Introduction
Cutaneous metastasis from internal malignancy is
relatively uncommon, with a reported frequency varying between 0.7%
and 9%, among which breast, lung, oral mucosa and colorectal cancer
are most likely to metastasize to the skin (1). Cutaneous involvement from gastric
carcinoma is even rarer (1–3) and usually arises in the vicinity of
the primary tumor (such as the abdominal wall) as non-specific
nodules (4).
The scalp is an unusual site of cutaneous
metastasis. Brownstein and Helwig previously reported that scalp
metastasis accounts for 4% of all skin metastases (5). Gastric cancer metastatic to the scalp
is extremely rare with few cases reported to date (6–9). The
current report presents a case of scalp metastasis from gastric
cancer and a review of the related literature in order to provide
new insights into the diagnosis, treatment and prognosis of such
cases in future. Patient provided written informed consent.
Case report
A 41-year-old female patient was admitted to the
Department of Medical Oncology, Cancer Institute/Hospital, Chinese
Academy of Medical Sciences (Beijing, China) on July 21, 2010 due
to complaints of upper abdominal pain for 10 months and lower back
pain for three months. The patient’s Karnofsky Performance Status
score was 90. No skin rash or plaque was observed on general
physical examination. Multiple enlarged lymph nodes were palpable
in bilateral cervical and supraclavicular regions, and chest
palpation revealed tenderness over the seventh right rib. The
abdomen was soft without palpable organomegaly. No point tenderness
was identified under the xiphoid upon palpitation without muscle
guarding or rebound tenderness. Complete blood count showed anemia
(hemoglobin levels, 102 g/l), biochemistry tests were within the
normal ranges and certain serum biomarker levels were elevated
(CA19-9, 156.4 U/ml; CA72-4, 1,292 U/ml; CEA, within the normal
range). Gastroscopy revealed a 1.0×1.2-cm submucosal lesion along
the greater curvature of the gastric body. Pathological biopsy of
the gastric lesion showed signet ring cell carcinoma and HER-2
staining was negative in tumor cells. Pathological biopsy of the
supraclavicular lymph nodes showed metastatic carcinoma. Computed
tomography (CT) scan from the neck to the pelvis revealed enlarged
lymph nodes in the cervical, supraclavicular, mediastinal, hilar,
perigastric and retroperitoneal regions, in addition to thickening
of the gastric wall, bilateral ovarian metastases, pericardial
effusion, bilateral pleural effusion and ascites. Radionuclide bone
scan showed multiple bone metastases. Based on the previously
described observations, the diagnosis of stage IV gastric signet
ring cell carcinoma was determined. Between July 2010 and December
2010, the patient received 11 cycles of systemic chemotherapy using
docetaxel (40 mg/m2d1), oxaliplatin (85
mg/m2d2) and 5-fluorouracil (400
mg/m2 bolus on days two and three plus 600
mg/m2 continuous intravenous infusion over 22 h on day
one, twice every two weeks). During the interval of the second
cycle of chemotherapy, the patient received local radiotherapy to
the rib metastatic site due to unrelieved pains. The adverse
effects of the chemotherapy included grade II gastrointestinal
reactions, grade II thrombocytopenia and grade III neutropenia.
Following four cycles of chemotherapy, the patient achieved partial
response according to the RECIST guidelines (version 1.1) (10) and the results were confirmed
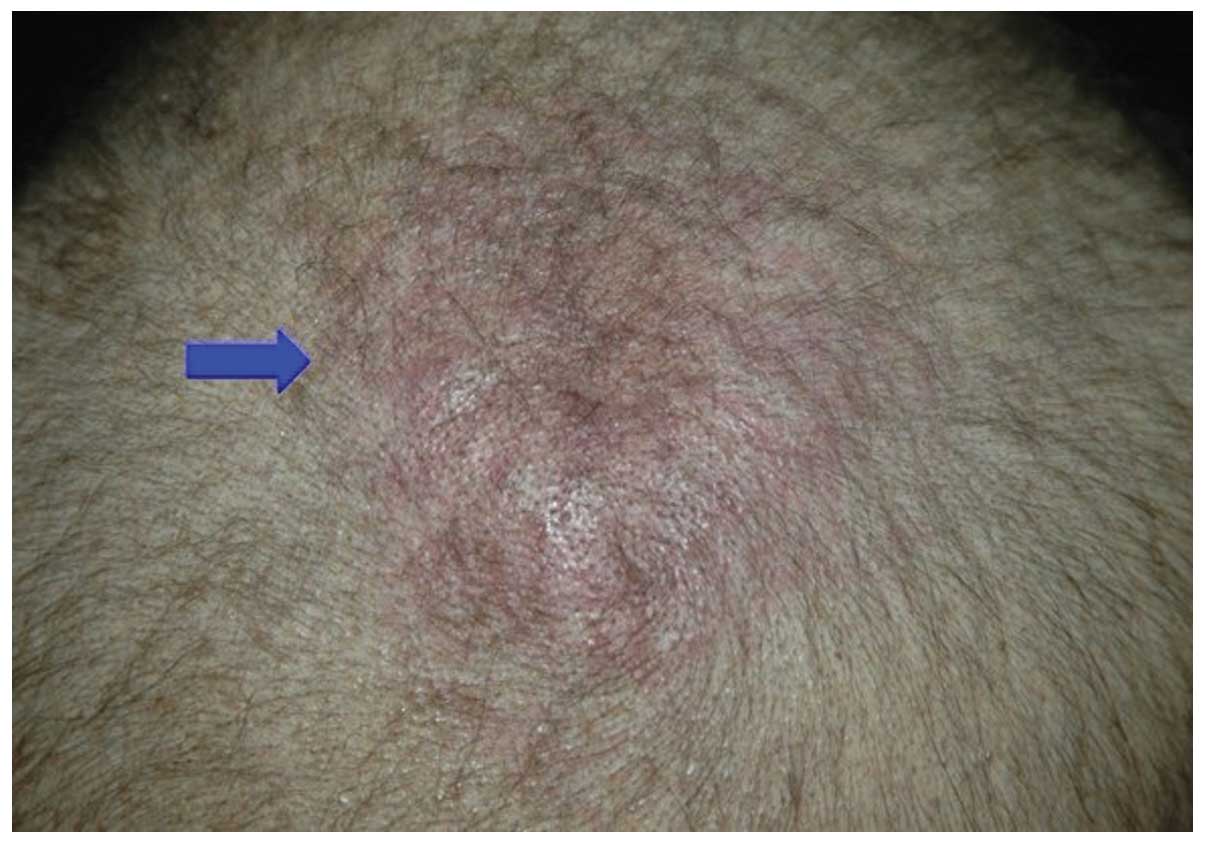
following eight cycles. In early December 2010, the patient
complained of pain in the scalp. Physical examination revealed a
pink lesion measuring 3×3 cm2 on the scalp over the
parietal region, with slight tenderness (Fig. 1). Further inquiry into the patient’s
past history indicated a similar ‘skin disease’ at the same site
several years previously, which had been cured by specific
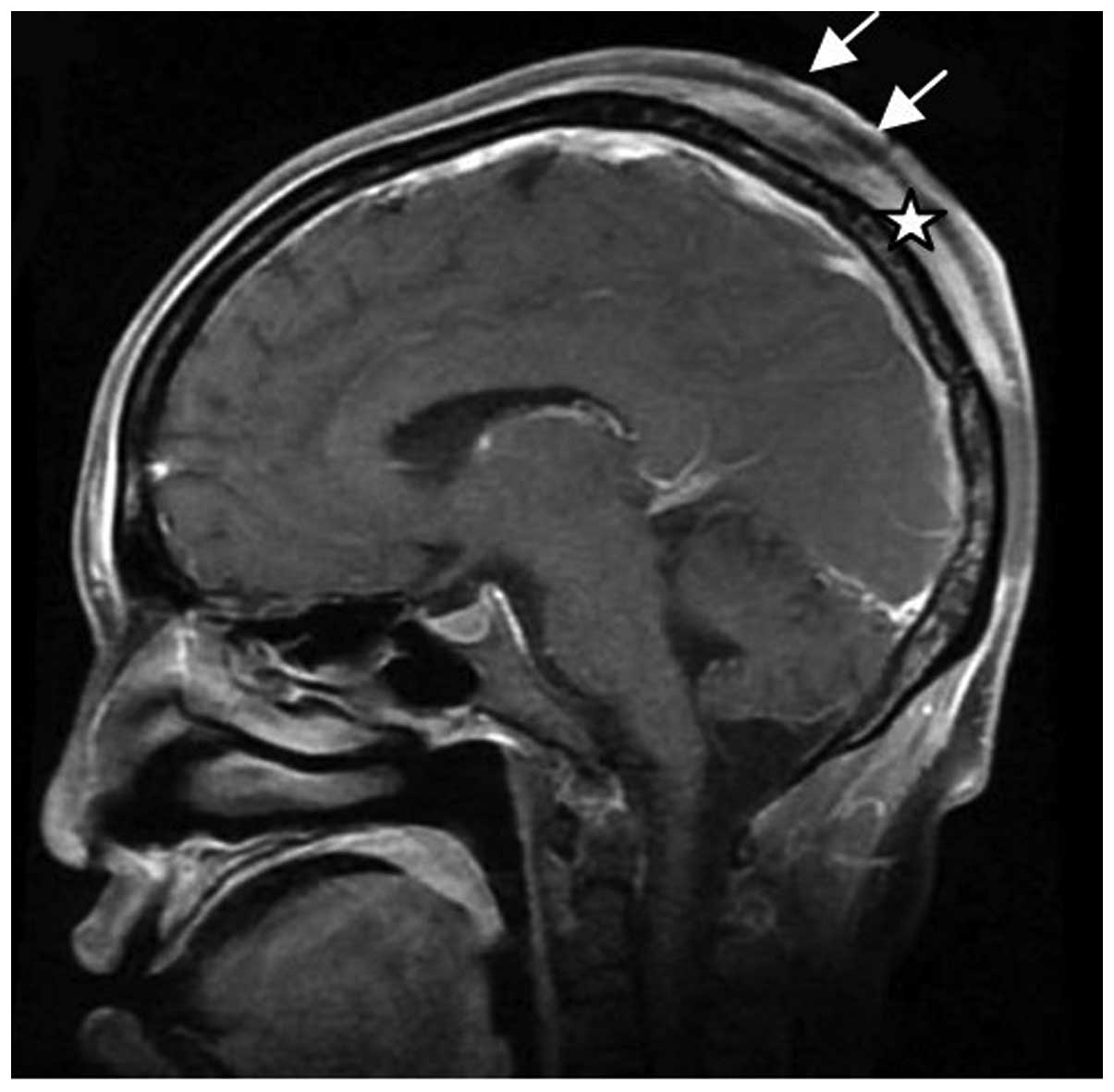
dermatologic drugs. Plain skull magnetic resonance imaging (MRI)
scan showed local thickening of the subparietal galea aponeurotica
(Fig. 2). The patient refused
further examination. The patient’s follow-up at our department for
regular chemotherapy found that the scalp lesion had increased in
size (12×13 cm2) and become darker and ulcerated
(Fig. 3). Therefore, the patient
was referred to the dermatology clinic. Pathological biopsy of the
lesion revealed tumor emboli in small vessels (Fig. 4). On January 21, 2011, the patient
complained of sickness, vertigo and diplopia. The patient was
admitted to our emergency room on January 24, 2011, and cranial MRI
revealed scalp and dural metastases (Fig. 5). The patient was treated with
mannitol and prednisolone to control intracranial hypertension.
However, the symptoms were uncontrollable and the patient succumbed
to the disease two days later.
We also performed a review of the associated
literature. PubMed was searched using the key words ‘gastric
cancer’, ‘cutaneous metastasis’ and ‘scalp’. The reference articles
of the search results were screened and five case reports were
found concerning scalp metastasis from gastric cancer, one of which
was written in Spanish without availability of the English abstract
and, therefore, was excluded from the study (Table I).
 | Table IScalp metastasis from gastric
carcinoma: review of the literature. |
Table I
Scalp metastasis from gastric
carcinoma: review of the literature.
| First author (year)
[ref] | Age, years | Gender | First sign of gastric
cancer | Site of cutaneous
metastasis | Synchronous
metastases | Time between scalp
lesion identification and diagnosis, months | Time between
diagnosis of scalp metastasis and mortality, months | Therapy following
diagnosis of scalp metastasis | Response to
therapy |
|---|
| Sakaki (1979)
[9] | 53 | Female | N | Scalp | Dural and lymph
nodes | 0 | 1 | Surgery | Patient succumbed to
the disease 5 days following surgery |
| Kim (1999) [8] | 36 | Female | N | Scalp | Pelvis | 10 | 2 | No | - |
| Lifshitz (2005)
[7] | 73 | Male | N | Upper forehead and
scalp | Not found | 4 | 7 | Localized IL-2
treatment of the scalp lesion and radiotherapy | The plaques decreased
in size following radiotherapy |
| Frey (2009) [6] | 54 | Male | Y | Scalp | Lung, liver and lymph
nodes | 4 | >12a | Chemotherapy
(docetaxel, cisplatin and 5-fluorouracil) | Scalp nodules
disappeared and the primary tumor regressed |
| Present case
(2011) | 41 | Female | N | Scalp | Lung, bone and lymph
nodes | 1 | 1 | No | - |
Discussion
Scalp metastasis is a rare occurrence in <2% of
patients with malignant metastases. Lung cancer (23.53%) has been
recognized as the primary tumor most frequently metastasizing to
the scalp, followed by colorectal (11.76%), liver (7.84%) and
breast (7.84%) cancer. Notably, metastatic tumors of undetermined
origin accounted for 29.41% of all metastatic scalp tumors
(11).
Scalp metastatic lesions may grow unnoticed for a
long period of time, manifesting as atypical nodules or plaques, or
alopecia neoplastica in even rarer cases (8). As scalp metastasis lacks
characteristic clinical presentations, it is often overlooked as an
ordinary skin disease, which is the main reason for delayed
diagnosis and treatment. According to the previous literature, a
number of patients remain undiagnosed until 4–10 months following
the identification of scalp lesions (6–8). In
the present case report, the diagnosis of the scalp lesion was
delayed for several weeks due to the confusing history of ‘skin
disease’ and incompliance of the patient. Therefore, it is
necessary to establish a full evaluation of any cutaneous lesion in
patients with internal malignancies, and pathological biopsy is
recommended.
Cutaneous metastasis portends a poor prognosis. The
mean survival for patients with cutaneous metastasis ranges between
one and 34 months depending on the tumor type (2). The majority of patients with cutaneous
metastasis from primary lung, cervical or esophageal cancer succumb
to their diseases three months after the development of cutaneous
metastases. In three of the four previously reported cases of
gastric cancer metastatic to the skin, the mean survival time was
one month (2), while the survival
time of the other patient remains unknown due to loss to follow-up.
Similarly, the median survival time was two months in the three
patients with gastric cancer following diagnosis of scalp
metastases (as shown in Table
I).
Cutaneous metastatic lesions often occur in the
final stage of cancer, indicating that underlying cancer has spread
extensively. The majority of patients exhibit concomitant
metastases to other organs. Extensive radiological evaluations,
including CT, MRI and positron emission tomography-CT, may provide
more valuable information. Systemic chemotherapy is recommended as
the major treatment (2,3). Previously, Frey et al reported
a patient with cutaneous metastasis from gastric cancer who
responded well to systemic chemotherapy and survived for >12
months (6). In cases where scalp
lesions induce uncontrolled symptoms, such as pain, or appear as
the only metastatic site, local excision/radiotherapy may be
considered. However, no significant change in survival has been
previously reported with any particular treatment available.
The present case report and review of the literature
demonstrated the rarity of scalp metastasis in gastric cancer.
Although cutaneous lesions usually reflect a more widely spreading
disease, they may also present as the first sign of cancer. For
patients with known internal malignancies, skin lesions often
require further evaluation. Pathological biopsy must be performed
when necessary. Extensive evaluations, including general physical
examination and further radiological examination, are important for
such patients. Scalp metastasis often indicates a grave prognosis
with a mean survival time of less than three months. Systemic
chemotherapy is the major treatment, but no particular treatment
has been previously reported to change survival rates.
References
|
1
|
Hu SC, Chen GS, Wu CS, Chai CY, Chen WT
and Lan CC: Rates of cutaneous metastases from different internal
malignancies: experience from a Taiwanese medical center. J Am Acad
Dermatol. 60:379–387. 2009. View Article : Google Scholar
|
|
2
|
Lookingbill DP, Spangler N and Helm KF:
Cutaneous metastases in patients with metastatic carcinoma: a
retrospective study of 4020 patients. J Am Acad Dermatol.
29:228–236. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lookingbill DP, Spangler N and Sexton FM:
Skin involvement as the presenting sign of internal carcinoma. A
retrospective study of 7316 cancer patients. J Am Acad Dermatol.
22:19–26. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Navarro V, Ramón D, Calduch L, Llombart B,
Monteagudo C and Jordá E: Cutaneous metastasis of gastric
adenocarcinoma: an unusual clinical presentation. Eur J Dermatol.
12:85–87. 2002.PubMed/NCBI
|
|
5
|
Brownstein MH and Helwig EB: Patterns of
cutaneous metastases. Arch Dermatol. 105:862–868. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Frey L, Vetter-Kauczok C, Gesierich A,
Bröcker EB and Ugurel S: Cutaneous metastases as the first clinical
sign of metastatic gastric carcinoma. J Dtsch Dermatol Ges.
7:893–895. 2009.PubMed/NCBI
|
|
7
|
Lifshitz OH, Berlin JM, Taylor JS and
Bergfeld WF: Metastatic gastric adenocarcinoma presenting as an
enlarging plaque on the scalp. Cutis. 76:194–196. 2005.PubMed/NCBI
|
|
8
|
Kim HJ, Min HG and Lee ES: Alopecia
neoplastica in a patient with gastric carcinoma. Br J Dermatol.
141:1122–1124. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sakaki S, Mori Y, Matsuoka K, Ohnishi T
and Bitoh S: Metastatic dural carcinomatosis secondary to gastric
cancer. Neurol Med Chir (Tokyo). 19:39–44. 1979. View Article : Google Scholar
|
|
10
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar
|
|
11
|
Chiu CS, Lin CY, Kuo TT, et al: Malignant
cutaneous tumors of the scalp: a study of demographic
characteristics and histologic distributions of 398 Taiwanese
patients. J Am Acad Dermatol. 56:448–452. 2007. View Article : Google Scholar
|