pPNET of
the kidney is an aggressive disease with a high metastatic
potential that predominantly occurs in children and young adults
(median patient age, 28 years) and exhibits a slight male
predominance (male:female ratio, 1.2:1) (8). pPNET of the kidney following or
synchronous with a different primary cancer is extremely rare, with
only two reported cases (from the USA and Germany, respectively)
(9,10). To the best of our knowledge, the
present case is unique: A female aged >50 years with a history
of breast adenocarcinoma that had been treated with chemotherapy
five years prior to the diagnosis of renal pPNET. Only six cases of
a patient aged >50 years have previously been reported (9,11–14),
the clinicopathologic features of which, together with that of the
present case, are summarized in Table
I. Whether the renal pPNETs developed independently or were
associated with the previous cancer is unknown and future studies
are required to clarify the issue.
 | Table IClinical and follow-up data of cases
of renal peripheral primitive neuroectodermal tumor in older
patients. |
Table I
Clinical and follow-up data of cases
of renal peripheral primitive neuroectodermal tumor in older
patients.
| Case report
(reference number) | Age, years | Gender | Tumor size, cm | Position | CD99 IHC | EWSR1 FISH | Treatment
strategy | Chemotherapeutic
agents | Recurrence or
metastasis | Follow-up period | Outcome at time of
report |
|---|
| Tariq et al
(11) | 57 | Female | UNK | UNK | + | + | Nephrectomy and
multimodal treatment | UNK | Pulmonary metastasis
at diagnosis | 8 years | Alive with stabilized
lung metastasis |
| Mandal et al
(12) | 50 | Female | 16.0 | L | + | NC | Nephrectomy and
chemotherapy | Vincristine, mesna,
ifosfamide and doxorubicin | Retroperitoneal lymph
nodal metastasis at diagnosis | 1 year | Alive |
| Wedde et al
(13) | 73 | Male | UNK | R | + | + | Nephrectomy and
chemotherapy | UNK | No | >7 months | Alive |
| Koski et al
(14) | 78 | Female | 10.9 | L | + | NC | Nephrectomy | NC | Pulmonary metastasis
without chemotherapy | 2 weeks | Deceased |
| Jimenez et al
(9) | 69 | Female | 5.0 | R | + | NC | Nephrectomy and
chemotherapy | Carboplatinum, VP-16,
taxol interferon and estramustine etoposide | Lung and bone
metastasis six months after chemotherapy | 25 months | Deceased |
| Jimenez et al
(9) | 50 | Male | UNK | UNK | + | NC | Nephrectomy | NC | UNK | UNK | UNK |
| Present case | 51 | Female | 11.5 | R | + | + | Nephrectomy | NC | No | 8 months | Alive |
Diagnosis of pPNET is based on morphologic,
immunohistochemical and genetic analyses. For example, pPNET of the
kidney is characterized by small, round cells with hyperchromatic
nuclei, scant to moderate cytoplasms and occasional rosette-like
structures (15). However, pPNET of
the kidney must still be differentiated from other small round-cell
tumors, such as blastemal Wilms’ tumor, malignant lymphoma, small
cell carcinoma, rhabdomyosarcoma, poorly differentiated synovial
sarcoma and desmoplastic small round-cell tumors. Strong membranous
positivity for CD99 and nuclear staining of FLI1 are characteristic
features of pPNET; however, they are not definitive features, as
CD99 positivity is observed in ~99% of cases (8). Therefore, an immunohistochemical panel
consisting CD99, FLI1 and other relevant differential markers is
recommended (16). Blastemal Wilms’
tumor is typically observed in patients of a young age (<5
years) and is usually immunohistochemically positive for WT-1 to
various extents. Additionally, pPNET can be differentiated from
rhabdomyosarcoma, which is positive for desmin and myogenin, and
lymphoma, which may be excluded by immunostaining for LCA and other
lymphohematopoietic markers (16).
Genetically, pPNET of the kidney is characterized by
the chromosomal translocation t(11; 22)(q24;q12), resulting in the
production of the EWS/FLI1 fusion gene (17). The EWS gene on chromosome 22 encodes
an RNA-binding protein that is disrupted by the t(11;22)(q24;q12)
translocation. The FLI1 gene on 11q24 was the first EWS
translocation partner identified in the EWS/PNET family of tumors;
it is a member of a large family of DNA-binding transcription
factors that have a highly conserved 85-amino acid domain, termed
the erythroblastosis virus-transforming sequence (ETS) domain
(18). The resultant oncogenic
fusion gene includes the N-terminal transactivation domain of EWS
and the C-terminal DNA activation domain of FLI1, which acts as a
powerful transcriptional activator (16). Furthermore, a recent study
identified an association between CD99 overexpression and EWS/FLI1
fusion: EWS/FLI1 may downregulate microRNAs (miR), such as
miR-30-5p, which may interact with the 3′-untranslated region of
CD99 and post-transcriptionally downregulate its expression
(19). Additionally, alternative
chromosomal translocations with analogous fusion of EWS to other
partners have been reported; for example, the rare
t(16;21)(p11;q22) translocation and fusion of the ETS-related gene
ETS domain to fused in sarcoma has previously been reported in
renal pPNET (20). Thus, FISH with
negative EWS-FLI1 fusion only cannot completely exclude the
diagnosis of pPNET of the kidney (20,21).
pPNET of the kidney is an aggressive tumor with a
poor prognosis; a previous study identified that 25–50% of patients
presented with metastases and the five-year disease-free survival
rate was ~45–55% (22). A review of
116 reported cases of renal pPNET demonstrated consistent results;
33% of patients exhibited metastases at diagnosis and 40% of
patients developed metastases following surgery for the primary
tumor (8). Treatment strategies for
renal pPNET are similar to those for Ewing’s sarcoma, requiring
systemic chemotherapy in conjunction with surgery or radiotherapy
or both modalities for local tumor control. The benefit of
radiotherapy is not clear, however, it may be preferable in locally
advanced disease or in cases with Gerota’s fascia involvement
(23). Since the cases of patients
aged >50 years are rare, no consensus of a recommended treatment
strategy has been documented.
In conclusion, although pPNET of the kidney
typically occurs in young adults, it has also been reported to
occur in older patients. Immunohistochemistry for CD99, FLI1 and
other differential markers, as well as FISH analysis for EWSR1
fusion are key in the diagnosis of renal pPNET, which should be
included in the differential diagnosis of small-cell kidney tumors
in all age groups.
Acknowledgements
The authors thank Dr Hongying Zhang for performing
the FISH analysis. The present study was supported by grants from
the National Science Foundation of China (grant nos. 81272820,
81272824, 81101529 and 81100148).
Abbreviations:
|
pPNET
|
peripheral primitive neuroectodermal
tumor
|
|
ES
|
Ewing’s sarcoma
|
|
USG
|
ultrasonography
|
|
CT
|
computerized tomography
|
|
FISH
|
fluorescent in situ
hybridization
|
|
IHC
|
immunohistochemistry
|
References
|
1
|
Marley EF, Liapis H, Humphrey PA, et al:
Primitive neuroectodermal tumor of the kidney - another enigma: a
pathologic, immunohistochemical, and molecular diagnostic study. Am
J Surg Pathol. 21:354–359. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Howe HL, Wu X, Ries LA, et al: Annual
report to the nation on the status of cancer, 1975–2003, featuring
cancer among U.S. Hispanic/Latino populations. Cancer.
107:1711–1742. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tsokos M, Alaggio RD, Dehner LP and
Dickman PS: Ewing sarcoma/peripheral primitive neuroectodermal
tumor and related tumors. Pediatr Dev Pathol. (Suppl 1)15:108–126.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Movahedi-Lankarani S, Hruban RH, Westra WH
and Klimstra DS: Primitive neuroectodermal tumors of the pancreas:
a report of seven cases of a rare neoplasm. Am J Surg Pathol.
26:1040–1047. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mani S, Dutta D and De BK: Primitive
neuroectodermal tumor of the liver: a case report. Japanese J Clin
Oncol. 40:258–262. 2010. View Article : Google Scholar
|
|
6
|
Seemayer TA, Thelmo WL, Bolande RP and
Wiglesworth FW: Peripheral neuroectodermal tumors. Perspect Pediatr
Pathol. 2:151–172. 1975.PubMed/NCBI
|
|
7
|
Zöllner S, Dirksen U, Jürgens H and Ranft
A: Renal Ewing tumors. Ann Oncol. 24:2455–2461. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Risi E, Iacovelli R, Altavilla A, et al:
Clinical and pathological features of primary neuroectodermal
tumor/Ewing sarcoma of the kidney. Urology. 82:382–386. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jimenez RE, Folpe AL and Lapham RL:
Primary Ewing’s sarcoma/primitive neuroectodermal tumor of the
kidney: a clinicopathologic and immunohistochemical analysis of 11
cases. Am J Surg Pathol. 26:320–327. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Eggers H, Waalkes S, von Klot C,
Trankenschuh W, Merseburger AS and Herrmann TR: Ewing’s sarcoma of
the kidneys with simultaneous seminoma. Urologe A. 50:205–207.
2011.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tariq Z, Ghose A, Sofi A, Mohamed I and
Harmon D: Metastatic renal extraskeletal Ewing sarcoma in complete
remission for the last 8 years. Am J Ther. 19:120–121. 2012.
View Article : Google Scholar
|
|
12
|
Mandal PK, Mukherjee S, Roy S and
Bhattacharyya NK: PNET of kidney: Report of four cases. Indian J
Med Paediatr Oncol. 33:130–133. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wedde TB, Lobmaier IV, Brennhovd B, Lohne
F and Hall KS: Primary Ewing’s sarcoma of the kidney in a
73-year-old man. Sarcoma. 2011:9783192011. View Article : Google Scholar
|
|
14
|
Koski ME, Tedesco JM and Clark PE: Renal
peripheral neuroectodermal tumor presenting at age 78: case report.
Scientific World Journal. 8:830–834. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Parham DM, Roloson GJ, Feely M, Green DM,
Bridge JA and Beckwith JB: Primary malignant neuroepithelial tumors
of the kidney: a clinicopathologic analysis of 146 adult and
pediatric cases from the National Wilms’ Tumor Study Group
Pathology Center. Am J Surg Pathol. 25:133–146. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Saxena R, Sait S and Mhawech-Fauceglia P:
Ewing sarcoma/primitive neuroectodermal tumor of the kidney: a case
report. Diagnosed by immunohistochemistry and molecular analysis.
Ann Diagn Pathol. 10:363–366. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sorensen PH, Liu XF, Delattre O, et al:
Reverse transcriptase PCR amplification of EWS/FLI-1 fusion
transcripts as a diagnostic test for peripheral primitive
neuroectodermal tumors of childhood. Diagn Mol Pathol. 2:147–157.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wasylyk B, Hahn SL and Giovane A: The Ets
family of transcription factors. Eur J Biochem. 211:7–18. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Franzetti GA, Laud-Duval K, Bellanger D,
Stern MH, Sastre-Garau X and Delattre O: MiR-30a-5p connects
EWS-FLI1 and CD99, two major therapeutic targets in Ewing tumor.
Oncogene. 32:3915–3921. 2013. View Article : Google Scholar
|
|
20
|
Berg T, Kalsaas AH, Buechner J and Busund
LT: Ewing sarcoma-peripheral neuroectodermal tumor of the kidney
with a FUS-ERG fusion transcript. Cancer Genet Cytogenet.
194:53–57. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Angel J, Alfred A, Sakhuja A, Sells RE and
Zechlinkski JJ: Ewing’s sarcoma of the kidney. Int J Clin Oncol.
15:314–318. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ishii H and Ogaki K: Primitive
neuroectodermal tumor of the kidney. Med Mol Morphol. 42:175–179.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Thyavihally YB, Tongaonkar HB, Gupta S, et
al: Primitive neuroectodermal tumor of the kidney: a single
institute series of 16 patients. Urology. 71:292–296. 2008.
View Article : Google Scholar : PubMed/NCBI
|