Introduction
Hamartomas of the breast, also known as
fibroadenolipomas, lipofibroadenomas or adenolipomas, are benign
lesions that were first described in 1971 (1). Hamartomas account for between 0.04 and
1.15% of all benign breast tumors in females (2,3). Myoid
hamartoma of the breast is composed of differentiated mammary
glandular and stromal structures and is considered to be a rare
variant of mammary hamartoma. Myoid hamartomas may present as
painless breast lumps, using sonography it has been revealed that
the majority of hamartomas are hyperechoic or composed of mixed
echogenicity, retrotumor acoustic phenomena are absent. Breast
hamartomas are rare lesions, that may be misdiagnosed
pre-operatively, with a definitive diagnosis made by histological
examination. As a hamartoma has the potential to progress to breast
cancer (3–10), surgical removal is the curative
treatment for breast hamartomas (11,12).
The patient provided written informed consent.
Case report
A 44-year-old female was admitted to the Changhua
Christian Hospital, LuKang branch Hospital, Outpatient Department
(Changhua, Taiwan) on March 12, 2014 with a mass in the left breast
that had been apparent for four months. A physical examination
revealed the presence of a mass measuring ~3 cm in diameter in the
upper outer quadrant (UOQ) of the left breast. The presence of a
contralateral mass or axillary lymphadenopathy was not evident.
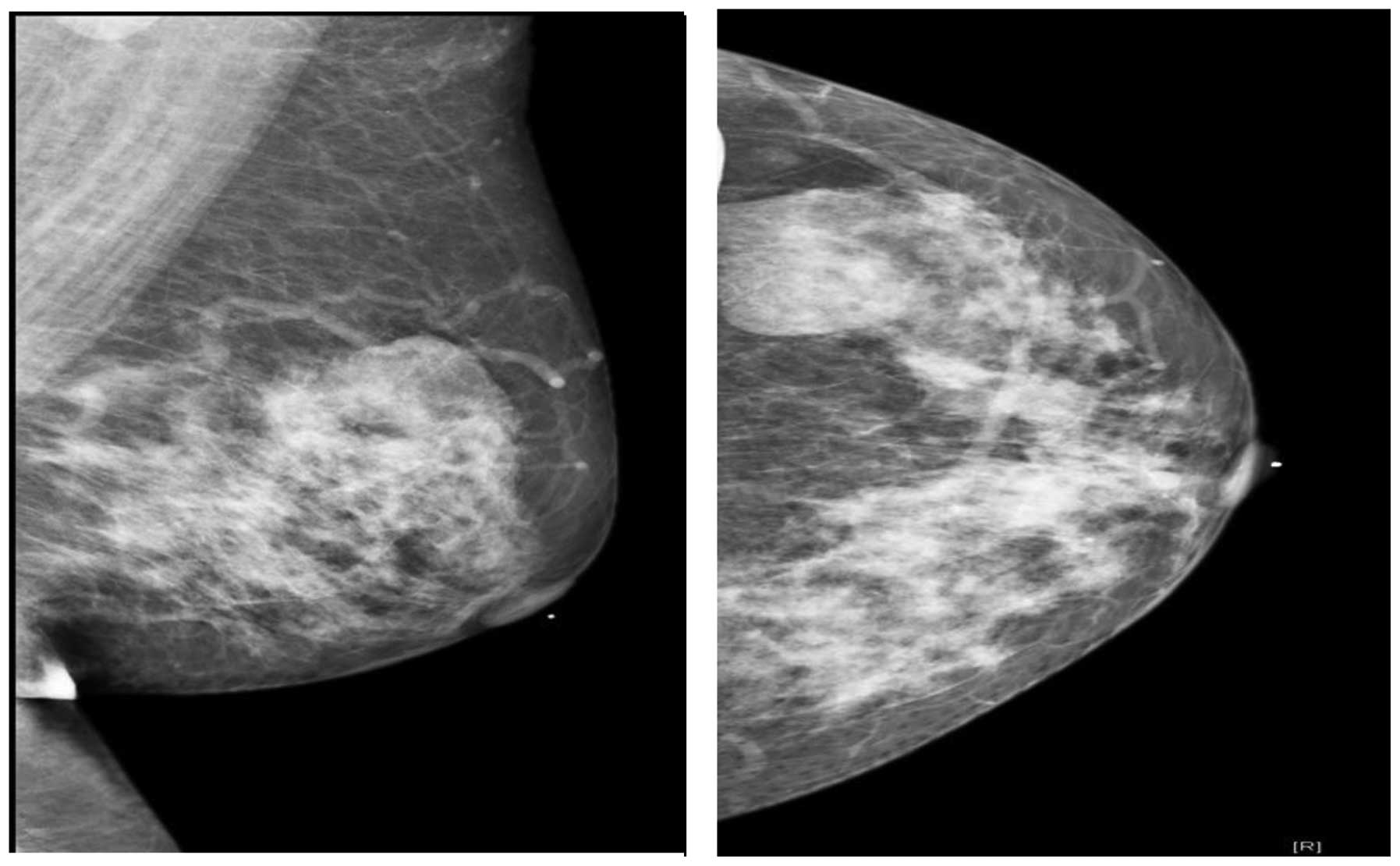
Mammographical examinations performed to rule out malignancy
revealed a lobulated partial indistinct isodense mass measuring
~3.8 cm in the UOQ of the left breast (Fig. 1) and suggested that further
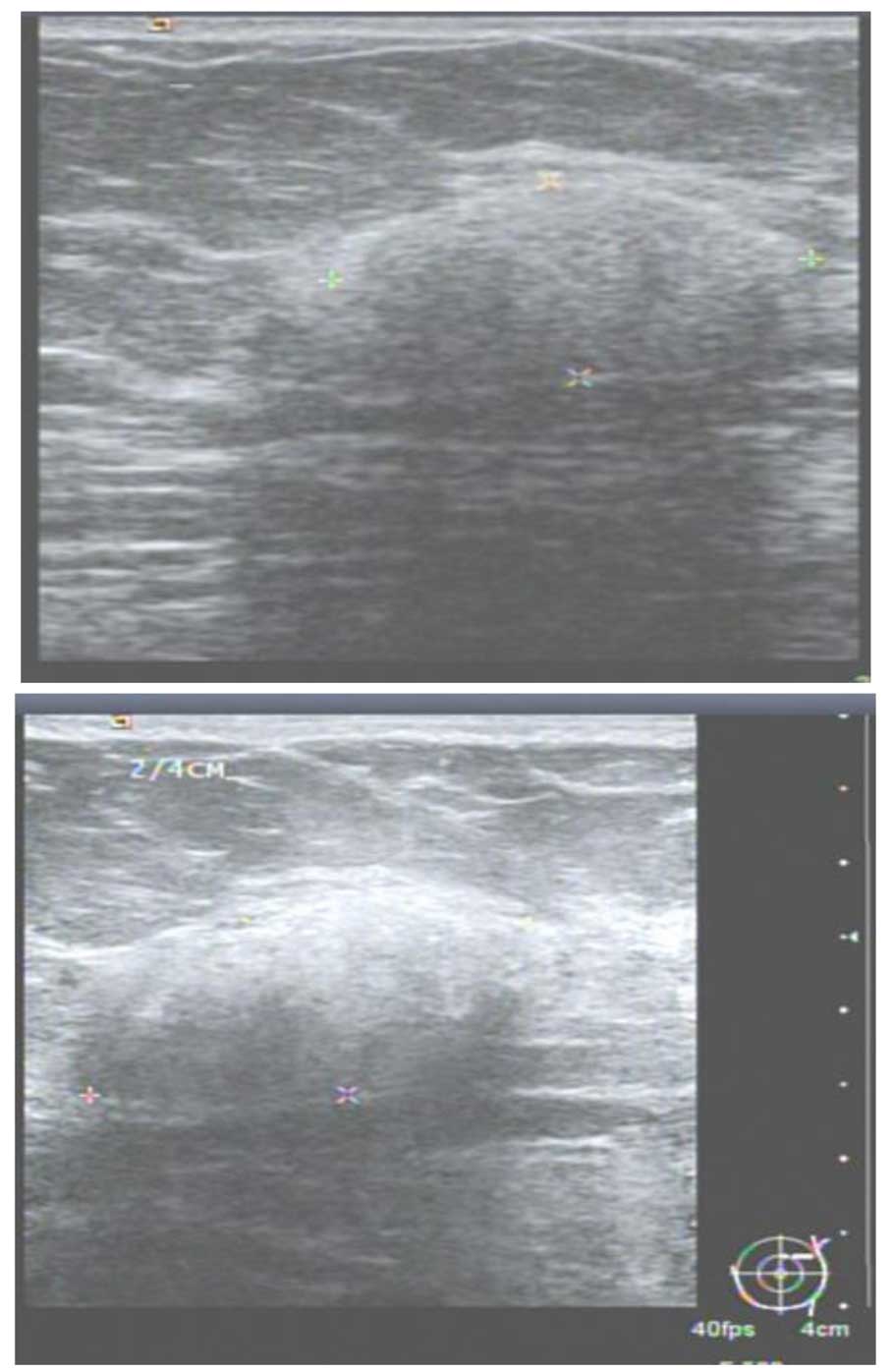
evaluation and tissue examinations were necessary. Ultrasonography
examinations revealed a ~2.42×2.17×1.36 cm mass in the left breast,
which was fairly well-circumscribed and demonstrated complex
scattered echogenic areas and isoechoic tissue, which was
consistent with a diagnosis of lipoma (Fig. 2). Due to the presence of
heterogeneous echo dense areas, an ultrasound-guided core needle
biopsy was recommended for further assessment. The core needle
biopsy revealed fibrocystic changes with small focal duct
aggregations. Immunohistochemically, intact myoepithelial cells
were identified using p63 staining. A diagnosis of focal adenosis
was considered. As malignancy could not be excluded, an excisional
biopsy was performed using a circumareolar incision. The excised
specimen, which consisted of a tissue fragment measuring
5.5×3.4×2.5 cm, was fixed in formalin. Grossly, the tissue appeared
tan-white in color and elastic. Upon dissection, a whitish nodule
measuring 1.7×1.5 cm was identified. Microscopically, a
well-circumscribed tumor measuring 1.9×1.8 cm was identified, which
was primarily composed of fibrous stroma, spindle cells, abundant
fat cells and scatted mammary ductolobular units in the center or
periphery of the tumor. Pseudoangiomatous stromal hyperplasia was
also evident in the tumor region. Immunostaining revealed that the
spindle cells were p63(−), cluster of differentiation 34(+) and
desmin(+). Focal microcalcification was also apparent inside the
ducts and lobules. Consequently, a diagnosis of myoid hamartoma
with focal chondromyxoid differentiation and pseudoangiomatous
stromal hyperplasia was established (Figs. 3 and 4). The patient exhibited no post-operative
complications during the Outpatient Department follow-up and no
further treatment was necessary.
Discussion
Myoid hamartomas may present as painless breast
lumps that can be misdiagnosed pre-operatively. It is well
documented that the internal echo texture of the majority of
hamartomas is hyperechoic or composed of mixed echogenicity.
Retrotumor acoustic phenomena are absent in the majority of
hamartomas (13), however, the
phenomena were present in the patient in the present study(Fig. 2). Breast hamartomas are
well-circumscribed, solid, oval tumors without intratumor
microcalcification. In cases where a benign breast lesion is
encountered with microcalcifications, coexistent malignancy should
be ruled out (14). The patient in
the present study presented with a breast tumor with focal
microcalcification inside the ducts and lobules, but with the
absence of any malignancy. Breast hamartomas are rare lesions, with
a definitive diagnosis made by histological examination. The use of
excisional biopsies and immunohistochemical analyses are important
in order to avoid confusion during the diagnosis of benign and
malignant spindle cell tumors (15,16).
It is well documented that the use of fine-needle aspiration
cytology and needle biopsy is unlikely to provide sufficient
evidence for pathologists (17). In
the present study, a core needle biopsy of the breast tumor
revealed fibrocystic changes with small focal duct aggregations, in
agreement with the literature (17). Although hamartomas are benign,
coincidental malignancy may occur. Therefore, surgical removal is
the curative treatment for breast hamartomas (11,12).
The patient in the present study underwent a partial mastectomy in
order to achieve a tumor-free margin. The pathological report
established a diagnosis of myoid hamartoma with focal chondromyxoid
differentiation and pseudoangiomatous stromal hyperplasia, which is
an exceptionally rare breast lesion. Post-operative complications
were not observed during the Outpatient Department follow-up.
References
|
1
|
Arrigoni MG, Dockerty MB and Judd ES: The
identification and treatment of mammary hamartoma. Surg Gynecol
Obstet. 133:577–582. 1971.PubMed/NCBI
|
|
2
|
Hessler C, Schnyder P and Ozello L:
Hamartoma of the breast: diagnostic observation of 16 cases.
Radiology. 126:95–98. 1978. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee EH, Wylie EJ, Bourke AG and Bastiaan
De Boer W: Invasive ductal carcinoma arising in a breast hamartoma:
two case reports and a review of the literature. Clin Radiol.
58:80–83. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schrager CA, Schneider D, Gruener AC, Tsou
HC and Peacocke M: Clinical and pathological features of breast
disease in Cowden’s syndrome: an underrecognized syndrome with an
increased risk of breast cancer. Hum Pathol. 29:47–53. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mester J, Simmons RM, Vazquez MF and
Rosenblatt R: In situ and infiltrating ductal carcinoma arising in
a breast hamartoma. AJR Am J Roentgenol. 175:64–66. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tse GM, Law BK, Pang LM and Cheung HS:
Ductal carcinoma in situ arising in mammary hamartoma. J Clin
Pathol. 55:541–542. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Baron M, Ladonne JM, Gravier A, Picquenot
JM and Berry M: Invasive lobular carcinoma in a breast hamartoma.
Breast J. 9:246–248. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ruiz-Tovar J, Reguero-Callejas ME, Aláez
AB, et al: Infiltrating ductal carcinoma and ductal carcinoma in
situ associated with mammary hamartoma. Breast J. 12:368–370. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scally N, Campbell W, Hall S, McCusker G
and Stirling WJ: Invasive ductal carcinoma arising within a breast
hamartoma. Ir J Med Sci. 180:767–768. 2011. View Article : Google Scholar
|
|
10
|
Kai M, Tada K, Tamura M, et al: Breast
cancer associated with mammary hamartoma. Breast Cancer.
19:183–186. 2012. View Article : Google Scholar
|
|
11
|
Barbaros U, Deveci U, Erbil Y and Budak D:
Breast hamartoma: a case report. Acta Chir Belg. 105:658–659.
2005.
|
|
12
|
Guray M and Sahin AA: Benign breast
diseases: classification, diagnosis and management. Oncologist.
11:435–449. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chao TC, Chao HH and Chen MF: Sonographic
features of breast hamartomas. J Ultrasound Med. 26:447–452.
2007.PubMed/NCBI
|
|
14
|
Al-Sindi Khalid: Myoid hamartoma: An
exceptionally rare breast lesion. Bahrain Med Bull. 30:1–4.
2008.
|
|
15
|
Mizuta N, Sakaguchi K, Mizuta M, et al:
Myoid hamartoma of the breast that proved difficult to diagnose: a
case report. World J Surg Oncol. 10:122012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Khoo JJ, Alwi RI and Abd-Rahman I: Myoid
hamartoma of breast with chondroid metaplasia: a case report.
Malays J Pathol. 31:77–80. 2009.PubMed/NCBI
|
|
17
|
Tse GM, Law BK, Ma TK, Chan AB, Pang LM,
Chu WC and Cheung HS: Hamartoma of the breast: a
clinicopathological review. J Clin Pathol. 55:951–954. 2002.
View Article : Google Scholar : PubMed/NCBI
|