Introduction
Gliomas account for 80% of malignant brain tumors
and are rarely curable (1–3). The traditional treatments, including
surgical excision, chemotherapy and radiotherapy, have limited
effects on gliomas. Targeted therapy is a promising approach for
cancer treatment, but identification of the tumor-specific target
remains difficult (4–6). In recent years, a scorpion-derived
polypeptide chlorotoxin (CTX) was found to selectively bind
malignant gliomas (7,8) mediated by the cell surface matrix
metalloproteinase-2 (MMP-2) and annexin-2, whose expression is
increased in gliomas (9,10). CTX was first isolated from the
scorpion venom in 1993 and is composed of 36 amino acids and four
disulfide bonds (11). In previous
years, the glioma-binding properties of CTX have been extensively
investigated and CTX conjugates have been developed for the
treatment and diagnosis of gliomas and other malignant tumors
(12–21). The radioactive iodine-131-labeled
CTX has been designated as an orphan drug for the treatment of
malignant glioma and melanoma by the US Food and Drug
Administration, and other fluorescent dye- or nanoparticle-labeled
CTXs also show great potential for glioma diagnosis and treatment
(22).
Onconase (Onc) is a small RNase that was first
isolated from oocytes of the northern leopard frog (Rana
pipiens) in 1988 (23). Onc is
composed of 104 amino acids and four disulfide bonds (24), and shares a similar tertiary
structure with other members of the ribonuclease A superfamily
(25). Subsequent to its
identification, Onc was revealed to exhibit anti-tumor properties,
as it can enter the tumor cells, degrade RNA and cause cell death
(26–29); thus, Onc is being developed as an
anti-tumor drug for several types of malignant tumors (30–33).
As CTX exhibits glioma-targeting properties and Onc exhibits
cytotoxicity, in the present study a CTX-conjugated Onc (CTX-Onc)
was prepared for the analysis of its anti-glioma effects on
cultured glioma cells and on a mouse model.
Materials and methods
Preparation of the recombinant CTX and
Onc
The recombinant CTX was prepared from a
GST-6′His-CTX precursor by enzymatic cleavage and in vitro
refolding, according to our previously described procedure
(34). The recombinant Onc was
prepared through heterologous expression of an N-terminally
6xHis-tagged Onc (6xHis-Onc) precursor by enzymatic cleavage,
N-terminal cyclization and in vitro refolding, according to
our previously described procedure (35).
Chemical conjugation of the recombinant
CTX with the recombinant Onc
To label CTX with N-Succinimidyl
3-(2-pyrdydithio)propionate (SPDP; Thermo Fisher Scientific,
Rockford, IL, USA), the lyophilized recombinant CTX was dissolved
in 1.0 mM aqueous HCl (Sinopharm, Beijing, China)and the SPDP
reagent in dimethylsulfoxide (DMSO). To start the reaction, they
were mixed together at equal concentrations (400 μm each) in the
reaction buffer (50 mM phosphate and 150 mM NaCl; pH 8.0) and
incubated at room temperature for 1 h. Subsequent to the reaction
mixture being acidified to pH 3.0 by trifluoroacetic acid (Merck
KGaA, Darmstadt, Germany), high performance liquid chromatography
(Agilent Technologies, Santa Clara, CA, USA) was applied to the
mixture, according to our previously described chromatography
methods (35). The labeled CTX
fractions were eluted from a C18 reverse-phase column (Agilent
Technologies) by an acidic acetonitrile gradient, manually
collected, and lyophilized.
To label Onc with 2-iminothiolane (Thermo Fisher
Scientific), the recombinant Onc was dissolved in 1.0 mM aqueous
HCl and the reagent 2-iminothiolane in DMSO. To start labeling, Onc
(50 μM at final) and 2-iminothiolane (1 mM at final) were mixed in
the reaction buffer (50 mM phosphate and 150 mM NaCl; pH 8.0) and
incubated at room temperature for 1 h. Thereafter, the reaction
mixture was acidified to pH 3.0 by acetic acid and applied to gel
filtration. The Onc fraction was eluted from a Sephadex®
G-25 column (Sinopharm) by 10% aqueous acetic acid, manually
collected and lyophilized.
To prepare the CTX-Onc conjugate, the SPDP-labeled
CTX and the 2-iminothiolane labeled Onc were dissolved in 1.0 mM
aqueous HCl, respectively. To start conjugation, they were mixed
together at equal concentrations (50 μM each) in the reaction
buffer (50 mM NaPO4 and 150 mM NaCl; pH 8.0) and
incubated at room temperature for 0.5 h. Thereafter, the reaction
mixture was acidified to pH 3.0 by acetic acid and applied to gel
filtration. The CTX-Onc conjugate was eluted from the
Sephadex® G-25 column by 10% acetic acid and
lyophilized.
Cytocoxicity of the CTX-Onc conjugate on
the cultured glioma cells
Human glioma U251 and SHG-44 cells were purchased
from the Cell Bank, Shanghai Institutes For Biological Sciences,
Chinese Academy of Sciences (Shanghai, China) and cultured in
Dulbecco’s modified Eagle’s medium supplemented with 10% fetal
bovine serum and antibiotics, at 37°C in a CO2
incubator. For the cytotoxicity assay, the cells were seeded into a
96-well plate (5×103 cells/well). The subsequent day,
the cells were changed into the medium containing different
concentrations of CTX-Onc conjugate or the physical mixture of CTX
and Onc (CTX + Onc), and were continuously cultured for 36 h.
Thereafter, the cell viability was assayed using the MTT method
(MTT assay kiy; Solarbio, Beijing, China).
Anti-glioma effect of the CTX-Onc
conjugate on a nude mouse model
All animal experiments were approved by the Animal
Care and Use Committee of Tongji University (Shanghai, China). The
five-week-old male athymic mice (BALB/c) were obtained from
Shanghai Laboratory Animal Center (Shanghai, China). The cultured
U251 cells (5×107 cells/mouse) were suspended in 200 μl
phosphate-buffered saline (PBS) containing 50% Matrigel™ (BD
Biosciences, Franklin Lakes, NJ, USA) and subcutaneously injected
into the nude mice. The dimensions (length and width) of the tumors
were measured by calipers, and the tumor burden was calculated
using the following formula: 0.5 × length × width2. Once
the tumor had grown to 200–300 mm3, it was removed and
cut into uniform tablets (size, 10–20 mm3) subsequent to
the mouse being sacrificed in a CO2 chamber, and then
the tumor tablets (one tablet/mouse) were subcutaneously injected
into the nude mice. The cultured SHG-44 cells (1×107
cells/mouse) were suspended in 200 μl PBS and subcutaneously
injected into the nude mice.
Two months after inoculation with the tablets, the
nude mice bearing the U251 tumors were randomly divided into three
groups (n=3 mice/group), and two of the groups were intravenously
injected at 2.5 mg/kg with 0.2 ml CTX + Onc mixture dissolved in
PBS and CTX-Onc conjugate dissolved in PBS, respectively, twice a
week for ~1 month. The other group was intravenously injected with
0.2 ml PBS by the same method as a control. The nude mice bearing
SHG-44 tumors were only divided into three groups (n=5 mice/group)
two months after inoculation, and were then given the same
treatment as the nude mice bearing the U251 tumors. The dimensions
of the tumors and the weights of the mice were measured at least
twice a week and recorded during the treatments.
Results
Chemical conjugation of the recombinant
CTX and Onc
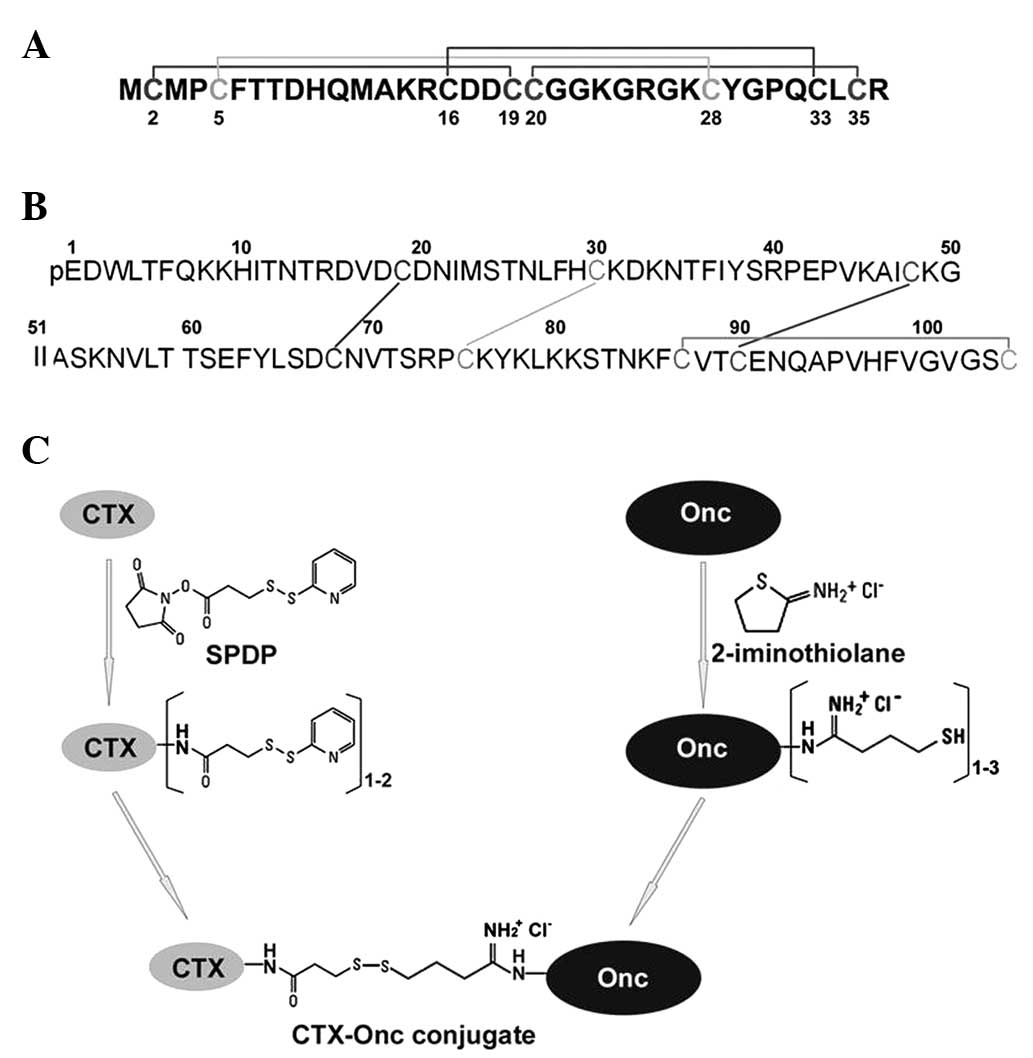
As CTX can selectively bind malignant gliomas, the
present study attempted to use it to target Onc toward gliomas. To
prepare the CTX-Onc conjugate, an efficient conjugation procedure
was established by which CTX and Onc were covalently crosslinked
through reversible disulfide bond(s) (Fig. 1). Firstly, active disulfide(s) were
introduced into the recombinant CTX by chemical modification using
the primary amine-specific reagent SDPD, while free thiol(s) were
introduced into the recombinant Onc by chemical modification using
the primary amine-specific reagent 2-iminothiolane. Secondly,
CTX-Onc conjugates were formed via reaction of the introduced free
thiol(s) of the modified Onc with the introduced active disulfide
bond(s) of the modified CTX. Owing to the presence of the
reversible disulfide crosslinking in the present CTX-Onc conjugate,
free Onc is likely to be released from the conjugate and to enter
the glioma cells to exert its cytotoxicity, since the disulfide
crosslinking may be reduced by the reductive redox potential at the
cell membrane.
CTX has four primary amine moieties, including one
N-terminal α-amine and three internal ɛ-amines of the side-chain of
lysine (Lys) residues (Fig. 1A).
These primary amine moieties would all react with the primary
amine-specific modification reagent SPDP during chemical
modification. Thus, seven major peaks were eluted from the C18
reverse-phase column following SPDP modification, although the
ratio of CTX to SPDP was carefully controlled (Fig. 2A). Mass spectrometry analyses showed
that the first peak (indicated by a star) was the unlabeled CTX
(measured molecular mass, 3,998.0; theoretical value, 3,996.8);
peaks 2–4 were the mono-labeled CTXs (indicated by a letter ‘m’)
carrying one active disulfide bond (measured molecular mass,
4,193.0; theoretical value, 4,194.8); peaks 5–7 were the di-labeled
CTXs (indicated by a letter ‘d’) carrying two active disulfide
bonds (measured molecular mass, 4,391.0; theoretical value,
4,391.8). In the subsequent conjugation reaction, the mono-labeled
and di-labeled CTXs were mixed together and reacted with the
modified Onc.
 | Figure 2Preparation of the CTX-Onc conjugate.
(A) Purification of the SPDP-modified CTXs by rp-HPLC. The peak of
unlabeled CTX was indicated by *; the peaks of mono-labeled CTXs
were indicated by the letter ‘m’; the peaks of di-labeled CTXs were
indicated by the letter ‘d’. (B) Purification of the
2-iminothiolane-modified Onc by gel filtration. The first peak was
the eluted Onc fraction (indicated by *) and the second peak was
the excess modification reagent. (C) Purification of CTX-Onc
conjugate by gel filtration. The first peak was the eluted CTX-Onc
fraction (indicated by *) and the second peak was the salts in the
reaction buffer. (D) Tricine SDS-PAGE analysis. Lane M, protein
marker; lane 1, the SPDP-modified CTX; lane 2, the
2-iminothiolane-modified Onc; lane 3, CTX-Onc conjugate; lane 4,
CTX-Onc conjugate treated by DTT. CTX, chlorotoxin; Onc, onconase;
SPDP, N-Succinimidyl 3-(2-pyrdydithio)propionate; rp-HPLC, reverse
phase high performance liquid chromatography; DTT,
dithiothreitol. |
Although Onc has no N-terminal α-amine moiety due to
the formation of a pyroglutamate residue, it has 12 internal
ɛ-amine moieties of the side-chain of Lys residues (Fig. 1B). All these internal primary amine
moieties would react with the reagent 2-iminothiolane, thus the
reaction condition was optimized by controlling the ratio of Onc to
2-iminothiolane during the modification. Subsequently the excess
2-iminothiolane was removed by gel filtration (Fig. 2B) and the eluted Onc fraction was
analyzed by mass spectrometry; 1–3 free thiol moieties were
introduced into the majority of Onc molecules (measured molecular
mass, 11,920.0, 12,022.0 or 12,121.0). In the subsequent
conjugation reaction, the modified Onc mixture was used for
conjugation with the SDPD-modified CTX.
To form the CTX-Onc conjugate, the SPDP-modified CTX
and the 2-iminothiolane-modified Onc were mixed at a molar ratio of
1:1. Following the reaction, the CTX-Onc conjugate was eluted from
a gel filtration column by 5% aqueous acetic acid (Fig. 2C) and analyzed by tricine SDS-PAGE
(Fig. 2D). The CTX-Onc conjugate
(lane 3) showed smear bands as it contained different numbers of
CTX and Onc. Subsequent to treatment by the reducing reagent
dithiothreitol, the conjugate (lane 4) showed two sharp bands
corresponding to the modified CTX (lane 1) and the modified Onc,
respectively. Thus, the conjugate was sensitive to the reducing
condition and the Onc would be released from the conjugate under
reducing conditions.
Cytotoxicity of the CXT-Onc conjugate to
the cultured glioma cells
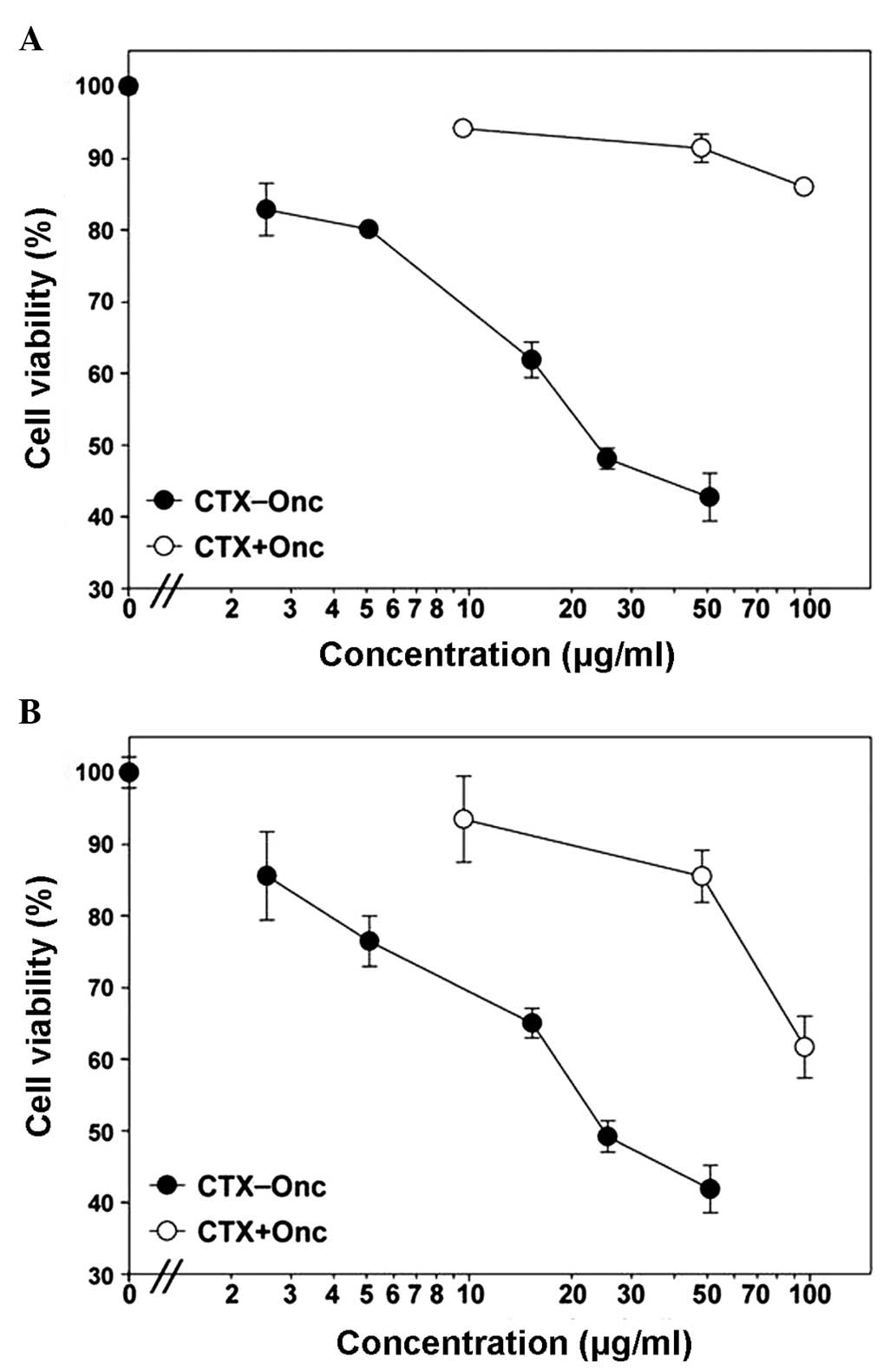
To test the anti-glioma effect of the CTX-Onc
conjugate, its cytotoxicity to the cultured glioma cells was first
measured. To test the targeting effect of CTX, the CTX + Onc
mixture at equal molar ratio was used as a control, designated as
CTX + Onc. Subsequent to treatment either by CTX-Onc conjugate or
by CTX + Onc mixture, the viability of the glioma cells were
measured by MTT assay. As shown in Fig.
3, the CTX-Onc conjugate had a dose-dependent cytotoxicity to
the U251 and SHG-44 cells, with the concentration to inhibit cell
survival to 50% (SF50) of ~20 μg/ml to the two cell types.
Furthermore, the conjugate showed much higher (>10-fold)
cytotoxicity than the CTX + Onc mixture, suggesting that CTX
targeted more Onc to glioma cells and significantly enhanced its
cytotoxicity.
Anti-glioma effects of the CTX-Onc
conjugate on a mouse model
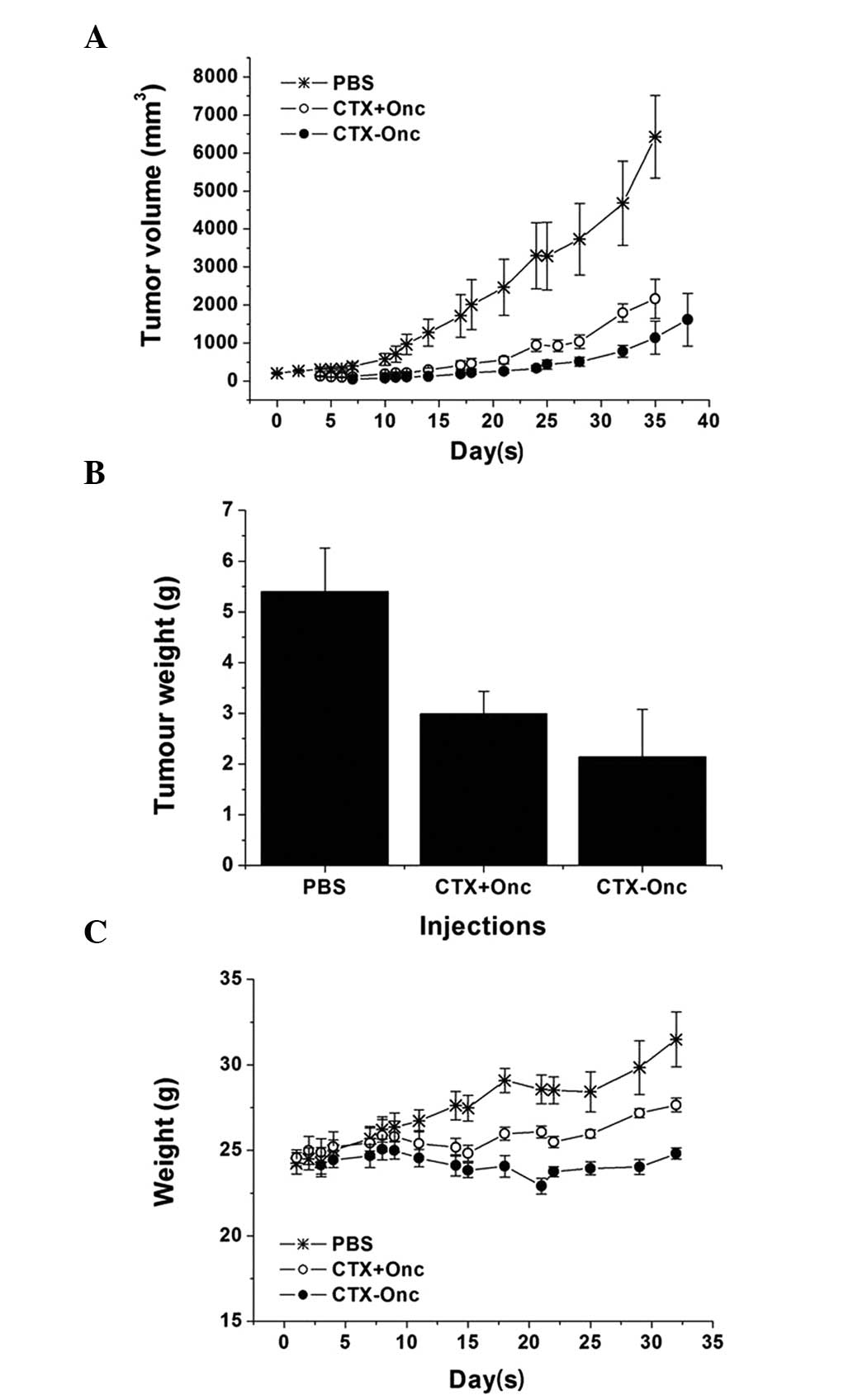
As the CTX-Onc conjugate had a significant
anti-glioma effect on cultured cells, its effect was further tested
on nude mice bearing either U251 or SHG-44 tumors. As shown in
Fig. 4A, when the mice bearing
subcutaneous U251 tumors were treated with CTX-Onc conjugate, CTX +
Onc mixture or PBS for a month, the CTX-Onc conjugate showed the
highest inhibition effect on the tumor growth, suggesting that CTX
also had a targeting effect in vivo. Subsequent to the mice
being sacrificed at the end of treatment, the mean tumor weight of
the CTX-Onc group was also lower than that of the CTX + Onc group,
confirming the CTX targeting effect (Fig. 4B).
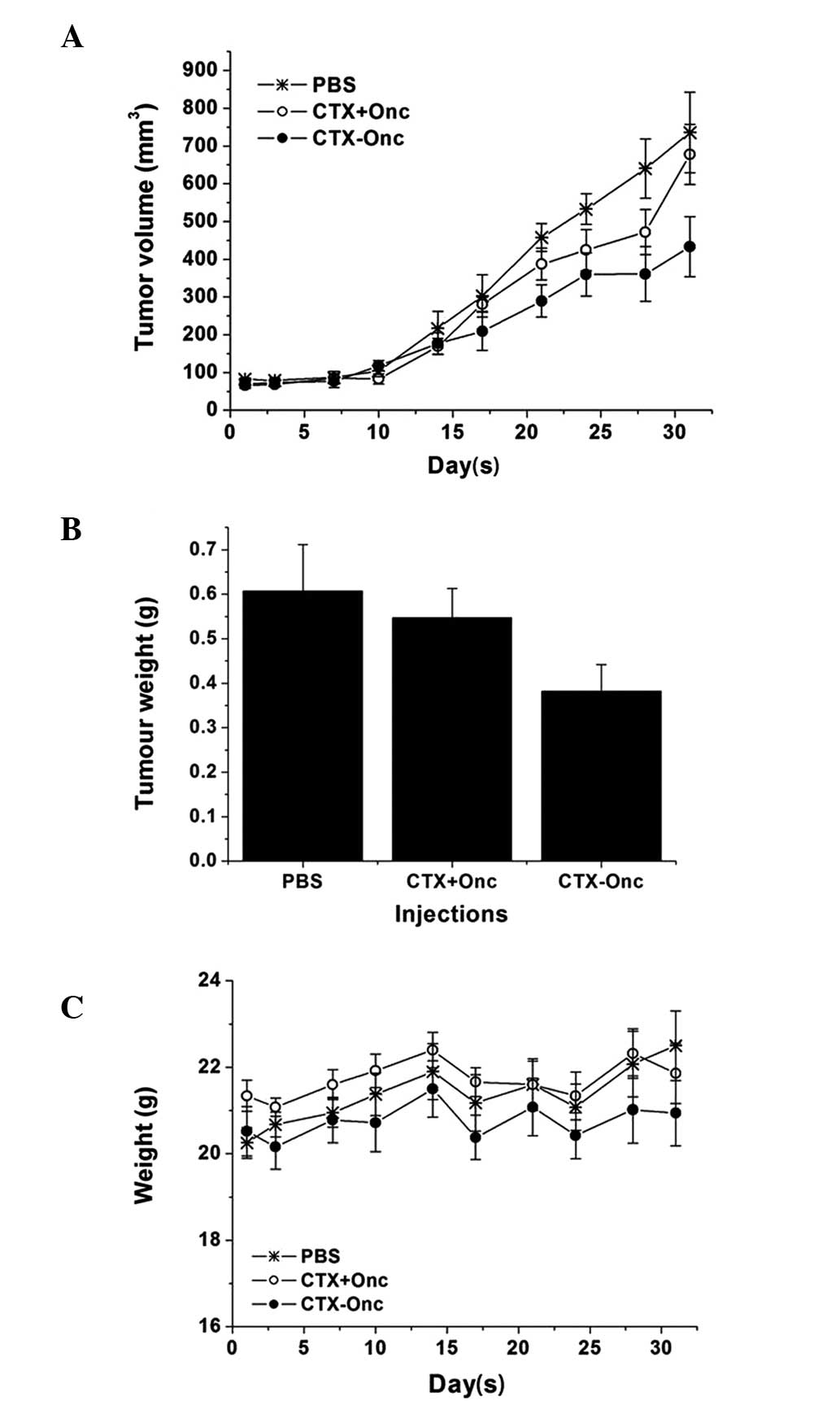
The effect of the CTX-Onc conjugate on the mice
bearing the subcutaneous SHG-44 tumors was also tested. After ~1
month of treatment, the CTX-Onc conjugate also showed the highest
inhibition effect on tumor growth (Fig.
5A), and it also suggested that CTX had a targeting effect
in vivo. Subsequent to the mice being sacrificed at the end
of treatment, the mean tumor weight of the CTX-Onc group was also
lower than that in the CTX + Onc group, confirming the CTX
targeting effect again (Fig. 5B).
As shown in Figs. 4C and 5C, the mean weights of the CTX-Onc group
were not significantly affected during the treatment, suggesting
that the CTX-Onc conjugate exhibited a low toxicity in
vivo.
Discussion
Malignant gliomas are common malignant tumors in the
central nervous system. Due to the rapid proliferation and poor
differentiation of gliomas, and the limited effects of the
traditional treatments on gliomas, patients generally have a poor
prognosis (2,3). Therefore, targeted therapy based on
the identification of the tumor-specific target is deemed to be a
promising approach for malignant glioma treatment. CTX can
selectively bind malignant gliomas, and now TM-601
(I131-labeled CTX) has been used as a drug for gliomas
in a clinical trial (36). However,
the cytotoxicity of CTX is not strong enough to result in tumor
cell apoptosis, therefore there was a requirement to link it with a
molecule that can cause the tumor cell apoptosis. Onc exhibits
anti-tumor effects on various tumors, with few side-effects, and
has been used as a drug to treat malignant pleural mesothelioma
(MPM) in a phase III clinical trial (37). Onc was selected to be linked to CTX
in the preparation of an anti-glioma drug in the present study.
There were two methods of preparation. One method was to construct
the fusion gene of CTX and Onc, but the eight disulfide bonds
contained by the fusion proteins of CTX and Onc may have resulted
in difficulty in refolding of the fusion protein in vitro.
Therefore the other method of preparation was selected. The
recombinant CTX and Onc were respectively obtained and linked by a
disulfide bond to prepare the CTX-Onc conjugate, rather than use of
the chemical linkage, which was always used in preparation for the
monoclonal antibody-targeted drugs and can be broken in the
lysosome. Since it was not clear whether the membrane protein,
particularly MMP-2, on the glioma cell surface bound by CTX could
enter the cells by endocytosis, in order to prepare the CTX-Onc
conjugate, a reversible chemical crosslinking approach was
established. By reaction with the primary amine-specific
bifunctional reagent SPDP, active disulfide bond(s) were introduced
into the recombinant CTX; by reaction with the primary
amine-specific reagent 2-iminothiolane, free thiol group(s) were
introduced into the recombinant Onc. Via reaction of free thiol(s)
of the modified Onc with active disulfide bond(s) of the modified
CTX, the CTX-Onc conjugate was obtained. It was expected that the
disulfide bond between CTX and Onc could be broken by the reducing
power on the cell surface when the CTX-Onc conjugate bound to the
glioma cells by CTX, and that the Onc released could enter cells by
electrostatic interaction and endocytosis to degrade RNA in the
glioma cells.
The results of the in vitro and in
vivo experiments demonstrated that the CTX-Onc conjugate
exhibited an improved anti-tumor effect compared with the CTX + Onc
mixture, suggesting that CTX could target more Onc to glioma cells
and significantly enhance its cytotoxicity. The anti-tumor effect
of CTX-Onc is similar to that of the CTX-conjugated nanoparticle
(NP-MTX-CTX) reported by Sun et al in vitro, which was
capable of inhibiting >50% of glioma cell survival at ~100 μg/ml
(14). Furthermore, the anti-tumor
effect of the CTX-Onc conjugate is greater than that of the
CTX-based conjugate (ClTx-LS) reported by Xiang et al in
vivo, which had an inhibition ratio of ~34% compared that of
the saline group, at 5 mg/kg (38).
When compared with the inhibition ratio of the CTX + Onc mixture on
tumor growth in vivo, the ratio of the CTX-Onc conjugate
increased by 15–30%. In addition, it was revealed that the
injection method could impact on the inhibitory effect of the
CTX-Onc conjugate on gliomas in vivo. The intraperitoneal
injection with CTX-Onc conjugate did not result in any inhibitory
effect on the growth of the glioma. This may be associated with the
large molecular weight of the CTX-Onc conjugate, which is prevented
from entering the blood system, or with the fact that the CTX-Onc
conjugate may be digested by proteases in the peritoneal cavity.
Finally, intravenous injection was selected as the method of drug
delivery. Although the orthotopic glioma model in vivo was
not used to determinate the anti-tumor effect of the CTX-Onc
conjugate in the present study, the in vivo results can be
used as the basis for the future clinical study of the CTX-Onc
conjugate, since the drug delivery in the treatment of gliomas in
clinical practice can be made through the cerebrospinal fluid to
avoid the blood-brain barrier. Therefore, the CTX-Onc conjugate
designed in the present study can be used as a novel potential
anti-glioma drug for further studies.
Acknowledgements
This study was supported by the Chinese Major
Scientific and Technological Special Project for ‘Major New Drugs
Creation’ (grant no. 2009ZX09103-656).
References
|
1
|
Tanaka S, Louis DN, Curry WT, Batchelor TT
and Dietrich J: Diagnostic and therapeutic avenues for
glioblastoma: no longer a dead end? Nat Rev Clin Oncol. 10:14–26.
2013. View Article : Google Scholar
|
|
2
|
Watkins S and Sontheimer H: Unique biology
of gliomas: challenges and opportunities. Trends Neurosci.
35:546–556. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lima FR, Kahn SA, Soletti RC, et al:
Glioblastoma: therapeutic challenges, what lies ahead. Biochim
Biophys Acta. 1826:338–349. 2012.PubMed/NCBI
|
|
4
|
Patel M, Vogelbaum MA, Barnett GH, et al:
Molecular targeted therapy in recurrent glioblastoma: current
challenges and future directions. Expert Opin Investig Drugs.
21:1247–1266. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Polivka J Jr, Polivka J, Rohan V, Topolcan
O and Ferda J: New molecularly targeted therapies for glioblastoma
multiforme. Anticancer Res. 32:2935–2946. 2012.PubMed/NCBI
|
|
6
|
Agarwal S, Sane R, Oberoi R, Ohlfest JR
and Elmquist WF: Delivery of molecularly targeted therapy to
malignant glioma, a disease of the whole brain. Expert Rev Mol Med.
13:e172011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Soroceanu L, Gillespie Y, Khazaeli MB and
Sontheimer H: Use of chlorotoxin for targeting of primary brain
tumors. Cancer Res. 58:4871–4879. 1998.PubMed/NCBI
|
|
8
|
Lyons SA, O’Neal J and Sontheimer H:
Chlorotoxin, a scorpion-derived peptide, specifically binds to
gliomas and tumors of neuroectodermal origin. Glia. 39:162–173.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Deshane J, Garner CC and Sontheimer H:
Chlorotoxin inhibits glioma cell invasion via matrix
metalloproteinase-2. J Biol Chem. 278:4135–4144. 2003. View Article : Google Scholar
|
|
10
|
Kesavan K, Ratliff J, Johnson EW, et al:
Annexin A2 is a molecular target for TM601, a peptide with
tumor-targeting and anti-angiogenic effects. J Biol Chem.
285:4366–4374. 2010. View Article : Google Scholar :
|
|
11
|
DeBin JA, Maggio JE and Strichartz GR:
Purification and characterization of chlorotoxin, a chloride
channel ligand from the venom of the scorpion. Am J Physiol.
264:C361–C369. 1993.PubMed/NCBI
|
|
12
|
Veiseh M, Gabikian P, Bahrami SB, et al:
Tumor paint: a chlorotoxin: Cy5.5 bioconjugate for intraoperative
visualization of cancer foci. Cancer Res. 67:6882–6888. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sun C, Veiseh O, Gunn J, et al: In vivo
MRI detection of gliomas by chlorotoxin-conjugated
superparamagnetic nanoprobes. Small. 4:372–379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sun C, Fang C, Stephen Z, et al:
Tumor-targeted drug delivery and MRI contrast enhancement by
chlorotoxin-conjugated iron oxide nanoparticles. Nanomedicine
(Lond). 3:495–505. 2008. View Article : Google Scholar
|
|
15
|
Veiseh O, Kievit FM, Gunn JW, Ratner BD
and Zhang M: A ligand-mediated nanovector for targeted gene
delivery and transfection in cancer cells. Biomaterials.
30:649–657. 2009. View Article : Google Scholar :
|
|
16
|
Veiseh O, Gunn JW, Kievit FM, et al:
Inhibition of tumor-cell invasion with chlorotoxin-bound
superparamagnetic nanoparticles. Small. 5:256–264. 2009. View Article : Google Scholar :
|
|
17
|
Orndorff RL and Rosenthal SJ: Neurotoxin
quantum dot conjugates detect endogenous targets expressed in live
cancer cells. Nano Lett. 9:2589–2599. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Veiseh O, Sun C, Fang C, et al: Specific
targeting of brain tumors with an optical/magnetic resonance
imaging nanoprobe across the blood-brain barrier. Cancer Res.
69:6200–6207. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kievit FM, Veiseh O, Fang C, et al:
Chlorotoxin labeled magnetic nanovectors for targeted gene delivery
to glioma. ACS Nano. 4:4587–4594. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang R, Han L, Li J, et al:
Chlorotoxin-modified macromolecular contrast agent for MRI tumor
diagnosis. Biomaterials. 32:5177–5186. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fu Y, An N, Li K, Zheng Y and Liang A:
Chlorotoxin-conjugated nanoparticles as potential glioma-targeted
drugs. J Neurooncol. 107:457–462. 2012. View Article : Google Scholar
|
|
22
|
Cheng Y, Zhao J, Qiao W and Chen K: Recent
advances in diagnosis and treatment of gliomas using
chlorotoxin-based bioconjugates. Am J Nucl Med Mol Imaging.
4:385–405. 2014.PubMed/NCBI
|
|
23
|
Darzynkiewicz Z, Carter SP, Mikulski SM,
Ardelt WJ and Shogen K: Cytostatic and cytotoxic effects of Pannon
(P-30 Protein), a novel anticancer agent. Cell Tissue Kinet.
21:169–182. 1988.PubMed/NCBI
|
|
24
|
Ardelt W, Mikulski SM and Shogen K: Amino
acid sequence of an anti-tumor protein from Rana pipiens oocytes
and early embryos. Homology to pancreatic ribonucleases. J Biol
Chem. 266:245–251. 1991.PubMed/NCBI
|
|
25
|
Mosimann SC, Ardelt W and James MN:
Refined 1.7 A X-ray crystallographic structure of P-30 protein, an
amphibian ribonuclease with anti-tumor activity. J Mol Biol.
236:1141–1153. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wu Y, Mikulski SM, Ardelt W, Rybak SM and
Youle RJ: A cytotoxic ribonuclease. Study of the mechanism of
onconase cytotoxicity. J Biol Chem. 268:10686–10693.
1993.PubMed/NCBI
|
|
27
|
Saxena SK, Sirdeshmukh R, Ardelt W, et al:
Entry into cells and selective degradation of tRNAs by a cytotoxic
member of the RNase A family. J Biol Chem. 277:15142–15146. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Suhasini AN and Sirdeshmukh R: Transfer
RNA cleavages by onconase reveal unusual cleavage sites. J Biol
Chem. 281:12201–12209. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rodríguez M, Torrent G, Bosch M, et al:
Intracellular pathway of Onconase that enables its delivery to the
cytosol. J Cell Sci. 120:1405–1411. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Newton DL, Hansen HJ, Mikulski SM, et al:
Potent and specific antitumor effects of an anti-CD22-targeted
cytotoxic ribonuclease: potential for the treatment of non-Hodgkin
lymphoma. Blood. 97:528–535. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pavlakis N and Vogelzang NJ: Ranpirnase-an
antitumour ribonuclease: its potential role in malignant
mesothelioma. Expert Opin Biol Ther. 6:391–399. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lee I, Kalota A, Gewirtz AM and Shogen K:
Antitumor efficacy of the cytotoxic RNase, ranpirnase, on A549
human lung cancer xenografts of nude mice. Anticancer Res.
27:299–307. 2007.PubMed/NCBI
|
|
33
|
Chang CH, Gupta P, Michel R, et al:
Ranpirnase (frog RNase) targeted with a humanized, internalizing,
anti-Trop-2 antibody has potent cytotoxicity against diverse
epithelial cancer cells. Mol Cancer Ther. 9:2276–2286. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wang XM, Luo X and Guo ZY: Recombinant
expression and downstream processing of the disulfide-rich
tumor-targeting peptide chlorotoxin. Exp Ther Med. 6:1049–1053.
2013.PubMed/NCBI
|
|
35
|
Wang XM and Guo ZY: Recombinant
expression, different downstream processing of the disulfide-rich
anti-tumor peptide Ranpirnase and its effect on the growth of human
glioma cell line SHG-44. Biomed Rep. 1:747–750. 2013.
|
|
36
|
Hockaday DC, Shen S, Fiveash J, et al:
Imaging glioma extent with 131I-TM-601. J Nucl Med. 46:580–586.
2005.PubMed/NCBI
|
|
37
|
Pavlakis N and Vogelzang NL: Ranpirnase-an
antitumor ribonuclease: its potential role in malignant
mesothelioma. Expert Opin Biol Therm. 6:391–399. 2006. View Article : Google Scholar
|
|
38
|
Xiang Y, Liang L, Wang X, et al: Chloride
channel-mediated brain glioma targeting of chlorotoxin-modified
doxorubicine-loaded liposomes. J Control Release. 152:402–410.
2011. View Article : Google Scholar : PubMed/NCBI
|