Introduction
The occurrence of multiple primary malignant
neoplasms (MPMNs) is increasing, with the reported incidence
ranging between 0.734 and 11.3% in India (1). In patients with neoplastic disease, an
early diagnosis and treatment with chemo- and radiotherapy improves
long-term survival, thus increasing the risk of developing
subsequent primary tumours (2).
Furthermore, with improvements in diagnostic modalities, including
positron emission tomography (PET), indolent tumour detection rates
have increased, contributing to the apparent increase in the
incidence of multiple primary malignancies (3).
Studies on the survival of patients with MPMNs are
limited, possibly due to the particularly heterogeneous nature of
this group (4). It has been
suggested that the presence of multiple cancers does not affect the
overall survival rate of patients with MPMNs (5), and that the overall survival rate is
similar to that of patients with single lesion tumour types
(6). However, according to the
literature, patients with three asynchronous primary malignant
neoplasms exhibit an extremely poor prognosis (7,8).
In the current study, a patient presented with three
rare distinct primary malignant neoplasms, consisting of
epithelioid hemangioendothelioma (EHE) of the brain, Ewing’s
sarcoma of the lumbar vertebrae and malignant solitary fibrous
tumour (SFT) of the liver. The primary Ewing’s sarcoma affected the
lumbar 2 (L2) vertebra, as did metastases of the EHE and malignant
SFT. The patient received multidisciplinary treatment and survived
for >14 years. Written informed consent was obtained from the
patient’s family.
Case report
A 31-year-old female presented with severe headache
upon wakening for 6 months and was referred to The First Affiliated
Hospital of Sun Yat-sen University (Guangzhou, China) in May 1999.
No other symptoms were noted during a physical examination. Head
computed tomography (CT) scans revealed a slightly hyperintense
mass in the left parietal region. Radionuclide bone scanning, chest
radiography and abdominal ultrasonography revealed no evidence of
malignant lesions in other organs. The patient underwent surgical
excision of the left parietal lesion. Histopathological analysis of
the resected tumour revealed an EHE with a cluster of
differentiation (CD)34-positive and factor VIII-associated
antigen-positive immunophenotype. A post-operative follow-up, which
lasted for five years, revealed no evidence of recurrence.
In November 2004, the patient reported lower back
and left leg pain. A magnetic resonance imaging (MRI) scan revealed
a compression fracture and slightly hyperintense mass in the L2
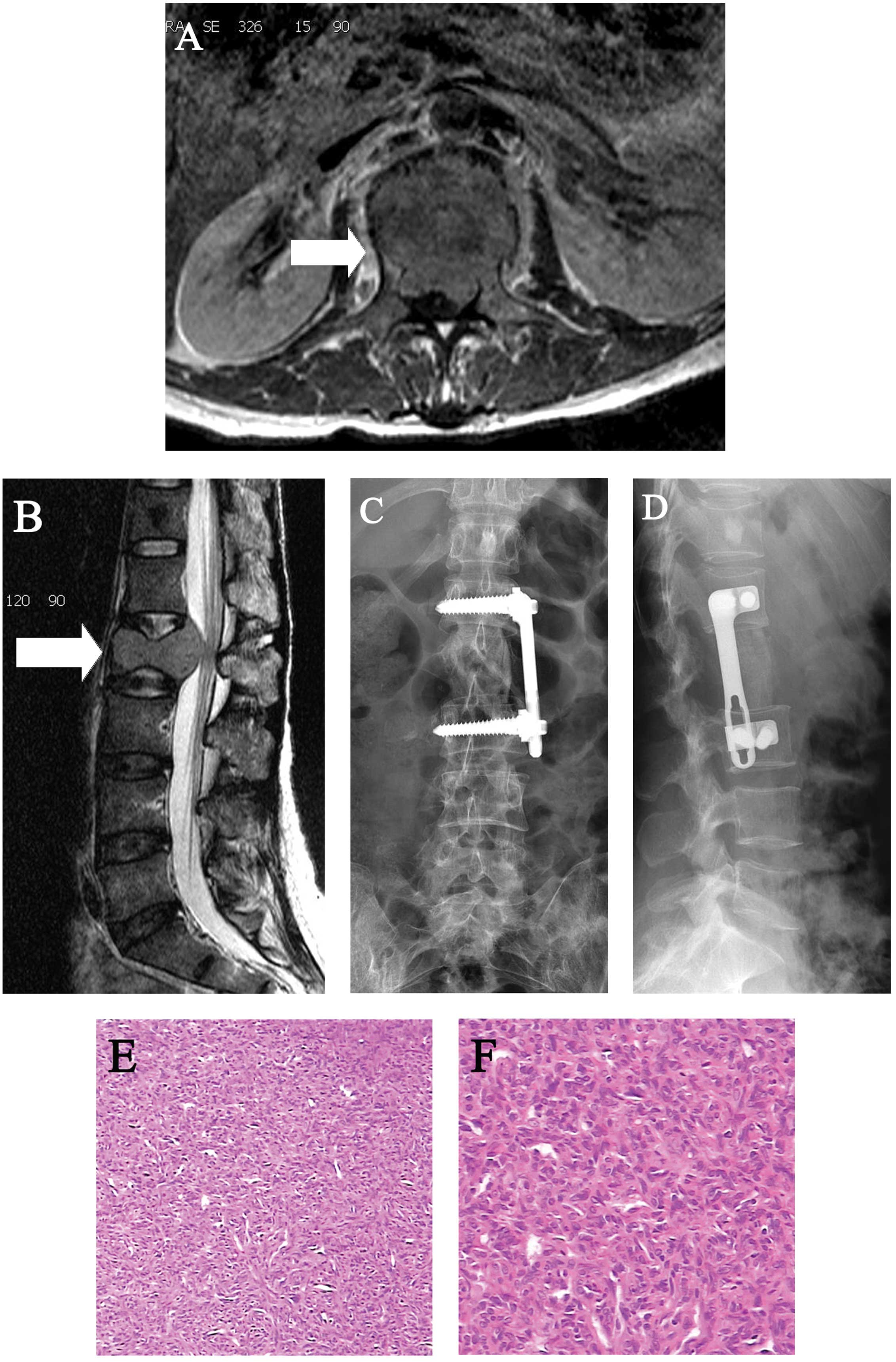
vertebra, as well as compression of the spinal cord (Fig. 1A and B). Following the exclusion of
other organ involvement by radionuclide bone scanning, chest
radiography and abdominal ultrasonography, an anterior L2
vertebrectomy and L1–L3 fusion were performed (Fig. 1C and D). The post-operative
histopathological examination indicated that the lesion was
metastatic EHE (Fig. 1E and F). The
patient was administered with radiotherapy at a dose of 44 Gy for
22 cycles. The patient did not experience any adverse reactions in
response to the radiotherapy.
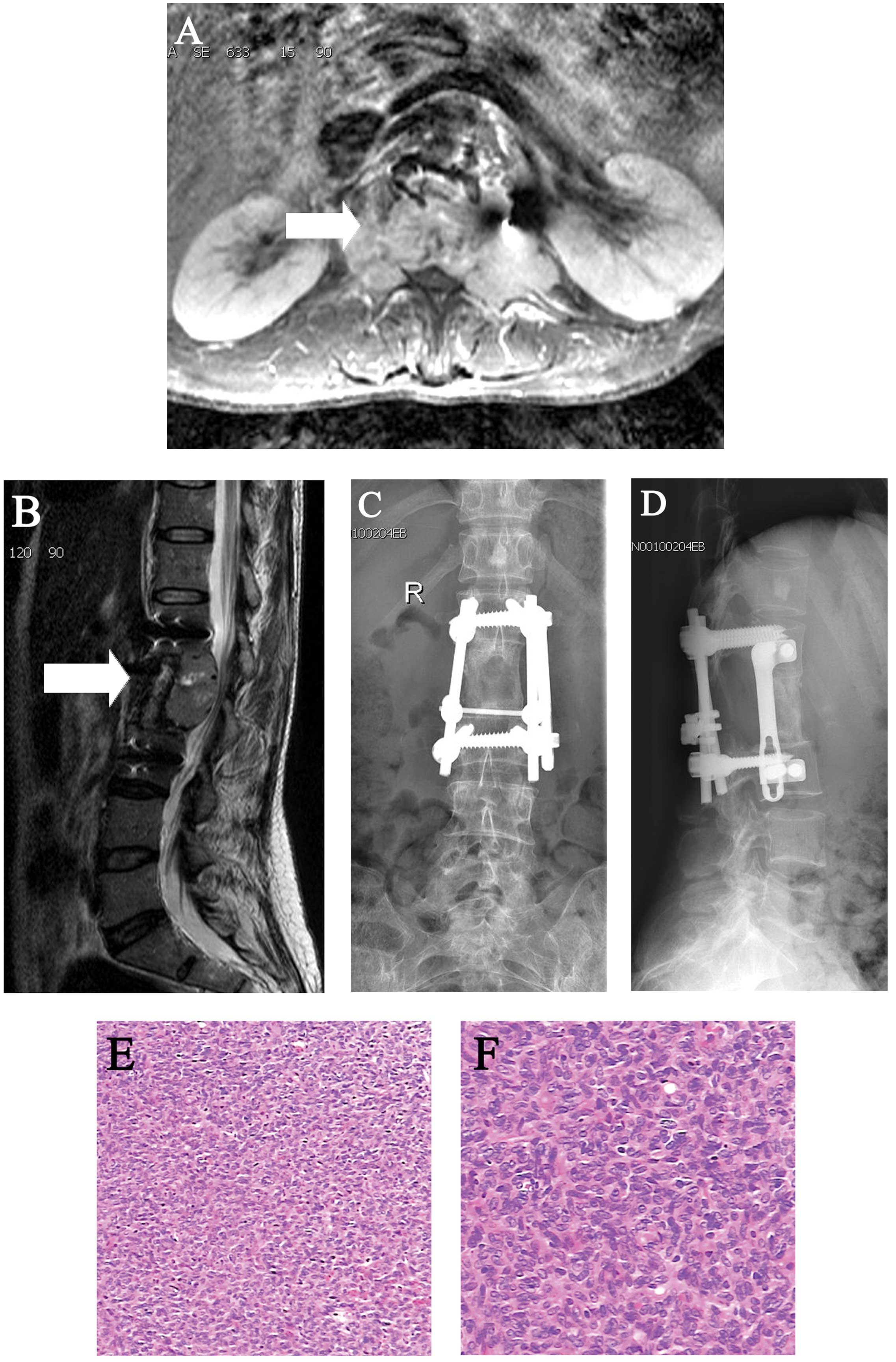
In April 2007, the patient presented with recurrent
lower back and left leg pain. An MRI scan revealed a posterior
enhancing mass and spinal cord compression at the L2 vertebra
level, with involvement of the bilateral vertebral lamina and
superior processes (Fig. 2A and B).
The involvement of other organs was excluded. Following a
pre-operative diagnosis of recurrent EHE, a posterior lesion
excision was performed with pedicle screw fixation (Fig. 2C and D). However, the subsequent
histopathological examination indicated primary lumbar Ewing’s
sarcoma with a vimentin-positive and microneme protein 2
(MIC2)-positive immunophenotype (Fig.
2E and F), for which the patient received 22 cycles of
radiotherapy at a dose of 40 Gy and six cycles of chemotherapy,
consisting of 2 mg vincristine, 0.7 mg dactinomycin, 700 mg
cyclophosphamide and 40 mg adriamycin, over an 18-week period. The
patient experienced mild gastrointestinal symptoms and impaired
liver function during the treatment phase.
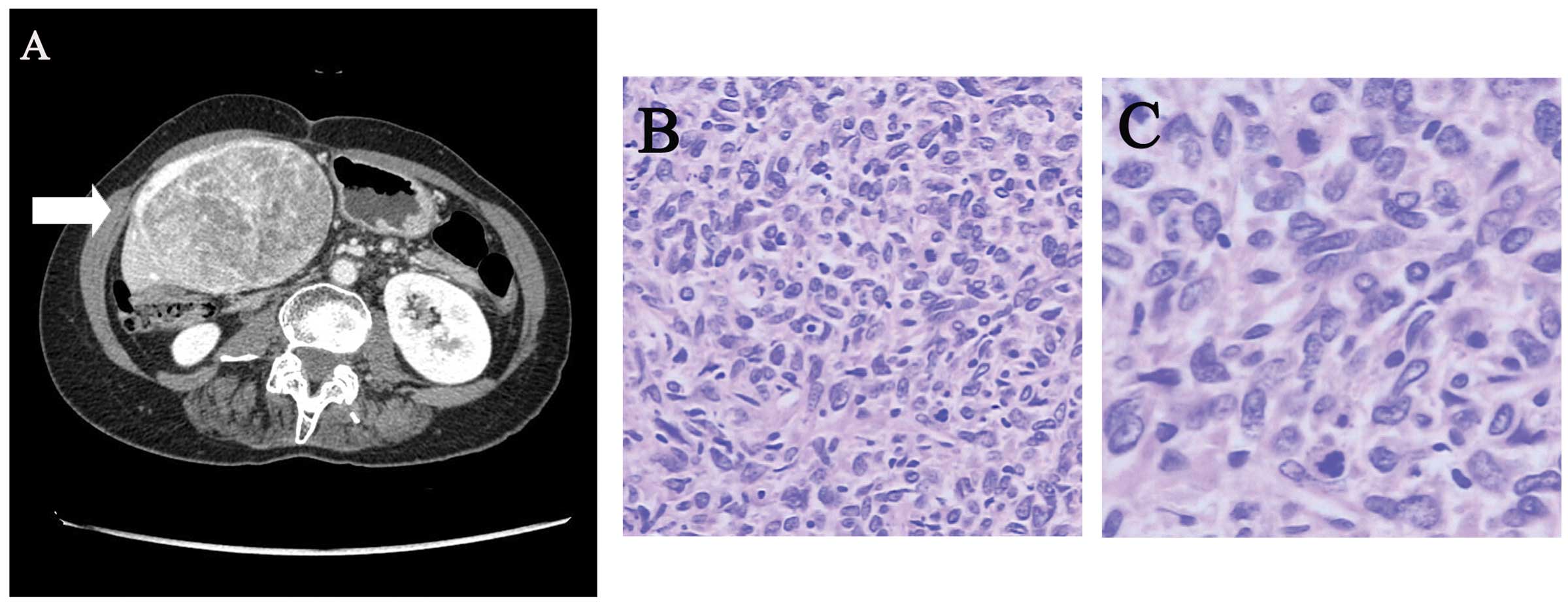
In May 2009, the patient presented with an abdominal
mass. An abdominal CT scan revealed a hyperintense mass in the S5
hepatic segment, with a maximum diameter of 10 cm (Fig. 3A). The involvement of other organs
was excluded. Hepatic segmentectomy was conducted to remove the S5
hepatic segment and the tumour. The histopathological report
indicated a primary malignant SFT (Fig.
3B and C) with a CD34-positive and B-cell lymphoma
(Bcl)-2-positive immunophenotype.
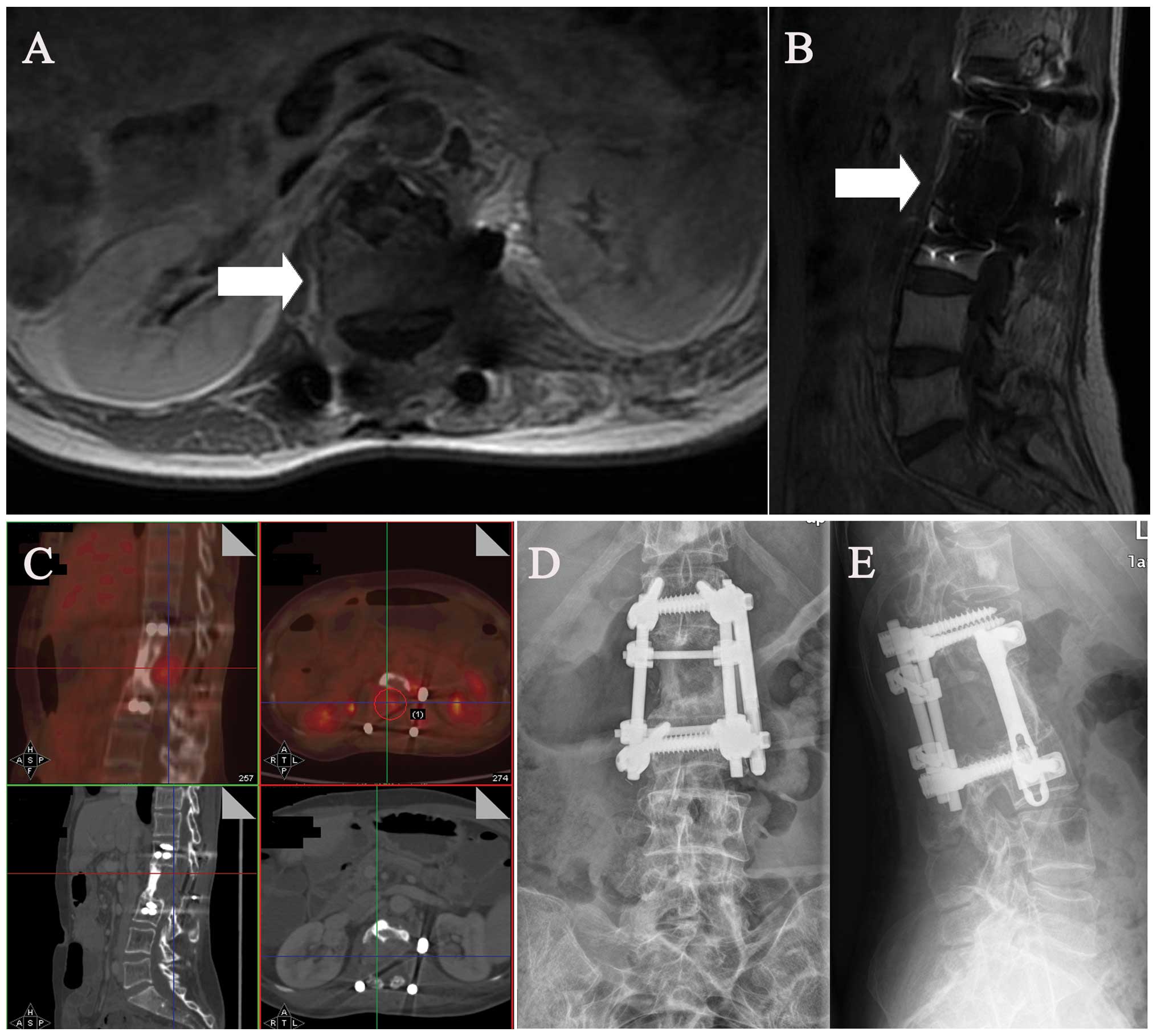
In March 2010, the patient presented again with
recurrent lower back and left leg pain. MRI and PET-CT scans
revealed a posterior enhancing mass and spinal cord compression at
the L2 vertebral level (Fig. 4A–C).
Recurrent lumbar Ewing’s sarcoma was diagnosed and, subsequent to
discussion with the patient, a palliative resection of the lumbar
mass was performed to decompress the spinal cord (Fig. 4D and E). The post-operative
histopathological examination indicated that the lesion was
metastatic malignant SFT and palliative chemoradiotherapy was
therefore initiated.
In April 2013, the patient experienced fever,
dyspnoea and bone pain throughout the body. Radionuclide bone
scanning and chest radiography revealed multiple bone metastases
and a pulmonary infection. Laboratory examinations revealed
pancytopenia. The patient was treated with palliative care and
symptomatic therapy, but succumbed to respiratory-circulatory
failure in June 2013.
Discussion
Multiple primary neoplasms in a single patient were
first reported at the end of the 19th century (9). The criteria for the definition of
multiple primary neoplasms was provided by Warren and Gates in 1932
(10), who specified that each
tumour must be distinct and present a definitive pattern of
malignant disease, and that the possibility of metastasis from a
primary tumour must be excluded. Tumours were defined as
synchronous if occurring within six months of the diagnosis of the
cancer and asynchronous if occurring more than six months prior to
or following the diagnosis. In the present case, the patient was
diagnosed with three rare distinct primary tumours, thus meeting
the criteria for a diagnosis of triple asynchronous PMNs. MPMNs
with three distinct lesions are considered extremely rare (11). MPMNs most commonly occur in the
respiratory, gastrointestinal and genitourinary systems (10), and the involvement of brain, bone
and liver tissues has rarely been reported (4). In addition, the incidence of EHE of
the brain, Ewing’s sarcoma of the lumbar vertebra and malignant SFT
of the liver, respectively, is extremely low, making the current
case unique. EHE is an extremely rare intracranial tumour (12) that frequently affects the soft
tissues, lung, liver and bone. The clinical manifestations of EHE
depend on the location of occurrence, and the majority of patients
present with a mass and symptoms of intracranial hypertension.
Intracranial EHE lesions appear as isointense, hyperintense or
heterogeneous masses on pre-operative MRI T1- and T2-weighted
images (13), and vascular flow
voids are observed on T2-weighted images (14). EHE tumours are detected by positive
immunostaining for endothelial cell markers, including CD31, CD34
and factor VIII-associated antigen (15). In the present study, CD34 and factor
VIII-associated antigen immunopositive tumour cells were detected,
indicating the presence of EHE.
Ewing’s sarcoma of the bone most frequently involves
the pelvic bones and femur (16),
and although the vertebral column is frequently involved in
metastatic disease (17), primary
vertebral Ewing’s sarcoma is rare, with a reported incidence of
3.5–15% of all cases (18,19). The clinical manifestations of
Ewing’s sarcoma that arise primarily in the spinal epidural space
include back pain with or without radicular pain, paresis in one or
two legs, sensory disturbances, and bladder and bowel dysfunction
(20). The severe lower back pain
and radicular leg pain experienced by the present patient were
indicative of Ewing’s sarcoma. On MRI scans, Ewing’s sarcoma
exhibits a low to isointense signal on T1-weighted images, high
signal intensity on T2-weighted images and heterogeneous
enhancement (21). Characteristic
histological features of Ewing’s sarcoma include narrow sheets of
poorly-differentiated cells exhibiting uniform round or oval nuclei
and scant cytoplasm (22).
Immunohistochemical analysis of Ewing’s sarcoma typically reveals
the expression of vimentin and MIC2, as was observed in the present
case.
Hepatic SFT is rare (23) and exhibits non-specific clinical
manifestations. It can be asymptomatic and demonstrate increased
abdominal volume, as was observed in the current case, or can
present with symptoms that include nausea, vomiting, abdominal pain
and hypoglycaemia (24,25). The majority of hepatic SFTs are
benign and few studies reporting local recurrence or metastases
exist (26). The current case is
remarkable as lumbar metastases were apparent. The imaging features
of SFT are also non-specific and cannot be used to distinguish
between benign and malignant tumours. The lesion is usually a
single large, well-circumscribed, heterogeneously enhancing mass on
CT and MRI images (24). SFT cells
are positive for CD34 in 90–95% of tumours, MIC2 in 70% of tumours
and Bcl-2 in >80% of tumors (27). In the present case, the tumour cells
were strongly positive for CD34 and Bcl-2, but were negative for
CD117, smooth muscle antigen, S-100, EMA and desmin expression,
indicating that the tumour was an SFT.
In the present study, the interval between the
occurrences of the first two primary neoplasms was eight years, and
the subsequent intervals were two years. Similar to other reported
cases, the mean interval between the diagnoses of the first two
primary tumours is always greater than the interval between the
detections of subsequent neoplasms, the cause of which has yet to
be elucidated (28). There are
numerous possible reasons for the development of MPMNs, including
prior chemo- or radiotherapy, lifestyle choices, such as tobacco,
alcohol and diet, environmental exposures, host determinants, such
as genetic predisposition or immune dysfunction, and combination
effects, such as gene-environment and gene-gene interactions
(29). Treatment-associated
exposure to high doses of radiation or alkylating agents has been
implicated in the development of subsequent malignancies (30). In the current case, the second and
the third primary malignant neoplasms developed following
chemoradiotherapy, which may have contributed to the development of
MPMNs to a certain extent. A notable phenomenon was that the L2
vertebra was the sole vertebral site for the primary Ewing’s
sarcoma, the metastatic EHE and the malignant SFT. Among patients
with cancer, 12–20% present initially with spinal column
metastases, 30% of which occurs in the lumbosacral region, but
rarely in a single vertebra, indicating that the initial
radiotherapy in this region may have been the cause of subsequent
malignancies. In addition, the risk of multiple malignancies
appears to be impacted by age at the time of diagnosis of the first
tumour (31). A review of the
literature determined that patients with MPMNs tend to be older
than those with a single primary malignant neoplasm, with >75%
of patients with MPMNs being >50 years old (32). However, the present patient was 45
years old at the time of writing the current study.
Treatment strategies for patients with MPMNs differ
from the strategies used for patients with metastatic or recurrent
cancer. Therefore, a novel tumour in a patient with cancer should
be considered not only as recurrence or metastasis but also as a
different primary malignancy. For asynchronous primary malignant
neoplasms, it has been recommended for each tumour to be evaluated
and staged as an independent tumour and treated aggressively with
curative intent to achieve the maximum therapeutic benefit
(1). If surgery is indicated for
the two tumours, the procedure can be performed in a single-stage
setting in the majority of cases, with low rates of morbidity and
mortality (33). In the current
case, the three primary malignant neoplasms were treated
differently according to the individual tumour characteristics.
Surgical removal is the recommended treatment for
EHE (34), and pre- and
post-operative adjuvant therapies, consisting of chemo- or
radiotherapy, are recommended for cases in which total resection is
not possible, and those involving metastasis or multiple tumours
(13,34). The initial excision of the
intracranial EHE in the current case proved successful, with no
complications or symptoms until the metastasis of EHE in the L2
vertebra five years later, which required chemoradiotherapy.
Current protocols for the treatment of Ewing’s
sarcoma include radical excision, which generally exhibits a good
prognosis (35), followed by
radiotherapy and multidrug chemotherapy. In the current case, the
Ewing’s sarcoma was pre-operatively diagnosed as recurrent EHE.
Therefore, the patient underwent radical excision and
chemoradiotherapy, with no evidence of recurrence being found
during the follow-up.
The recommended treatment for hepatic SFT is radical
removal of the tumour with clear margins of resection, with
post-operative adjuvant therapy reserved for cases of incomplete
resection or cases exhibiting histopathological features of
malignancy (36). In the current
case, radical resection was performed on the primary hepatic SFT
without subsequent chemoradiotherapy in 2009. However, one year
later, the lumbar metastasis of SFT was indentified and adjuvant
chemoradiotherapy was initiated following surgical resection of the
metastatic lesion.
Depending upon the site, pathological pattern,
tumour variant, type of treatment and clinical series, the
five-year survival rate of patients with MPMN can range between 33
and 65% (37,38). Gursel et al reported the mean
overall survival of patients with MPMN to be 97.2±15.0 months
(3). The longest overall survival
of a patient with MPMN documented to date is 288 months (39). The patient in the present case
survived for >14 years and the increased survival time may be
associated with the multidisciplinary treatment the patient
received.
The findings of the present study have the following
clinical implications. Firstly, if pre-operative biopsy is not
performed, a correct diagnosis may not be obtained, thus delaying
treatment for MPMNs. A more standardized diagnosis procedure,
including pre-operative biopsy, would be required in future for an
improved outcome. Secondly, with the exception of recurrence of
primary lesions or metastases, the occurrence of novel MPMNs should
be considered during follow-up. Thirdly, multidisciplinary
treatment can substantially increase the survival of patients with
MPMNs.
In the present study, multidisciplinary treatment
based on surgery exhibited a significant survival advantage for a
patient with a rare case of MPMN. However, further research with
additional cases, particularly including patients with more than
two MPMNs, is required to definitively prove the clinical benefit
of multidisciplinary treatment for the overall survival of patients
with MPMNs.
References
|
1
|
Hulikal N, Ray S, Thomas J and Fernandes
DJ: Second primary malignant neoplasms: A clinicopathological
analysis from a cancer centre in India. Asian Pacific J Cancer
Prev. 13:6087–6091. 2012. View Article : Google Scholar
|
|
2
|
van Westreenen HL, Westerterp M, Jager PL,
et al: Synchronous primary neoplasms detected on 18F-FDG PET in
staging of patients with esophageal cancer. J Nucl Med.
46:1321–1325. 2005.PubMed/NCBI
|
|
3
|
Gursel B, Meydan D, Özbek N, Ozdemir O and
Odabas E: Multiple primary malignant neoplasms from the black sea
region of Turkey. J Int Med Res. 39:667–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hayat MJ, Howlader N, Reichman ME and
Edwards BK: Cancer statistics, trends, and multiple primary cancer
analyses from the Surveillance, Epidemiology, and End Results
(SEER) Program. Oncologist. 12:20–37. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Luciani A and Balducci L: Multiple primary
malignancies. Seminars in oncology. 31:264–273. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nagasawa S, Onda M, Sasajima K, Takubo K
and Miyashita M: Multiple primary malignant neoplasms in patients
with esophageal cancer. Dis Esophagus. 13:226–230. 2000. View Article : Google Scholar
|
|
7
|
Naomoto Y, Haisa M, Yamatsuji T, et al:
Multiple primary cancers of the esophagus and thyroid gland. Jpn J
Clin Oncol. 29:349–352. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
López Mollá C, Estellés Ferriol E,
Carrasco Llatas M, Seijas Rosales T, Morales Suárez-Varela M and
Dalmau Galofre J: Malignant multiple neoplasms in head and neck
squamous cell carcinoma. Acta Otorrinolaringol Esp. 59:427–432.
2008.(In Spanish). View Article : Google Scholar
|
|
9
|
Billroth T: The general surgical pathology
and therapy. A handbook for students and doctors. Reimer G: 14th
editino. Auflage, Berlin: pp. 9081889, (In German).
|
|
10
|
Warren S and Gates O: Multiple primary
malignant tumors: a survey of the literature and a statistical
study. Am J cancer. 16:1358–1414. 1932.
|
|
11
|
Bumpers HL, Natesha RK, Barnwell SP and
Hoover EL: Multiple and distinct primary cancers: a case report. J
Natl Med Assoc. 86:387–388. 1994.PubMed/NCBI
|
|
12
|
Kubota T, Sato K, Takeuchi H and Handa Y:
Successful removal after radiotherapy and vascular embolization in
a huge tentorial epithelioid hemangioendothelioma: a case report. J
Neurooncol. 68:177–183. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zheng J, Liu L, Wang J, Wang S, Cao Y and
Zhao J: Primary intracranial epithelioid hemangioendothelioma: a
low-proliferation tumor exhibiting clinically malignant behavior. J
Neurooncol. 110:119–127. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Endo T, Su CC, Numagami Y and Shirane R:
Malignant intracranial epithelioid hemangioendothelioma presumably
originating from the lung: case report. J Neurooncol. 67:337–343.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Miettinen M, Lindenmayer AE and Chaubal A:
Endothelial cell markers CD31, CD34, and BNH9 antibody to H- and
Y-antigens-evaluation of their specificity and sensitivity in the
diagnosis of vascular tumors and comparison with von Willebrand
factor. Mod Pathol. 7:82–90. 1994.PubMed/NCBI
|
|
16
|
Unni KK and Inwards CY: Ewing tumor.
Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 6th
edition. Philadelphia: Lippincott-Raven; pp. 211–224. 2000
|
|
17
|
Pritchard DJ, Dahlin DC, Dauphine RT,
Taylor WF and Beabout JW: Ewing’s sarcoma. A clinicopathological
and statistical analysis of patients surviving five years or
longer. J Bone Joint Surg Am. 57:10–16. 1975.PubMed/NCBI
|
|
18
|
Barbieri E, Chiaulon G, Bunkeila F, et al:
Radiotherapy in vertebral tumors. Indications and limits: a report
on 28 cases of Ewing’s sarcoma of the spine. Chir Organi Mov.
83:105–111. 1998.PubMed/NCBI
|
|
19
|
Villas C and San Julian M: Ewing’s tumor
of the spine: report on seven cases including one with a 10-year
follow-up. Eur Spine J. 5:412–417. 1996. View Article : Google Scholar
|
|
20
|
Kaspers GJ, Kamphorst W, van de Graaff M,
van Alpen HA and Veerman AJ: Primary spinal epidural extraosseous
Ewing’s sarcoma. Cancer. 68:648–654. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shin JH, Lee HK, Rhim SC, Cho KJ, Choi CG
and Suh DC: Spinal epidural extraskeletal Ewing sarcoma: MR
findings in two cases. AJNR Am J Neuroradiol. 22:795–798.
2001.PubMed/NCBI
|
|
22
|
Desai KI, Nadkarni TD, Goel A, Muzumdar
DP, Naresh KN and Nair CN: Primary Ewing’s sarcoma of the cranium.
Neurosurgery. 46:62–69. 2000. View Article : Google Scholar
|
|
23
|
Patra S, Vij M, Venugopal K and Rela M:
Hepatic solitary fibrous tumor: report of a rare case. Indian J
Pathol Microbiol. 55:236–238. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fuksbrumer MS, Klimstra D and Panicek DM:
Solitary fibrous tumor of the liver: imaging findings. AJR Am J
Roentgenol. 175:1683–1687. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chithriki M, Jaibaji M and Vandermolen R:
Solitary fibrous tumor of the liver with presenting symptoms of
hypoglycemic coma. Am Surg. 70:291–293. 2004.PubMed/NCBI
|
|
26
|
Brochard C, Michalak S, Aubé C, et al: A
not so solitary fibrous tumor of the liver. Gastroenterol Clin
Biol. 34:716–720. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Korkolis DP, Apostolaki K, Aggeli C, et
al: Solitary fibrous tumor of the liver expressing CD34 and
vimentin: a case report. World J Gastroenterol. 14:6261–6264. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Nakata S, Takahashi H, Takezawa Y,
Kobayashi M, Suzuki T and Kawashima K: Clinical features of
multiple primary cancers including prostate cancer. Hinyokika Kiyo.
46:385–391. 2000.(In Japanese). PubMed/NCBI
|
|
29
|
Travis LB, Rabkin CS, Brown LM, et al:
Cancer survivorship- genetic susceptibility and second primary
cancers: research strategies and recommendations. J Natl Cancer
Inst. 98:15–25. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Inskip PD: Multiple primary tumors
involving cancer of the brain and central nervous system as the
first or subsequent cancer. Cancer. 98:562–570. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tateishi U, Hasegawa T, Yamamoto S, et al:
Incidence of multiple primary malignancies in a cohort of adult
patients with soft tissue sarcoma. Jpn J Clin Oncol. 35:444–452.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Demandante CG, Troyer DA and Miles TP:
Multiple primary malignant neoplasms: case report and a
comprehensive review of the literature. Am J Clin Oncol. 26:79–83.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Suzuki S, Nishimaki T, Suzuki T, Kanda T,
Nakagawa S and Hatakeyama K: Outcomes of simultaneous resection of
synchronous esophageal and extraesophageal carcinomas. J Am Coll
Surg. 195:23–29. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Parajón A and Vaquero J: Meningel
intracranial epithelioid hemangioendothelioma: case report and
literature review. J Neurooncol. 88:169–173. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sato S, Mitsuyama T, Ishii A, Kawakami M
and Kawamata T: Multiple primary cranial Ewing’s sarcoma in
adulthood: case report. Neurosurgery. 64:E384–E386. 2009.
View Article : Google Scholar
|
|
36
|
Archontaki M, Korkolis DP, Arnogiannaki N,
et al: Histologically malignant solitary fibrous tumour of the
anterior thoracic wall: a case report and review of the literature.
Case Rep Med. 2010:2571672010.PubMed/NCBI
|
|
37
|
Kharchenko VP, Chkhikvadze VD, Galil-Ogly
GA, et al: Multiple primary malignant neoplasms and survival of
patients with stage-I lung cancer. Vopr Onkol. 41:75–78. 1995.(In
Russian).
|
|
38
|
Dhooge IJ, De Vos M and Van Cauwenberge
PB: Multiple primary malignant tumors in patients with head and
neck cancer: results of a prospective study and future
perspectives. Laryngoscope. 108:250–256. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Salem A, Abu-Hijlih R, Abdelrahman F, et
al: Multiple primary malignancies: Analysis of 23 patients with at
least three tumors. J Gastrointest Cancer. 43:437–443. 2012.
View Article : Google Scholar
|