Introduction
Tongue squamous cell carcinoma (TSCC) is the most
common form of malignant tumor of the oral cavity, and is ranked
seventh most common amongst all cancers globally (1). TSCC accounts for ~3% of all malignant
tumors. Although the incidence of TSCC is lower than that of other
malignant tumors, its anatomical site is unique in that it affects
the cheek, tongue, lips, palate, lower oral cavity, upper and lower
jaw, and other organs. Therefore, the physical and mental impact on
patients with TSCC must be addressed (2). Squamous carcinomas account for 90% of
all oral and maxillofacial malignant tumors (3). While beneficial to the majority of
patients, surgery, radiotherapy, chemotherapy and other traditional
treatments inevitably have a functional impact on the face, head,
neck and other organs. In addition, patients experience other
post-treatment difficulties in facial reshaping, speech and
ventilation, which have consequences for their quality of life.
Therefore, there is an urgent clinical requirement to develop a
safe and effective novel treatment that differs from the
traditional methods.
Photodynamic therapy (PDT) for the treatment of
tumors is a novel technique that has been developed in recent
decades. Subsequent to injection into the body, photosensitizer
selectively accumulates in tumor tissue. Upon excitation by an
appropriate light source, a photochemical reaction occurs in the
tumor tissues, producing reactive oxygen species (ROS) and other
toxic substances that can kill tumor cells. A number of novel types
of photosensitizer and corresponding laser systems have been
researched and developed, with high safety and effectiveness, and
minimal invasiveness. The use of such photosensitizers has
therefore become popular in the field of research and development
in recent years. At present, PDT has demonstrated a broad range of
therapeutic applications, including the treatment of macular
degeneration, skin diseases and cancer. In the present study, the
photodynamic effect of the second-generation photosensitizer,
chlorin e6 (Ce6), on the human TSCC Tca8113 cell line was
investigated to provide an experimental basis for research in the
body.
Materials and methods
Cell cultures and reagents
Ce6 was purchased from Frontier Scientific (Logan,
UT, USA), and its basic molecular structure is shown in Fig. 1A. The human TSCC Tca8113 cell line
was provided by the Third Military Medical University (Chongqing,
China). The Tca8113 cells were cultured in Dulbecco’s modified
Eagle’s medium and 10% fetal calf serum, supplemented with 100 U/ml
streptomycin and 100 U/ml penicillin (all Gibco, Carlsbad, CA,
USA). The trypsin and Annexin V fluorescein isothiocyanate
(FITC)/propidium iodide (PI) apoptosis detection kit were purchased
from Sigma (St. Louis, MO, USA). The mitochondrial (ab112143) and
lysosomal (ab112137) probes were purchased from Abcam (Cambridge,
UK). The MTS kit was purchased from Promega (Madison, WI, USA). The
96- and 6-well plates, 50-ml flasks and 35-mm cell culture dishes
were purchased from Corning Costar (Amsterdam, the Netherlands),
the 35-mm glass-bottomed culture dish was purchased from Nest
(Wuxi, China) and the phosphate-buffered saline (PBS) was purchased
from Serva Electrophoresis GmbH (Heidelberg, Germany).
Method
Photosensitizer preparation
In sterile conditions, a 160-μg/ml stock solution
was prepared by dissolving Ce6 powder in PBS at pH 7.4. This was
stored at 4°C in the dark for subsequent use. For the study, the
stock solution was diluted into a working solution at corresponding
concentrations, as stated later.
Uptake of photosensitizer
In total, 10,000 Tca8113 cells were pre-treated with
40 μg/ml Ce6 for 30 min to 5 h in a glass-bottomed culture dish.
The photosensitizer-containing culture medium was disposed of.
Subsequent to washing twice with PBS, mitochondrial and lysosomal
probes were added to the dishes. Fluorescence images were collected
using a confocal laser-scanning microscope (UltraView VOX;
PerkinElmer, Waltham, MA, USA). The excitation wavelengths were 405
nm (Ce6), 488 nm (mitochondrial probe) and 561 nm (lysosomal
probe).
Laser irradiation
In total, 5,000 Tca8113 cells were seeded into the
96-well culture plates, or 6×105/well in the 6-well
plates/35-mm dishes. The cells were pre-treated with 0.5–20 μg/ml
Ce6 for 3 h in the 37°C incubator, then washed twice with PBS and
incubated for a further 30 min. The cells were then illuminated in
a dark room for 5–150 sec with a LD630 semiconductor diode laser
light, provided by the Laser Division of the People’s Liberation
Army General Hospital (Beijing, China), to achieve total light
doses of 0.5–15 J/cm2.
MTS assay
The assay was conducted according to the
instructions of the MTS test kit. Subsequent to treatment with
Ce6-PDT, the cells were incubated for 24 h in the 37°C incubator.
In total, 20 μl MTS reagent was added to each well. After 2 h, the
490-nm absorbance values were measured using an ELX-800UV plate
reader (BioTEK, Winooski, VT, USA).
Early apoptosis assessment by Annexin
V staining
The cells subjected to PDT were detached using 2.5%
trypsin (Gibco) 24 h after illumination. Early apoptosis was
assayed using the Annexin V-FITC/PI apoptosis detection kit
according to the manufacturer’s instructions (Sigma). A FACSCalibur
flow cytometer (BD Biosciences, San Jose, CA, USA) was used for
analysis of the results.
DNA content detection
The detection of apoptosis was based on evaluating
the DNA content of the cells with the use of PI and flow cytometry.
At 24h post-treatment, the cells were collected, washed twice with
PBS, fixed with 70% ethanol overnight at 4°C, rinsed twice with PBS
again and then stained with 25 μg/ml PI for 30 min at 4°C. The cell
suspensions were analyzed with a FACSCalibur flow cytometer (BD
Biosciences).
Statistical analysis
All data are presented as the mean ± standard
deviation. Statistical comparisons were performed using the
Student’s t-test and one way analysis of variance using GraphPad
Prism version 5.01 software (GraphPad Software, San Diego, CA,
USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
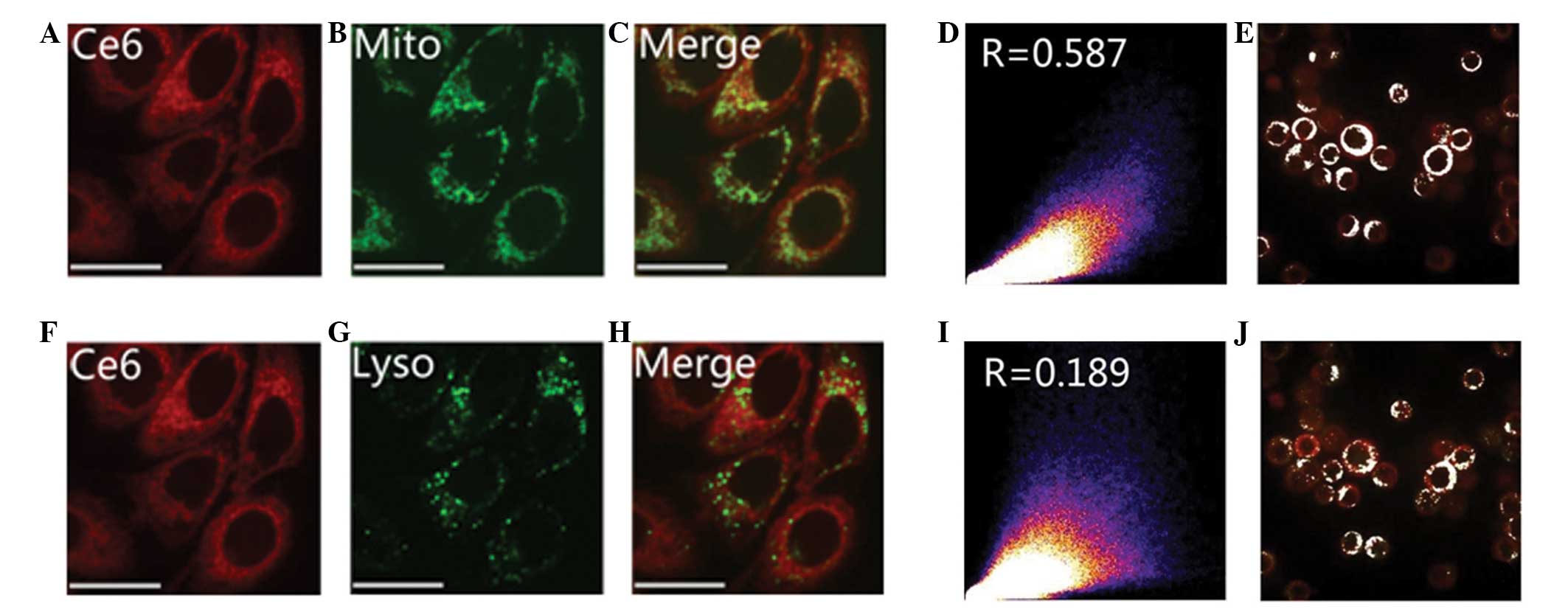
Ce6 is localized in Tca8113 cells
The intensity of Ce6 fluorescence gradually
increased with the extension of the co-incubation time. After 3 h,
the Ce6 fluorescence intensity stabilized. No statistically
significant difference was identified in the fluorescence intensity
between 3, 4 and 5 h (Fig. 1B). At
the beginning of photosensitizer uptake, the majority of Ce6 was
located around the cell membrane, with less observed in the
cytoplasm. As the incubation time increased, Ce6 was mainly
distributed granularly in the cytoplasm, with little observed in
the nucleus. The excitation wavelength of Ce6 was 405 nm (Fig. 1C–D). Fig. 2A–C and F–H demonstrate the cellular
location of Ce6 (red), the mitochondrial and lysosomal probes
(green) and the areas of co-localization (yellow) subsequent to 3 h
of co-incubation. In Fig. 2C, the
majority of the image appears yellow, with fewer areas of green
mitochondrial fluorescence. In Fig.
2H, however, there are more areas of distinct green lysosomal
fluorescence in the merged image. This demonstrates that the
majority of the mitochondria, and only a small number of lysosomes,
were co-localized with Ce6. The co-localization coefficient between
Ce6 and the mitochondria, and Ce6 and the lysosomes was >0.5 and
~0.2, respectively. These values demonstrate that Ce6 has a higher
co-localization with the mitochondria than with the lysosomes in
the Tca8113 cells (Fig. 2D, E, I and
J).
Ce6 dark toxicity on human TSCC Tca8113
cells
Using the colorimetric MTS assay, the toxicity of
Ce6 on the Tca8113 cells was analyzed by measuring dehydrogenase
enzyme activity. Subsequent to 24 h of incubation, 10 and 5 μg/ml
chlorin-e6 induced toxicities of <10% and 5%, respectively.
Considering that the Ce6 reached saturation density 3 h after
incubation (Fig. 1B), the MTS data
suggested that the safe drug dose for the following assays was ≤10
μg/ml (Fig. 3A), as it may
otherwise lead to dark toxicity.
Ce6 phototoxicity on Tca8113 cells
Subsequent to the MTS assay, the Tca8113 cells
incubated with different concentrations of Ce6 (range, 0.5 to 20
μg/ml) and light doses (range, 0.5–15 J/cm2) were
examined. The MTS assay demonstrated that illumination or treatment
with Ce6 alone does not induce significant cellular toxicity
(Fig. 3B and C). The Ce6-PDT
combination treatment demonstrated almost linear correlations with
light dose, Ce6 concentration and toxicity. Increasing the light
dose, from 0 to 15 J/cm2 in the cells treated with 2
μg/ml Ce6, led to a gradual increase in cellular toxicity
(P<0.05; Fig. 3B). Similarly,
when the same light dose of 2 J/cm2 was applied,
increasing the concentration of Ce6 from 5 to 20 μg/ml resulted in
a gradual increase in cellular toxicity (P<0.05; Fig. 3C). A cellular toxicity of ~80% was
observed following the use of 2 μg/ml Ce6 and a light dose of 5
J/cm2, conditions which were then applied to the
subsequent experiments.
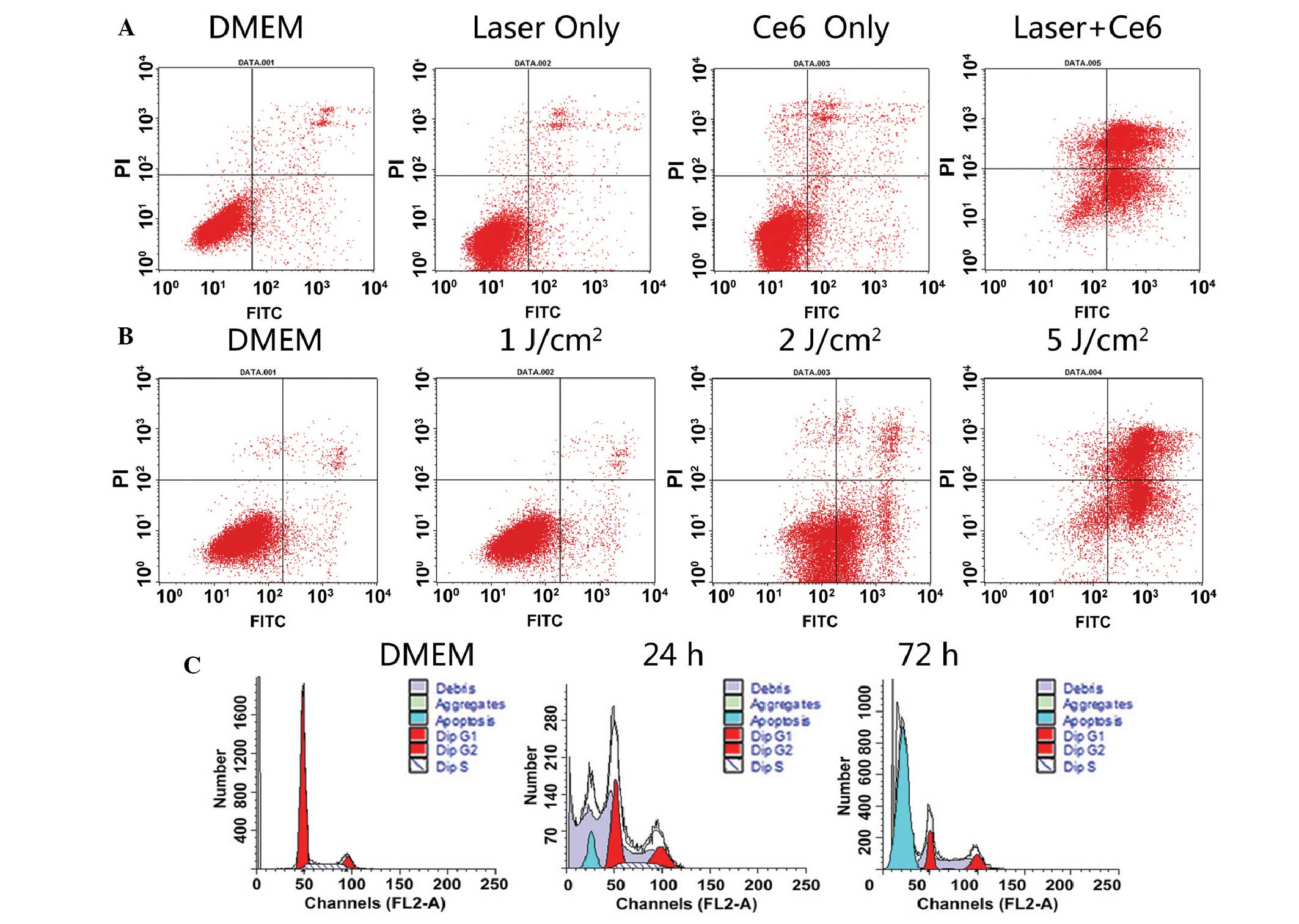
Apoptosis detection
Ce6 localized to the mitochondria and was excited by
the laser to produce ROS, which triggered cell necrosis and
apoptosis. It was observed that large doses of Ce6 caused necrosis,
while small doses initiated apoptosis. Post-PDT cell apoptosis was
detected using phosphatidylserine (PS) presentation and DNA
fragmentation (Fig. 4). The
apoptosis detection kit includes Annexin V-FITC and PI, and was
used to detect those cells undergoing early-stage apoptosis. During
the early stages of apoptosis, cells translocated to the membrane
PS from the inner face of the plasma membrane to the cell surface
and combined with Annexin V-FITC to produce green fluorescence,
while those cells not undergoing apoptosis were not stained. PI was
able to enter the dead cells and combine with the DNA to produce a
red fluorescence. In the late stages of apoptosis, the integrity of
the cell membrane was damaged, which enabled Annexin V and PI to
enter the cells. It was revealed that illumination of
Ce6-photosensitized cells led to an increase in the number of cells
that expressed PS (28% in Ce6-treated cells vs. 3% in controls).
Furthermore, an increase in Annexin V-PI double-positive and
PI-positive cells was observed, which suggested a reduction in the
integrity of the cell membrane (Fig.
4A). Similarly, increasing the light dose led to a gradual
increase in Annexin V-PI double-positive and PI-positive cells,
which suggested a decrease in the integrity of the cell membrane
(Fig. 4B). The application of
phototherapy or Ce6 alone had no observable impact on cellular
apoptosis and necrosis. The presence of DNA fragmentation is a
hallmark of apoptosis. In the present study, Ce6-PDT led to DNA
fragmentation in ~18% and ~79% of cells, 24 and 72 h after
illumination, respectively (Fig.
4C). This indicates that Ce6-PDT results in the classical
apoptosis of Tca8113 cells.
Discussion
The damage to normal tissue by PDT is mild and
avoids post-operative facial destruction or functional loss,
therefore, PDT has become attractive in recent years for its
therapeutic potential. In 1997, the Food and Drug Administration
(Silver Spring, MD, USA) listed PDT as one of the basic methods for
tumor treatment, alongside surgery, radiotherapy, chemotherapy and
biological immunity therapies. PDT as a treatment for cancer
patients has been successful in numerous countries, including the
United States, Japan, Britain, Germany, France and Canada, and has
been approved by a number of countries for a variety of tumor
therapies. PDT is clinically approved to treat certain types of
cancers, pre-malignant conditions and macular degeneration
(4–7). In addition to being effective for body
surface tumors, PDT has unique advantages in treating tumors of the
head and eyes, and the respiratory, gastrointestinal and urinary
tracts (8–10).
The exact molecular mechanism of Ce6-based PDT is
unclear. However, the production of ROS or singlet oxygen species,
and the initiation of endoplasmic reticulum stress and mitochondria
dysfunction, are the most common events in the process. These
events are believed to lead to the induction of cell-death
programs, including classical apoptosis and programmed necrosis or
autophagy (11).
Photosensitizers, lasers and tissue oxygen content
are three factors that enable PDT. The final effect is dependent on
the photosensitizer concentration, photosensitivity, characteristic
absorption spectra, extent of selective absorption of the
photosensitizer in the tumor tissue, light dose and tissue oxygen
supply. Ce6 is a type of chlorophyll degradation product with an
absorption spectrum of 600–800 nm and a maximum absorption
wavelength of 660 nm. Light-induced excitation at a long wavelength
can activate the photosensitizer in deep tumor tissues to generate
more efficacious treatment effects. The Ce6-PDT tissue penetration
depth has been reported to reach 16.6 mm (12). In addition, Ce6 has other
advantages, including a high yield of singlet oxygen, rapid
clearance in the body and a short accumulation time in the skin
(13).
The results of the present study suggested that Ce6
can produce a photodynamic effect on the Tca8113 cells, which
increases with Ce6 concentration and light dose. The light dose and
Ce6 concentration are positively correlated with PDT efficiency in
cell death. Furthermore, the 24 h dark cytotoxicity of Ce6 reaches
its limit at a concentration of 10 μg/ml (Fig. 3A). In addition, when Ce6 was
incubated with the cells for 3 h, a period sufficient for
saturation, almost no cytotoxicity was demonstrated (Fig. 3C). The experimental data revealed
that a Ce6 concentration of 2 μg/ml and a light dose of 1
J/cm2 induced no evident Ce6-PDT-mediated effect
(Fig. 3B). Similarly, a light dose
of 2 J/cm2 and a Ce6 concentration of <1 μg/ml
demonstrated almost no observable effect on cell viability.
Therefore, an ideal result of cellular toxicity with 82% of cells
apoptosed after 24 h can be achieved with 5 μg/ml Ce6 and a 2
J/cm2 laser dose, or 2 μg/ml Ce6 and a 5
J/cm2 laser dose. Luo and Kessell (14) demonstrated that when a certain
photosensitizer was introduced to cells, the mode of cell death of
either apoptosis or necrosis was functionally associated with the
light dose of PDT.
Ce6-PDT has been successful in the treatment of a
variety of tumors. Sheleg et al demonstrated that Ce6-PDT
achieved ideal results in patients with metastatic malignant
melanoma (15). Furthermore, it was
revealed that cellular toxicity was positively correlated with
increased Ce6 concentration. Low concentrations of <10 μg/ml Ce6
had no significant impact on cells, whilst at 20 μg/ml, >10% of
cells were killed. Therefore, the potential systemic damage caused
by Ce6 cytotoxicity should be carefully considered. Numerous
studies are analyzing complex forms of Ce6 and certain carriers
that increase the local drug concentration and weaken the
cytotoxicity (16–18).
In the present study, a preliminary observation was
made concerning the distribution of Ce6 in the Tca8113 cells. The
present study revealed that Ce6 was primarily distributed in
organelles in the plasma and nuclear membrane, indicating that the
injury of these sub-cellular organelles is a direct cause of
cellular damage. The localization of photosensitizer to the
mitochondria and lysosomes is generally accepted to lead to
apoptosis and necrosis, respectively. It was observed that Ce6-PDT
induced rapid mitochondrial destruction (see supplementary video
content online: http://www.56.com/u56/v_MTI5NDYyOTE3.html;
Morphological changes of mitochondria after Ce6-PDT). The Ce6,
mitochondria and lysosomes fluoresced red, green and blue,
respectively. Furthermore, yellow indicated the co-localization of
mitochondria and lysosomes with Ce6. The mitochondrial probe became
dispersive following photo-excitation, which indicated that the
mitochondria may be a sensitive target of Ce6-PDT.
In conclusion, using an in vitro PDT model
based on human TSCCs, the present study demonstrated that the
photosensitizer Ce6 may be useful in designing PDT for the
treatment of TSCC. However, the pharmacokinetics and cytotoxic
mechanisms of Ce6-PDT require further study in order to lay an
experimental foundation for future clinical use.
Acknowledgements
This study was supported in part by the Beijing
Natural Science Foundation of China (no. 7122174).
Abbreviations:
|
Ce6
|
chlorin e6
|
|
PDT
|
photodynamic therapy
|
|
TSCC
|
tongue squamous cell carcinoma
|
|
PI
|
propidium iodide
|
|
ROS
|
reactive oxygen species
|
|
CLSM
|
confocal laser scanning microscopy
|
References
|
1
|
Warnakulasuriya S: Global epidemiology of
oral and oropharyngeal cancer. Oral Oncol. 45:309–316. 2009.
View Article : Google Scholar
|
|
2
|
Gibson MK and Forastiere AA:
Multidisciplinary approaches in the management of advanced head and
neck tumors: state of the art. Curr Opin Oncol. 16:220–224. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Neville BW and Day TA: Oral cancer and
precancerous lesions. CA Cancer J Clin. 52:195–215. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Biel MA: Photodynamic therapy treatment of
early oral and laryngeal cancers. Photochem Photobiol.
83:1063–1068. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fien SM and Oseroff AR: Photodynamic
therapy for non-melanoma skin cancer. J Natl Compr Canc Netw.
5:531–540. 2007.PubMed/NCBI
|
|
6
|
Taub AF: Photodynamic therapy: other uses.
Dermatol Clin. 25:101–109. 2007. View Article : Google Scholar
|
|
7
|
Woodburn KW, Fan Q, Kessel D, et al:
Photodynamic therapy of B16F10 murine melanoma with lutetium
texaphyrin. J Invest Dermatol. 110:746–751. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Malik R, Manocha A and Suresh DK:
Photodynamic therapy - a strategic review. Indian J Dent Res.
21:285–291. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Luketich JD, Christie NA, Buenaventura PO,
et al: Endoscopic photodynamic therapy for obstructing esophageal
cancer: 77 cases over a 2-year period. Surg Endosc. 14:653–657.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Walther MM: The role of photodynamic
therapy in the treatment of recurrent superficial bladder cancer.
Urol Clin North Am. 27:163–170. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Buytaert E, Dewaele M and Agostinis P:
Molecular effectors of multiple cell death pathways initiated by
photodynamic therapy. Biochim Biophys Acta. 1776:86–107.
2007.PubMed/NCBI
|
|
12
|
Kostenich GA, Zhuravkin IN, Furmanchuk AV
and Zhavrid EA: Photodynamic therapy with chlorin e6. A morphologic
study of tumor damage efficiency in experiment. J Photochem
Photobiol B. 11:307–318. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gijsens A, Missiaen L, Merlevede W and de
Witte P: Epidermal growth factor-mediated targeting of chlorin e6
selectively potentiates its photodynamic activity. Cancer Res.
60:2197–2202. 2000.PubMed/NCBI
|
|
14
|
Luo Y and Kessel D: Initiation of
apoptosis versus necrosis by photodynamic therapy with
chloroaluminum phthalocyanine. Photochem Photobiol. 66:479–483.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sheleg SV, Zhavrid EA, Khodina TV, et al:
Photodynamic therapy with chlorin e(6) for skin metastases of
melanoma. Photodermatol Photoimmunol Photomed. 20:21–26. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Efremenko AV, Ignatova AA, Borsheva AA, et
al: Cobalt bis(dicarbollide) versus closo-dodecaborate in boronated
chlorin e(6) conjugates: implications for photodynamic and
boron-neutron capture therapy. Photochem Photobiol Sci. 11:645–652.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kim JY, Choi WI, Kim M and Tae G:
Tumor-targeting nanogel that can function independently for both
photodynamic and photothermal therapy and its synergy from the
procedure of PDT followed by PTT. J Control Release. 171:113–121.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li Z, Wang C, Cheng L, et al:
PEG-functionalized iron oxide nanoclusters loaded with chlorin e6
for targeted, NIR light induced, photodynamic therapy.
Biomaterials. 34:9160–9170. 2013. View Article : Google Scholar : PubMed/NCBI
|