Abernethy malformation is an extremely rare
congenital vascular malformation that is characterized by the
diversion of portal blood away from the liver (1). It frequently comprises a number of
congenital anomalies of the liver, including congenital absence of
the portal vein (CAPV), portosystemic shunt, and liver nodules, as
well as congenital heart diseases such as atrial septal defect,
ventricular septal defect (VSD) and patent ductus arteriosus
(2).
The number of CAPV diagnoses has increased in recent
years due to advances in imaging techniques (3,4). To
the best of our knowledge, 101 cases of CAVP have been reported
since the condition was first described in 1793 (1), and the majority of affected patients
were <18 years of age and female (1,3–90).
Almost all adult patients in the reported cases that have been
reviewed in the present study were admitted to hospital with
various symptoms including nausea, vomiting, fatigue, epigastric
pain, asthenia, anorexia, jaundice and dyspnea (3–31). In
general, the treatment options for CAPV include surgical correction
of shunts, liver nodule resectioning and liver transplantation. The
outcome of CAPV in adults is good, and may be improved further by
adopting appropriate treatment strategies.
The current study reports the case of multiple focal
nodular hyperplasia (FNH) with CAPV in an asymptomatic adult male
patient of postoperative VSD status. Written informed consent was
obtained from the patient.
A 19-year-old male was admitted to the Endocrinology
Department, Beijing Friendship Hospital (Beijing, China), due to a
mildly elevated alanine transaminase level that had been
incidentally identified during a routine health examination. No
clinical evidence of encephalopathy or weight loss was observed.
Physical examination revealed no abnormalities with the exception
of mild jaundice and a diastolic murmur at the upper left sternal
border. The patient’s medical history included VSD and pulmonary
valve stenosis, and the patient had undergone surgical VSD repair
at 3 years of age. The mother also reported a mild viral infection
(a cold) in her early pregnancy, which may have affected early
fetal development.
Liver function testing showed an alanine
transaminase level of 51 U/l (normal, 0–40 U/l), a γ-glutamyl
transpeptidase level of 134 U/l (normal, 8–55 U/l), a total
bilirubin level of 52.46 μmol/l (normal, 3.42–17.1 μmol/l) and an
indirect bilirubin level of 36.83 μmol/l (normal, 0–12 μmol/l).
Routine blood tests and a reticulocyte analysis revealed a white
blood cell count of 6.8×109/l (normal range,
4.0–10.0×109/l), a neutrophil level of
3.6×109/l (normal range, 2.0–7.0×109/l), a
red blood cell count of 5.5×1012/l (normal range,
4.0–5.5×1012/l), a hemoglobin level of 167 g/l (normal
range, 120–160 g/l), platelet level of 226×109/l (normal
range, 100–300×109/l) and reticulocyte level of
0.02×1012/l (normal range, 0.01–0.09×1012/l).
No fragmented red blood cells were identified in the peripheral
blood. The coagulation profile was normal. Serological markers for
ceruloplasmin and hepatitis A–E viruses as well as immunological
markers were negative; α-fetoprotein was also negative.
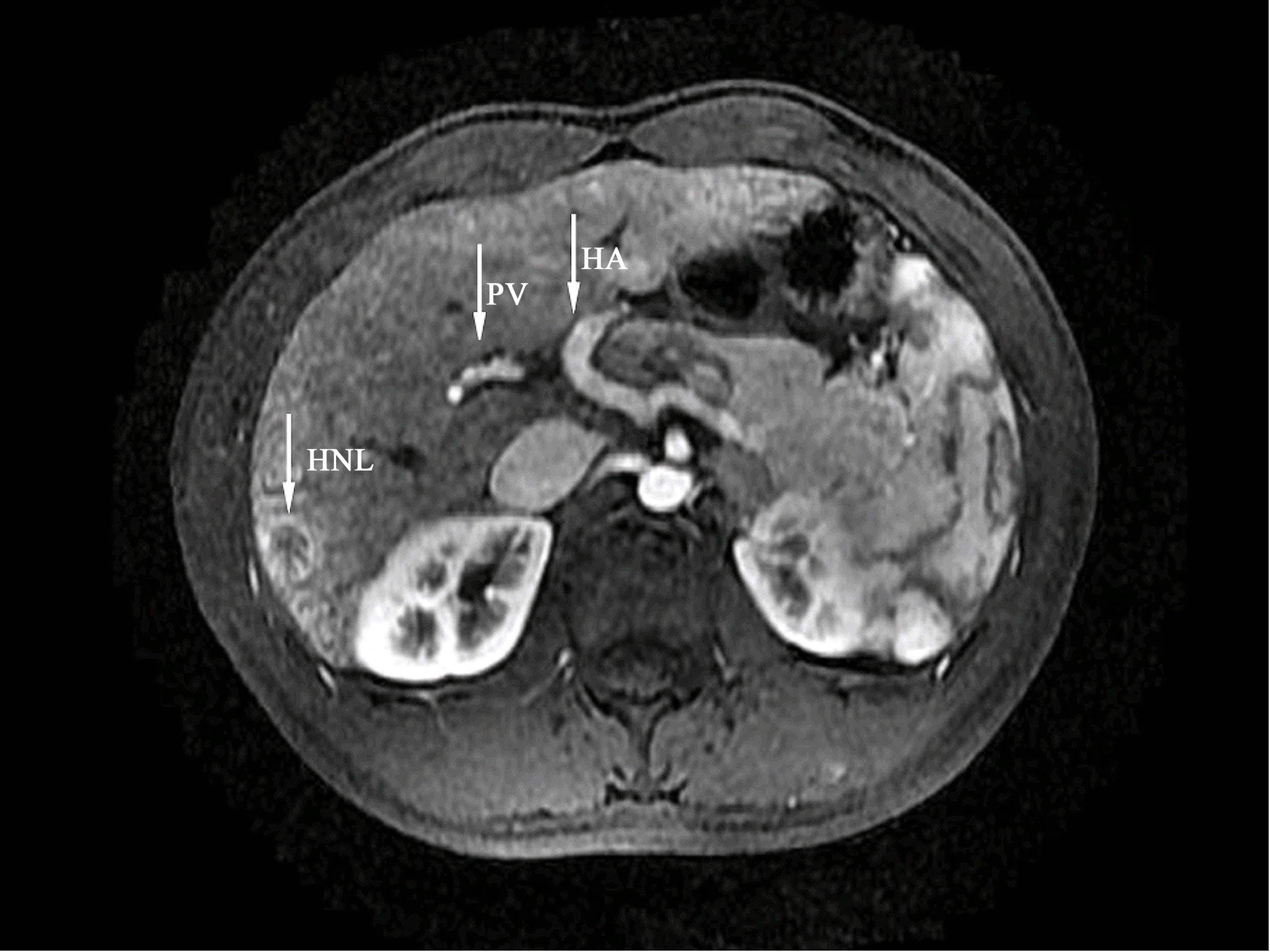
Abdominal ultrasonography revealed a number of
hypoechoic solid masses distributed in the right and left lobes of
the liver, and an enlarged spleen. A splenorenal shunt was also
detected. Magnetic resonance imaging was advised based on the
abdominal ultrasound findings (Fig.
1). Magnetic resonance imaging confirmed the presence of a
splenorenal shunt and multiple lesions with rich blood supplies. It
also showed that the portal vein was slender with unclear
branching. These findings led to the diagnosis of type II CAPV.
Percutaneous fine-needle aspiration biopsy of the
liver nodules was subsequently performed (Fig. 2). Pathological examination revealed
bile duct proliferation, hydropic degeneration of hepatocytes,
hyperplasia of thick-walled arterioles and fibrosis in the portal
area, but no intrahepatic cholestasis. The lesions were therefore
confirmed to be FNH.
Electrocardiography revealed a right bundle branch
block, and ultrasonic cardiography indicated congenital heart
disease, postoperative VSD status, pulmonary valve stenosis and
pulmonary regurgitation.
The term CAPV was first coined by John Abernethy in
1793. Congenital extrahepatic portosystemic shunt is also known as
Abernethy malformation in recognition of its initial identification
(1). Complete portosystemic shunts
that do not perfuse the liver via the portal vein are defined as
type I, whereas partial shunts with a remaining degree of portal
perfusion to the liver are defined as type II. Type I is further
subclassified into types Ia and Ib according to the course of the
splenic and mesenteric veins (32).
A number of patients with Abernethy malformation
have been previously described (1,3–89).
Among them, 66 were female and 35 were male, with ages ranging from
fetus to 61 years at the time of diagnosis. In total, 70 patients
(69.30%) were<18 years of age, and <10% had type II
malformations (45,58,75–77).
In the present case, imaging findings indicated that
the portal vein had formed by the union of the splenic and superior
mesenteric veins. These veins were present, but appeared slender
and hypoperfused as a portion of the blood was being diverted into
the inferior vena cava via a splenorenal shunt. Therefore, a
diagnosis of type II Abernethy malformation was determined.
In addition to the absence of the portal vein,
nodular liver lesions were observed in almost half of the reported
cases (48.51%). The association between portal vein agenesis and
nodular liver lesions is attributed to the absence of portal blood
flow and compensatory increased hepatic arterial blood flow.
Systemic shunting of the visceral venous return may lead to
abnormal development, malfunction and regeneration of the liver,
secondary to the absence of portal hepatotrophic factors, resulting
in the development of hepatic lesions (87). The majority of these lesions were
characterized as benign, such as FNH (36.73%). Other reported
lesions included nodular regenerated hyperplasia (16.33%),
hepatoblastoma (4.08%), hepatic adenoma (10.20%), hepatocellular
carcinoma (26.53%) and cirrhosis (6.12%). In the current review,
only a few patients with CAPV associated with FNH were male (8.16%;
Table I).
The patient in the present case was in reasonable
health following heart surgery and visited a doctor for the
evaluation of an abnormal result obtained during a regular health
examination. Although the patient felt no discomfort, the
ultrasonography report indicated a more serious condition.
Following a series of imaging examinations and a biopsy, malignant
lesions were ruled out and it was concluded that the characteristic
hepatic changes were secondary to the congenital malformation of
the portal vein, and were associated with congenital heart
disease.
Several known associations between primary liver
disease and concomitant congenital cardiac defects have been
identified (2). Congenital cardiac
diseases including atrial septal defect, patent foramen ovale, VSD
and patent ductus arteriosus are frequently observed concurrent
with CAPV. Congenital stenosis of the aortic valve and pulmonary
artery valve, observed in a number of patients with CAPV, can cause
tricuspid regurgitation (36,44,90).
However, it has also been hypothesized that systemic shunting of
portal venous flow could adversely affect hepatic and cardiac
development and function. Concomitant atrial and ventricular septal
defects associated with CAPV may be attributed to a congenital
adaptive change that occurs during development from the embryonic
stage, which tends to compensate for the congestive effects of
portal venous aplasia (2).
Another possible cause of vascular dysplasia is
viral infection in early pregnancy, as occurred in the present
case, where the patient’s mother reported a mild viral infection (a
cold) during early pregancy. Embryologically, the portal vein
originates from the paired vitelline veins. Between gestational
weeks four and five, the paired vitelline veins form three
anastomoses that, over the course of the first trimester, undergo
selective involution to produce the portal vein (91). Aberrations in this process of
involution may result in anatomical variations within the portal
system; specifically, excessive involution may result in the
absence of the portal vein. Almost simultaneously, a wall forms,
separating the right and left ventricles. If the wall does not
completely form, a hole remains. This hole is known as a VSD. Any
abnormality in this process of involution may lead to VSD.
Among the reported cases, 46 cases associated with a
variety of congenital anomalies were identified (92). In addition to the aforementioned
congenital cardiac disease (16/46; 34.78%), other types of
dysplasia involved the kidney (6/46; 13.04%), spleen (5/46;
10.87%), bone (4/46; 8.70%), arteries (3/46; 6.52%), bile duct
(3/46; 6.52%), nervous system (2/46; 4.35%), urethra (1/46; 2.17%)
and endocrine glands (1/46; 2.17%). In addition, a number of
patients were affected by Turner syndrome (2/46; 4.35%), Caroli
syndrome (1/46; 2.17%), Goldenhar syndrome (1/46; 2.17%) and Down
syndrome (1/46; 2.17%; Table
I).
The type of CAPV and simultaneous presence of
congenital anomalies are the key factors in determining the
severity of a given patient’s pathogenetic condition and the course
of the disease. Furthermore, the mode of management should be
established on a case-by-case basis, according to the type or
anatomy of the disease, in addition to the symptoms and clinical
condition of the patient.
Treatments may include liver transplantation,
balloon-occluded retrograde transvenous obliteration, embolization
with metallic coils and surgical correction of shunts (93). In patients with type II
malformations previously diagnosed with CAPV, occlusion of the
shunt is indicated in cases with serious symptoms such as hepatic
encephalopathy (43) or lateral
bleeding. In the present case, the patient was asymptomatic, and
the physical examination findings and laboratory test results
appeared normal. Thus, we propose that close clinical, biochemical,
and imaging follow-up must be performed and that interventional
treatment should not be immediately conducted.
In conclusion, the diagnosis of Abernethy
malformation and its associated anomalies is challenging. It is
important not only to detect portal vein malformation, but also to
identify other important associated anomalies, due to the variable
clinical consequences. It appears that the long-term prognosis
hinges on adequate control of the hepatic dysfunction and metabolic
derangements; however, only longitudinal follow-up of these
patients will provide further insight.
The authors would like to thank Dr HengChi Yu and Dr
WeiJia Duan for their help with the document retrieval work. And we
also thank Dr YaoEr Cheng for her valuable technical assistance in
selecting the imaging figure.
|
1
|
Abernethy J and Banks J: Account of two
instances of uncommon formation in the viscera of the human body.
Philos Trans R Soc Lond. 83:59–66. 1793. View Article : Google Scholar
|
|
2
|
Asrani SK, Asrani NS, Freese DK, et al:
Congenital heart disease and the liver. Hepatology. 56:1160–1169.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schaeffer DF, Laiq S, Jang HJ, John R and
Adeyi OA: Abernethy malformation type II with nephrotic syndrome
and other multisystemic presentation: an illustrative case for
understanding pathogenesis of extrahepatic complication of
congenital portosystemic shunt. Hum Pathol. 44:432–437. 2013.
View Article : Google Scholar
|
|
4
|
Witjes CD, Ijzermans JN, Vonk Noordegraaf
A and Tran TK: Management strategy after diagnosis of Abernethy
malformation: a case report. J Med Case Rep. 6:1672012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Daddi G, Cozzi M and Pardi G:
Anatomo-pathological considerations on a case of congenital
stenosis of the portal vein. Folia Hered Pathol (Milano).
15:1121965.(in Italian).
|
|
6
|
Motoori S, Shinozaki M, Goto N and Kondo
F: Case report: congenital absence of the portal vein associated
with nodular hyperplasia in the liver. J Gastroenterol Hepatol.
12:639–643. 1997. View Article : Google Scholar
|
|
7
|
Matsuoka Y, Ohtomo K, Okubo T, Nishikawa
J, Mine T and Ohno S: Congenital absence of the portal vein.
Gastrointest Radiol. 17:31–33. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arana E, Martí-Bonmatí L, Martinez V,
Hoyos M and Montes H: Portal vein absence and nodular regenerative
hyperplasia of the liver with giant inferior mesenteric vein. Abdom
Imaging. 22:506–508. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Northrup M, Mendez-Castillo A, Sethi Y and
Churchill R: Congenital absence of the portal vein with an
intrahepatic inferior vena cava branch showing hepatopetal flow. J
Ultrasound Med. 21:569–572. 2002.PubMed/NCBI
|
|
10
|
Lundstedt C, Lindell G, Tranberg KG and
Svartholm E: Congenital absence of the intrahepatic portion of the
portal vein in an adult male resected for hepatocellular carcinoma.
Eur Radiol. 11:2228–2231. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
De Gaetano AM, Gui B, Macis G, Manfredi R
and Di Stasi C: Congenital absence of the portal vein associated
with focal nodular hyperplasia in the liver in an adult woman:
imaging and review of the literature. Abdom Imaging. 29:455–459.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Appel H, Loddenkemper C, Schirmacher P, et
al: Congenital absence of the portal vein with splenomegaly and
hypersplenism in a young woman. Digestion. 67:105–110. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wojcicki M, Haagsma EB, Gouw AS, Slooff MJ
and Porte RJ: Orthotopic liver transplantation for portosystemic
encephalopathy in an adult with congenital absence of the portal
vein. Liver Transpl. 10:1203–1207. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cheung KM, Lee CY, Wong CT and Chan AK:
Congenital absence of portal vein presenting as hepatopulmonary
syndrome. J Paediatr Child Health. 41:72–75. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tsuji K, Naoki K, Tachiyama Y, et al: A
case of congenital absence of the portal vein. Hepatol Res.
31:43–47. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Takagaki K, Kodaira M, Kuriyama S, et al:
Congenital absence of the portal vein complicating hepatic tumors.
Intern Med. 43:194–198. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kornprat P, Langner C, Fritz K and
Mischinger HJ: Congenital absence of the portal vein in an adult
woman: a case report. Wien Klin Wochenschr. 117:58–62. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ohnishi Y, Ueda M, Doi H, et al:
Successful liver transplantation for congenital absence of the
portal vein complicated by intrapulmonary shunt and brain abscess.
J Pediatr Surg. 40:E1–E3. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Takeichi T, Okajima H, Suda H, et al:
Living domino liver transplantation in an adult with congenital
absence of portal vein. Liver Transpl. 11:1285–1288. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Oei M and Wessling J: Abernethy
malformation - congenital aplasia of the portal vein a 29-year-old
patient. RoFo. 179:167–169. 2007.(in German). View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Collard B, Maleux G, Heye S, et al: Value
of carbon dioxide wedged venography and transvenous liver biopsy in
the definitive diagnosis of Abernethy malformation. Abdom Imaging.
31:315–319. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Maekawa S, Suzuki T, Mori K, et al:
Congenital absence of the portal vein in an adult woman with liver
tumor. Nihon Shokakibyo Gakkai Zasshi. 104:1504–1511. 2007.(in
Japanese). PubMed/NCBI
|
|
23
|
Kong Y, Zhang H, Liu C, et al: Abernethy
malformation with multiple aneurysms: incidentally found in an
adult woman with Caroli’s disease. Ann Hepatol. 12:327–331.
2013.PubMed/NCBI
|
|
24
|
Matsuura T, Soejima Y and Taguchi T:
Auxiliary partial orthotopic living donor liver transplantation
with a small-for-size graft for congenital absence of the portal
vein. Liver Transpl. 16:1437–1439. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chandler TM, Heran MK, Chang SD, Parvez A
and Harris AC: Multiple focal nodular hyperplasia lesions of the
liver associated with congenital absence of the portal vein. Magn
Reson Imaging. 29:881–886. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Barchetti F, Pellegrino L, Al-Ansari N, De
Marco V, Scarpato P and Ialongo P: absence of the portal vein in a
middle-aged man. Surg Radiol Anat. 33:369–372. 2011. View Article : Google Scholar
|
|
27
|
Caputo S and Manganiello CA: Severe
portopulmonary hypertension associated with an unusual pattern of
Abernethy malformation: three-dimensional computed tomography view.
Echocardiography. 29:E275–E277. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Scheuermann U, Foltys D and Otto G: Focal
nodular hyperplasia proceeds hepatocellular carcinoma in an adult
with congenital absence of the portal vein. Transpl Int.
25:E67–E68. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Badea R, Serban A, Procopet B, et al:
Education and imaging: hepatobiliary and pancreatic: Abernethy
malformation-congenital portocaval shunt. J Gastroenterol Hepatol.
27:18752012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tateishi Y, Furuya M, Kondo F, et al:
Hepatocyte nuclear factor-1 alpha inactivated hepatocellular
adenomas in patient with congenital absence of the portal vein: a
case report. Pathol Int. 63:358–363. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Alewine TC, Carter WR and Frew MJ:
Congenital absence of the portal vein in a patient with
urolithiasis. AJR Am J Roentgenol. 189:W150–W152. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Morgan G and Superina R: Congenital
absence of the portal vein: two cases and a proposed classification
system for portasystemic vascular anomalies. J Pediatr Surg.
29:1239–1241. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Morse SS, Taylor KJ, Strauss EB, Ramirez E
and Seashore JH: Congenital absence of the portal vein in
oculoauriculovertebral dysplasia (Goldenhar syndrome). Pediatr
Radiol. 16:437–439. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Marois D, van Heerden JA, Carpenter HA and
Sheedy PF 2nd: Congenital absence of the portal vein. Mayo Clin
Proc. 54:55–59. 1979.PubMed/NCBI
|
|
35
|
Yancy AG, Jeffries CP and Miller RM:
Congenital absence of the portal vein. J Natl Med Assoc.
53:119–121. 1961.PubMed/NCBI
|
|
36
|
Laverdiere JT, Laor T and Benacerraf B:
Congenital absence of the portal vein: case report and MR
demonstration. Pediatr Radiol. 25:52–53. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kamiya S, Taniguchi I, Yamamoto T, et al:
Analysis of intestinal flora of a patient with congenital absence
of the portal vein. FEMS Immunol Med Microbiol. 7:73–80. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Woodle ES, Thistlethwaite JR, Emond JC,
Whitington PF, Vogelbach P, Yousefzadeh DK and Broelsch CE:
Successful hepatic transplantation in congenital absence of
recipient portal vein. Surgery. 107:475–479. 1990.PubMed/NCBI
|
|
39
|
Nakasaki H, Tanaka Y, Ohta M, Kanemoto T,
Mitomi T, Iwata Y and Ozawa A: Congenital absence of the portal
vein. Ann Surg. 210:190–193. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Usuki N and Miyamoto T: A case of
congenital absence of the intrahepatic portal vein diagnosed by MR
angiography. J Comput Assist Tomogr. 22:728–729. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kim SZ, Marz PL, Laor T, Teitelbaum J,
Jonas MM and Levy HL: Elevated galactose in newborn screening due
to congenital absence of the portal vein. Eur J Pediatr.
157:608–609. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Guariso G, Fiorio S, Altavilla G, et al:
Congenital absence of the portal vein associated with focal nodular
hyperplasia of the liver and cystic dysplasia of the kidney. Eur J
Pediatr. 157:287–290. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Howard ER and Davenport M: Congenital
extrahepatic portocaval shunts - the Abernethy malformation. J
Pediatr Surg. 32:494–497. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Massin M, Verloes A and Jamblin P: Cardiac
anomalies associated with congenital absence of the portal vein.
Cardiol Young. 9:522–525. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Taoube KA, Alonso Calderon JL, Yandza T,
et al: Congenital absence of portal vein in a girl with biliary
atresia treated with liver transplant. Cir Pediatr. 12:38–40.
1999.(in Spanish). PubMed/NCBI
|
|
46
|
Wakamoto H, Manabe K, Kobayashi H and
Hayashi M: Subclinical portal-systemic encephalopathy in a child
with congenital absence of the portal vein. Brain Dev. 21:425–428.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kohda E, Saeki M, Nakano M, Masaki H,
Ogawa K, Nirasawa M and Hiramatsu K: Congenital absence of the
portal vein in a boy. Pediatr Radiol. 29:235–237. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Grazioli L, Alberti D, Olivetti L, et al:
Congenital absence of portal vein with nodular regenerative
hyperplasia of the liver. Eur Radiol. 10:820–825. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Andreani P, Srinivasan P, Ball CS, Heaton
ND and Rela M: Congenital absence of the portal vein in liver
transplantation for biliary atresia. Int J Surg Investig. 2:81–84.
2000.
|
|
50
|
Alvarez AE, Ribeiro AF, Hessel G, Baracat
J and Ribeiro JD: Abernethy malformation: one of the etiologies of
hepatopulmonary syndrome. Pediatr Pulmonol. 34:391–394. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Shinkai M, Ohhama Y, Nishi T, et al:
Congenital absence of the portal vein and role of liver
transplantation in children. J Pediatr Surg. 36:1026–1031. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kinjo T, Aoki H, Sunagawa H, Kinjo S and
Muto Y: Congenital absence of the portal vein associated with focal
nodular hyperplasia of the liver and congenital choledochal cyst: a
case report. J Pediatr Surg. 36:622–625. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Venkat-Raman N, Murphy KW, Ghaus K, Teoh
TG, Higham JM and Carvalho JS: Congenital absence of portal vein in
the fetus: a case report. Ultrasound Obstet Gynecol. 17:71–75.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Tanaka Y, Takayanagi M, Shiratori Y, et
al: Congenital absence of portal vein with multiple hyperplastic
nodular lesions in the liver. J Gastroenterol. 38:288–294. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Soejima Y, Taguchi T, Ogita K, et al:
Auxiliary partial orthotopic living donor liver transplantation for
a child with congenital absence of the portal vein. Liver Transpl.
12:845–849. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
56
|
Noe JA, Pittman HC and Burton EM:
Congenital absence of the portal vein in a child with Turner
syndrome. Pediatr Radiol. 36:566–568. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sumida W, Kaneko K, Ogura Y, et al: Living
donor liver transplantation for congenital absence of the portal
vein in a child with cardiac failure. J Pediatr Surg. 41:E9–E12.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Avila LF, Luis AL, Encinas JL, et al:
Congenital portosystemic shunt. The Abernethy malformation. Cir
Pediatr. 19:204–209. 2006.(in Spanish).
|
|
59
|
Koizumi J, Yamashita T, Dowaki S, et al:
Hepatobiliary and pancreatic: Hepatic adenoma, focal nodular
hyperplasia and congenital absence of the portal vein. J
Gastroenterol Hepatol. 21:6192006. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Schmidt S, Saint-Paul MC, Anty R, Bruneton
JN, Gugenheim J and Chevallier P: Multiple focal nodular
hyperplasia of the liver associated with congenital absence of the
portal vein. Gastroenterol Clin Biol. 30:310–313. 2006.(in French).
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Turkbey B, Karcaaltincaba M, Demir H,
Akcoren Z, Yuce A and Haliloglu M: Multiple hyperplastic nodules in
the liver with congenital absence of portal vein: MRI findings.
Pediatr Radiol. 36:445–448. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ringe K, Schirg E, Melter M, et al:
Congenital absence of the portal vein (CAPV). Two cases of
Abernethy malformation type 1 and review of the literature.
Radiologe. 48:493–502. 2008.(in German). View Article : Google Scholar
|
|
63
|
Kawano S, Hasegawa S, Urushihara N, et al:
Hepatoblastoma with congenital absence of the portal vein-a case
report. Eur J Pediatr Surg. 17:292–294. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Gocmen R, Akhan O and Talim B: Congenital
absence of the portal vein associated with congenital hepatic
fibrosis. Pediatr Radiol. 37:920–924. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ratnasamy C, Kurbegov A and Swaminathan S:
Cardiac anomalies in the setting of the Abernethy malformation of
the portal vein. Cardiol Young. 17:212–214. 2007. View Article : Google Scholar
|
|
66
|
Goo HW: Extrahepatic portosystemic shunt
in congenital absence of the portal vein depicted by time-resolved
contrast-enhanced MR angiography. Pediatr Radiol. 37:706–709. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Morotti RA, Killackey M, Shneider BL,
Repucci A, Emre S and Thung SN: Hepatocellular carcinoma and
congenital absence of the portal vein in a child receiving growth
hormone therapy for turner syndrome. Semin Liver Dis. 27:427–431.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Emre S, Arnon R, Cohen E, Morotti RA,
Vaysman D and Shneider BL: Resolution of hepatopulmonary syndrome
after auxiliary partial orthotopic liver transplantation in
Abernethy malformation. A case report. Liver Transpl. 13:1662–1668.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Morikawa N, Honna T, Kuroda T, et al:
Resolution of hepatopulmonary syndrome after ligation of a
portosystemic shunt in a pediatric patient with an Abernethy
malformation. J Pediatr Surg. 43:E35–E38. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Tsutsui M, Sugahara S, Motosuneya T, Wada
H, Fukuda I, Umeda E and Kazama T: Anesthetic management of a child
with Costello syndrome complicated by congenital absence of the
portal vein - a case report. Paediatr Anaesth. 19:714–715. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Peker A, Ucar T, Kuloglu Z, et al:
Congenital absence of portal vein associated with nodular
regenerative hyperplasia of the liver and pulmonary hypertension.
Clin Imaging. 33:322–325. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Kasahara M, Nakagawa A, Sakamoto S, et al:
Living donor liver transplantation for congenital absence of the
portal vein with situs inversus. Liver Transpl. 15:1641–1643. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Sanada Y, Mizuta K, Kawano Y, et al:
Living donor liver transplantation for congenital absence of the
portal vein. Transplant Proc. 41:4214–4219. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Hino T, Hayashida A, Okahashi N, et al:
Portopulmonary hypertension associated with congenital absence of
the portal vein treated with bosentan. Intern Med. 48:597–600.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Raghuram KA, Bijulal S, Krishnamoorthy KM
and Tharakan JA: Regression of pulmonary vascular disease after
therapy of Abernethy malformation in visceral heterotaxy. Pediatr
Cardiol. 4:1882–1885. 2013. View Article : Google Scholar
|
|
76
|
Loomba RS, Telega GW and Gudausky TM: Type
2 Abernethy malformation presenting as a portal vein-coronary sinus
fistula. J Pediatr Surg. 47:E25–E31. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Passalacqua M, Lie KT and Yarmohammadi H:
Congenital extrahepatic portosystemic shunt (Abernethy
malformation) treated endovascularly with vascular plug shunt
closure. Pediatr Surg Int. 28:79–83. 2012. View Article : Google Scholar
|
|
78
|
Pathak A, Agarwal N, Mandliya J, Gehlot P
and Dhaneria M: Abernethy malformation: a case report. BMC Pediatr.
12:572012. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Gadodia A, Sharma R, Kandpal H and Prashad
R: Congenital absence of portal vein with large inferior
mesenteric-caval shunt. Trop Gastroenterol. 32:223–226. 2011.
|
|
80
|
Asran MK, Loyer EM, Kaur H and Choi H:
Case 177: Congenital absence of the portal vein with hepatic
adenomatosis. Radiology. 262:364–367. 2012. View Article : Google Scholar
|
|
81
|
Chandrashekhara SH, Bhalla AS, Gupta AK,
Vikash CS and Kabra SK: Abernethy malformation with portal vein
aneurysm in a child. J Indian Assoc Pediatr Surg. 16:21–23. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Osorio MJ, Bonow A, Bond GJ, Rivera MR,
Vaughan KG, Shah A and Shneider BL: Abernethy malformation
complicated by hepatopulmonary syndrome and a liver mass
successfully treated by liver transplantation. Pediatr Transplant.
15:E149–E151. 2011. View Article : Google Scholar
|
|
83
|
Tannuri U, Galvão F, Leal AJ, Gibelli NE
and Tannuri AC: Congenital absence of the portal vein: a complex
disease with multiple manifestations and types of treatment. Eur J
Pediatr Surg. 21:269–272. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Law YM, Mack CL, Sokol RJ, Rice M, Parsley
L and Ivy D: Cardiopulmonary manifestations of portovenous shunts
from congenital absence of the portal vein: pulmonary hypertension
and pulmonary vascular dilatation. Pediatr Transplant.
15:E162–E168. 2011. View Article : Google Scholar :
|
|
85
|
Uchida H, Sakamoto S, Shigeta T, et al:
Living donor liver transplantation with renoportal anastomosis for
a patient with congenital absence of the portal vein. Case Rep
Surg. 2012:670289g2012.
|
|
86
|
Ogul H, Bayraktutan U, Yalcin A, Turan MI,
Ozgokce M, Eren S and Kantarci M: Congenital absence of the portal
vein in a patient with multiple vascular anomalies. Surg Radiol
Anat. 35:529–534. 2013. View Article : Google Scholar
|
|
87
|
Banz V, Olliff S, Taniere P, Mayer D and
Isaac J: Liver tumours in patients with Abernethy malformation. ANZ
J Surg. 81:640–641. 2011. View Article : Google Scholar
|
|
88
|
Shinkai M, Ohhama Y, Nishi T, et al:
Living related partial liver transplantation for hyperammonemia due
to congenital absence of the portal vein. Transplant Proc.
32:21842000. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Joyce AD and Howard ER: Rare congenital
anomaly of the portal vein. Br J Surg. 75:1038–1039. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Bellah RD, Hayek J and Teele RL: Anomalous
portal venous connection to the suprahepatic vena cava: sonographic
demonstration. Pediatr Radiol. 20:115–117. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Marks C: Developmental basis of the portal
venous system. Am J Surg. 117:671–681. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Moretti G, Staeffen J, Broustet A and Le
Bras M: Congenital malformations associated with stenosis of the
portal vein. Sem Hop. 44:893–897. 1968.(in French). PubMed/NCBI
|
|
93
|
K C S, Matsutani S, Maruyama H, et al:
Portal-systemic encephalopathy in two patients without liver
cirrhosis and portal hypertension. Hepatol Res. 23:122–129. 2002.
View Article : Google Scholar
|