Introduction
Primary cancer of the trachea is particularly rare
(1) and accounts for only 0.1–0.4%
of all newly diagnosed respiratory tract cancers, which corresponds
to 2.6 new cases per 1,000,000 individuals, annually, worldwide
(2,3). Approximately 75% of these tumors are
squamous cell carcinoma or adenoid cystic carcinoma (4). Malignant melanomas occur primarily as
skin lesions and account for 2% of all skin tumors, worldwide
(5). Although primary malignant
melanoma frequently metastasize to the liver, lung, brain, or bone,
this type of cancer rarely occurs in parts of the body other than
the skin. The most uncommon form of extracutaneous melanoma is
primary tracheal melanoma (6–10). In
the present study, the case of a patient presenting with malignant
melanoma of the trachea is reported to improve the current
understanding of this rare disease. Written informed consent was
obtained from the patient.
Case report
In March 2013, a 68-year-old male presented to the
Department of Respiratory Medicine, Shizuoka City Hospital
(Shizuoka, Japan) with a cough and bloody sputum, which had
worsened over the previous two month and become intractable, with
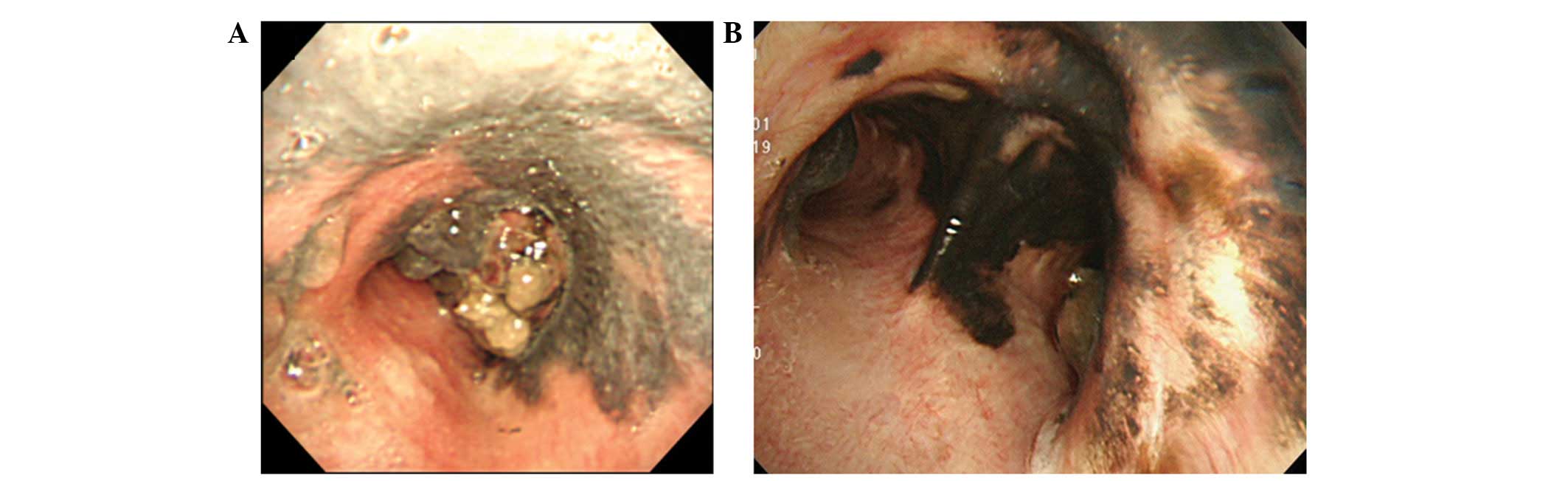
the development of stridor. A chest computed tomography (CT) scan
revealed a 25×20×15-mm intratracheal lesion located immediately
above the carina (Fig. 1), which
reduced the cross-sectional area of the trachea by ~90%. Flexible
bronchoscopy demonstrated these results and revealed an obstructive
tumor surrounding the carina, as well as irregularly shaped,
darkened regions in the tracheal mucosa (Fig. 2A).
Following biopsy of the tumor and the surrounding
mucosa, the tumor was cauterized with argon plasma coagulation
(APC) to restore airway patency, however, the presence of a
residual tumor mass was not clear. Following cauterization, the
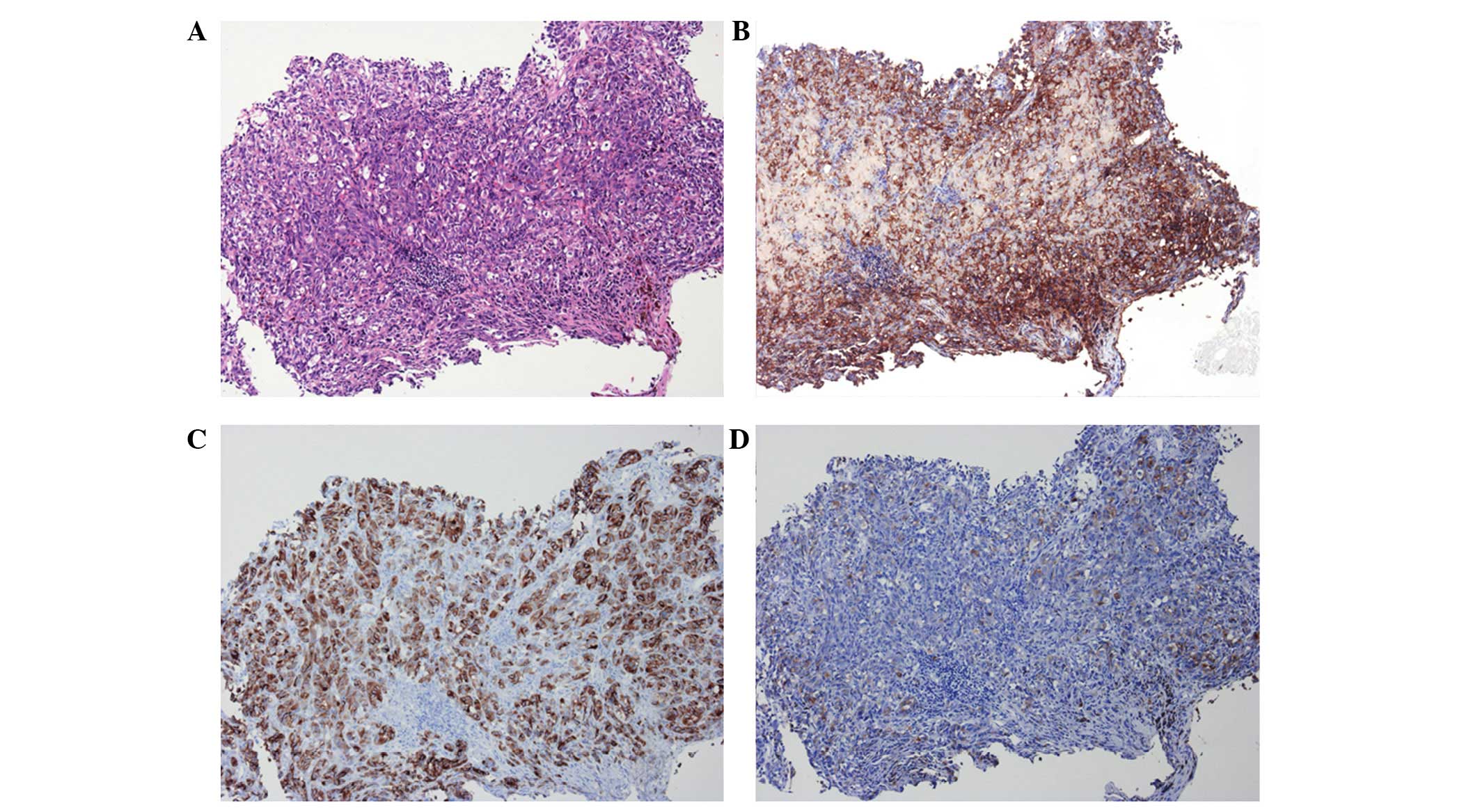
patient experienced immediate symptomatic relief. The biopsy
specimens were composed of tumor fragments and aggregated
melanophages. Histologically, hematoxylin and eosin staining of the
tumor demonstrated proliferation of epithelioid-shaped atypical
cells with marginal melanin production (Fig. 3A). In addition, the tumor cells
showed positive immunostaining for three melanoma markers, S-100,
melan-A and HMB-45 (Fig. 3B–D).
Subsequently, the tumor was diagnosed as a malignant melanoma. The
biopsy specimens from the bronchial mucosa revealed a band-like
accumulation of melanophages and lymphocytes beneath the tracheal
epithelium. However, melanoma infiltration was not observed among
the melanophages.
The patient did not have a history of previous
surgeries or skin biopsies and did not exhibit melanoma-like skin
lesions. In addition, magnetic resonance imaging and positron
emission tomography did not reveal any metastatic lesions in the
brain. The level of 5-S-cysteinyldopa, a biochemical marker of
melanoma, which was 7.6 nmol/l (normal range, 1.5–8.0 nmol/l) at
diagnosis, did not increase. As a result of these findings, it was
hypothesized that the trachea was the primary site of the tumor and
no metastasis had occurred at the time of clinical
presentation.
The lesion was inoperable due to its large size;
therefore, the patient was treated with a combination of
dacarbazine-based chemotherapy (200 mg/m2 dacarbazine,
days 1–5) for three cycles every 4 weeks, for three months and
thoracic radiotherapy (total dose, 65 Gy in 30 fractions).
Following chemoradiotherapy, bronchoscopy revealed darkened regions
of the tracheal mucosa (Fig. 2B).
Subsequently, metastatic lesions appeared in the lungs and the
5-S-cysteinyldopa levels gradually increased, thus, chemotherapy
was resumed.
Discussion
Primary tracheal malignant melanoma is particularly
rare (6–10) and there are only a small number of
reports regarding intratracheal metastasis (11). Various studies have investigated the
oncogenesis of mucosal melanomas and have attempted to elucidate
the histogenesis of lower respiratory tract melanomas (12,13).
Theories include melanocytic migration during embryogenesis,
transformation of respiratory epithelial cells into melanocytes and
differentiation of neuroendocrine cells to melanocyte (12).
Pathological examination cannot distinguish primary
melanoma from metastatic melanoma. The criteria for primary
respiratory malignant melanoma diagnosis are as follows: A solitary
lesion; ‘dropping off’ of melanoma cells together with junctional
changes in the mucosa; invasion from the epithelium toward the
submucosa; histologically identified presence of melanin; no prior
skin lesions; and no familial history of cutaneous disease
(12). In the present case, no
other primary lesions were identified on radiological or
dermatological examination. The patient was diagnosed with a
primary tracheal malignant melanoma on the basis of three criteria:
The lack of a history of skin lesions and a family history of
cancer; the presence of a solitary tumor surrounded by abnormal
mucosa; and positive immunostaining for three melanoma markers,
S-100, melan-A and HMB-45. These results are consistent with the
diagnostic criteria for primary malignant melanoma in the
respiratory tract (13,14).
Tracheal tumors may be fatal as they occasionally
obstruct the airway. However, due to their rarity, no standard
treatment has been identified. Treatment is either palliative,
which aims to restore airway patency, or therapeutic, with tracheal
resection and end-to-end anastomosis (15). In the current case, APC was
conducted to restore airway patency. This indicated that treating
tracheal tumors with APC may be an effective type of palliative
therapy to provide immediate relief, as well as long-term
improvements in patient quality of life. Although it is useful to
combine palliative measures with therapeutic agents, including
radiation and biological or chemical agents, the current treatment
strategies are inadequate. For example, radiotherapy may be an
effective method to locally control tracheal melanoma, however, it
does not improve long-term survival (16).
In conclusion, the patient in the current case was
treated with radiation and dacarbazine-based chemotherapy, which is
a standard chemotherapeutic agent for malignant melanoma.
Initially, the radiotherapy facilitated with controlling the local
spread of the tumor, however, follow-up CT scans revealed distant
metastasis to the lungs. In future, targeted cancer therapies using
molecules, such as BRAF inhibitors, and cytotoxic
T-lymphocyte-associated protein, programmed cell death protein 1
and programmed death-ligand 1 antibodies (17–20),
may be effective options for treating cases of advanced malignant
melanoma, including those originating in the trachea.
Acknowledgements
The authors would like to thank Ms. Mutsumi
Yamazaki, Mr. Taiki Miyauchi, Dr Kazushige Wakuda, Dr Takuya
Oyakawa, Dr Yasushi Hisamatsu and Dr Hiroaki Akamatsu for their
assistance in preparing this case report.
References
|
1
|
Urdaneta AI, Yu JB and Wilson LD:
Population based cancer registry analysis of primary tracheal
carcinoma. Am J Clin Oncol. 34:32–37. 2011. View Article : Google Scholar
|
|
2
|
Rostom AY and Morgan RL: Results of
treating primary tumours of the trachea by irradiation. Thorax.
33:387–393. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Maziak DE, Todd TR, Keshavjee SH, Winton
TL, Van Nostrand P and Pearson FG: Adenoid cystic carcinoma of the
airway: thirty-two-year experience. J Thorac Cardiovasc Surg.
112:1522–1532. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li W, Ellerbroek NA and Libshitz HI:
Primary malignant tumors of the trachea. A radiologic and clinical
study. Cancer. 66:894–899. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lens MB and Dawes M: Global perspectives
of contemporary epidemiological trends of cutaneous malignant
melanoma. Br J Dermatol. 150:179–185. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Duarte IG, Gal AA and Mansour KA: Primary
malignant melanoma of the trachea. Ann Thorac Surg. 65:559–560.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Terra RM, Minamoto H, Junqueira JJ,
Falzoni R, Pego-Fernandes PM and Jatene FB: Tracheal malignant
melanoma: successful outcome with tracheal resection. Ann Thorac
Surg. 86:308–310. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nattout M, Fuleihan N, Sabra O, Aburizk I
and Hamdan AL: Primary malignant melanoma of the trachea. Middle
East J Anesthesiol. 20:607–609. 2010.PubMed/NCBI
|
|
9
|
Cekin E, Cincik H, Yilmaz I and Gungor A:
Primary malignant melanoma of the trachea: case report. Ear Nose
Throat J. 89:E18–E20. 2010.PubMed/NCBI
|
|
10
|
Nureki S, Miyazaki E, Fujisaki H, Ito T,
Kumamoto T, Tokuishi K and Kawahara K: Incidentally discovered
primary malignant melanoma of the trachea. Intern Med.
51:1743–1746. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Koh HK: Cutaneous melanoma. N Engl J Med.
325:171–182. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jennings TA, Axiotis CA, Kress Y and
Carter D: Primary malignant melanoma of the lower respiratory
tract. Report of a case and literature review. Am J Clin Pathol.
94:649–655. 1990.PubMed/NCBI
|
|
13
|
Colby TV, Koss MN and Travis WD: Tumors of
the lower respiratory tract. Atlas of Tumor Pathology. Rosai J and
Sobin LH: 3rd edition. Armed Forces Institute of Pathology, . Armed
Forces Institute of Pathology; Washington DC: pp. 483–487. 1995
|
|
14
|
Jensen OA and Egedorf J: Primary malignant
melanoma of the lung. Scand J Respir Dis. 48:127–135.
1967.PubMed/NCBI
|
|
15
|
Capaccio P, Peri A, Fociani P, Ferri A and
Ottaviani F: Flexible argon plasma coagulation treatment of
obstructive tracheal metastatic melanoma. Am J Otolaryngol.
23:253–255. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lentsch EJ and Myers JN: Melanoma of the
head and neck: current concepts in diagnosis and management.
Laryngoscope. 111:1209–1222. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ascierto PA, Minor D, Ribas A, Lebbe C,
O’Hagan A, Arya N, et al: Phase II trial (BREAK-2) of the BRAF
inhibitor dabrafenib (GSK2118436) in patients with metastatic
melanoma. J Clin Oncol. 31:3205–3211. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hamid O, Robert C, Daud A, Hodi FS, Hwu
WJ, Kefford R, et al: Safety and tumor responses with lambrolizumab
(anti-PD-1) in melanoma. N Engl J Med. 369:134–144. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ott PA, Hodi FS and Robert C: CTLA-4 and
PD-1/PD-L1 blockade: new immunotherapeutic modalities with durable
clinical benefit in melanoma patients. Clin Cancer Res.
19:5300–5309. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wolchok JD, Kluger H, Callahan MK, Postow
MA, Rizvi NA, Lesokhin AM, et al: Nivolumab plus ipilimumab in
advanced melanoma. N Engl J Med. 369:122–133. 2013. View Article : Google Scholar : PubMed/NCBI
|