Introduction
Pyriform sinus carcinoma is one type of
hypopharyngeal carcinoma. Early diagnosis of the disease is
difficult, and lymph node metastasis can be observed in a number of
patients (1). Therefore, lymph node
status is one of the most important prognostic factors in pyriform
sinus carcinoma (1). To date, neck
lymph node dissection has been the standard procedure for lymph
node metastasis (2). Although
surgical dissection is an efficient therapeutic tool, it is
accompanied by complications, including limitation of shoulder
movement and lymph edema (2). In
addition, some patients with pyriform sinus carcinoma have
histopathologically negative neck lymph nodes. Thus, early
diagnosis of the neck lymphatic metastasis in hypopharyngeal
carcinomas has predominant value (3,4).
During the past several years, this field gained increasing focus.
B ultrasound, computed tomography (CT), magnetic resonance imaging
and positron emission tomography remain the main methods. All the
above methods demonstrate size rather than architecture, but it is
occasionally not possible to discriminate whether lymphatic
metastasis would happen when the lymph node is a normal size. The
sentinel lymph node mapping is another method of early diagnosis
(5). The most commonly used are the
local injection of dye, lymphoscintigraphy imaging (5) and lymph node biopsy (6), but there are shortcomings. Thus, a new
imaging technique that allows accurate preoperative assessment of
the neck lymph nodes would be important. However, lymphography (LG)
has the unique capability of demonstrating internal architectural
derangements within normal-sized lymph nodes (7). The thin-walled and fenestrated
lymphatic microvessel is easily penetrated by particulate and
macromolecular agents following injection into the extracellular
space. Once inside the vessel, materials that are transported with
the lymph either specifically target certain nodal elements (e.g.
neoplastic cells) or become cleared by macrophages located in the
lymph nodes. According to this theory, interstitial delivery of
diagnostic agents has been of benefit in determining the regional
spread of cancer and assessing lymphatic function either by
indirect CT-LG or indirect magnetic resonance imaging LG (8). This study focuses on indirect CT-LG
used to identify lymph node metastasis in rabbit pyriform sinus VX2
carcinoma.
Materials and methods
Preparation of VX2 tumor mass
suspension
The tumor cells (The First People’s Hospital of
Shanghai Jiao Tong University, Shanghai, China) have been
continuously passed intramuscularly in rabbits. Rabbits were
anesthetized with 60 mg/kg ketamine (Jiangsu HengRui Medicine Co.,
Ltd., Nanjing, China) and 15 mg/kg pentobarbital sodium (Jiangsu
HengRui Medicine Co., Ltd.) and the tumor cells were then implanted
into the thigh muscle. Subsequent to the tumor growing to a
palpable size, the rabbit was sacrificed using an intravenous
overdose of pentobarbital (Jiangsu HengRui Medicine Co., Ltd.). The
tumor was then excised. Muscle and necrotic tissue were removed.
The tumor was placed in a petri dish with saline (Baxter Healthcare
(Shanghai) Co., Ltd., Shanghai, China). Four 1-cm3
pieces were selected and cut with eye scissors into pieces ≤1
mm3. These pieces were then put into another dish with
40 ml balanced saline and suspended at 100 pieces/ml.
Animal model
Fifteen New Zealand white rabbits, weighing 2.0–3.0
kg, were provided and bred by the Laboratory Animal Center of the
Eye, Ear, Nose and Throat Hospital (Shanghai, China) under routine
conditions according to the institute’s ethical and environmental
guidelines. The rabbits were randomly divided into three groups,
each containing five rabbits. Tumor implantations were performed
under general anesthesia. The rabbits were premedicated with 60
mg/kg of 5% ketamine injected intramuscularly. After 5 min, a
‘butterfly’ needle (Shanghai Medical Instruments Co., Ltd.,
Shanghai, China) was inserted into the marginal vein of the ear,
and 15 mg/kg pentobarbital sodium was injected slowly. Animals
breathed without the aid of a respirator. Anesthesia was maintained
≤30 min with good analgesia and muscle relaxation.
Anesthetized rabbits were placed in a supine
position on a specifically designed operation table (Eye, Ear, Nose
and Throat Hospital) which allowed for the extension of the neck. A
pediatric direct laryngoscope (Shanghai Medical Instruments Co.,
Ltd.) was used to expose the pyriform sinus. The VX2 mass
suspension was drawn up into a 1-ml syringe (Jiangsu Zhengkang
Medical Apparatus Co., Ltd., Changzhou, China) with a
retropharyngeal puncture needle (1.2 mm diameter; Shanghai Medical
Instruments Co., Ltd.) and 0.5 ml was injected into the submucosa
of the lateral wall of the pyriform sinus. Injection into the site
was confirmed by the visualization of a small mucosal bleb. The
rabbits underwent a CT scan on days 14 (group 1), 21 (group 2), and
28 (group 3).
CT
A CT scan was performed using a multi-detector raw
CT scanner (SOMATOM Sensation 10, Siemens Healthcare, Shanghai,
China). A CT scan was administered to each group. Each anesthetized
animal was placed in the supine position on the CT table and
tightly fixed with cotton tape, extending their neck. The CT
scanning was operated at 120 kV, 150 mA, a 7–12 cm field of view,
512–512 matrix, with a detector of a 0.75 mm -10 rows, section
spacing of 3 mm and table speed of 5.6 mm/r. The number of sections
was individually adapted to ensure coverage of the anterior neck
region.
Plain scan and venous enhancement with Omnipaque™
(GE Healthcare Inc., Princeton, NJ, USA)were conducted prior to
indirect LG. Subsequently, 0.5 ml of Omnipaque™ was injected into
the submucosa of the pyriform sinus bilaterally under the direct
laryngoscope. The contiguous 3 mm-thick transaxial CT images from
the submandibular regions to the supra-sternum regions were
obtained immediately, in addition to successively at 1, 3, 5, 10
and 15 min after injection.
Image analysis
One surgeon and one experienced radiologist analyzed
the image data. The images were randomly viewed using a picture
archiving and communication system workstation (PCVDMAPP MFC
Application; Siemens AG Medical Solutions, Erlangen, Germany). The
two doctors were blind to each other’s radiological evaluation
results and to the histopathologic results. In cases of
discrepancies between the two authors, a consensus was reached
through discussion.
Histological evaluation
Rabbits were scarified on days 14 (group 1), 21
(group 2) and 28 (group 3) after CT scanning. Prior to
scarification, methylene blue (Southwest Synthetic Pharmaceutical
Co., Ltd., Chongqing, China) mixed with Omnipaque™ was injected
into the submucosa of the pyriform sinus bilaterally under the
direct laryngoscope. Subsequently, a complete cervical lymph node
dissection was performed and the pyriform sinus was observed and
excised. The location and size of the resected lymph nodes were
recorded for all rabbits. The blue-stained nodes were placed into
the specimen bottle and subjected to a CT scan. The resected lymph
nodes and pyriform sinus tumor were then fixed in 10% formalin
(Hubei Xinfei Chemical Co.Ltd, Wuhan, Hubei, China)in saline for
≥24 h. Sections were stained with hematoxylin and eosin (Beyotime
Biotechnology (Shanghai) Co., Ltd, Shanghai, China).
Statistical analysis
SPSS 11.5 software (SPSS, Inc., Chicago, IL, USA)
was used for data analysis. The average diameter of lymph nodes
between the CT and histological evaluation was compared by the way
of paired-sample t-test. A significance level of α=0.05 was
used.
Results
CT study
All the rabbits taken from the three groups were
scanned by CT. Eight tumors were found in the left hemisphere while
seven tumors were found in the right. In group 1, soft tissue
images could be observed in the implanted side, and the pyriform
sinus disappeared. However, paraglottic space invasion could also
be observed. In group 2, images of thyroid cartilage destruction
and outside invasion of tumors could be observed. In group 3, the
tumors could be observed adhering to adjacent nodes.
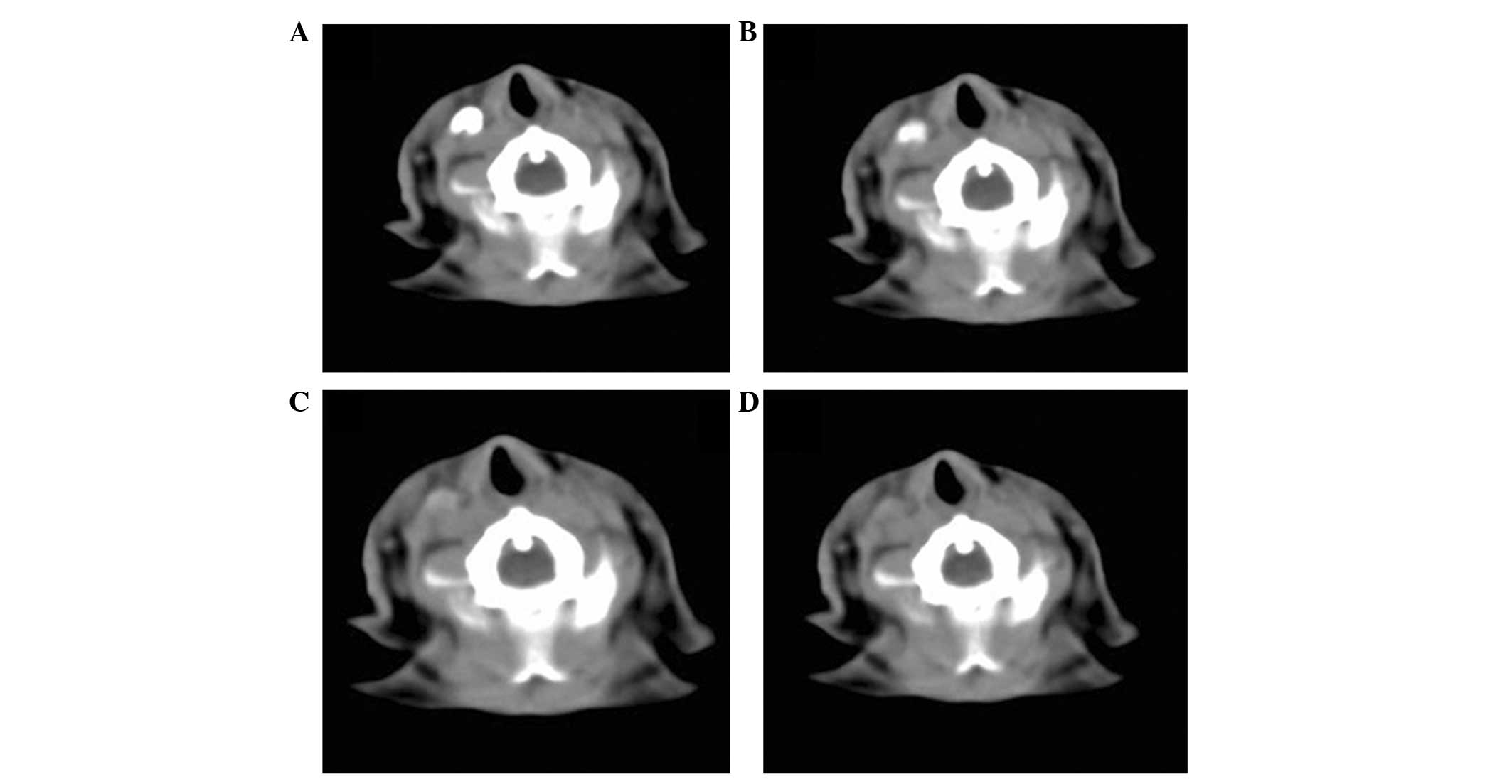
On plain CT images, cervical lymph nodes were not
clearly identified in all the rabbits (Fig. 1A). This also occurred in the venous
enhancement with a slightly high density (Fig. 1B). However, following the injection
of Omnipaque™ into the submucosa of the pyriform sinus bilaterally,
the deep cervical lymph nodes were rapidly enhanced in each rabbit.
However, the submandibular cervical lymph nodes remained
unrevealed. Ipsilateral deep lymph node metastasis was observed in
100% of animals in all the groups, and contralateral metastasis
occurred at rates of 80% on day 14, 60% on day 21, and 100% on day
28. There was one oval-shaped enhanced lymph node which was located
lateral to the larynx and cricoid cartilage, below the
sterno-thyroid muscle. The contrast agent filling defected appeared
on the metastasis nodes while the lymph node without metastasis was
smooth (Fig. 1C). Time points of 1
and 3 mins after injection exhibited the highest CT attenuation,
ranging at 400–600 HU. The CT attenuation generally decreased from
5 min with a range of 200–400 HU, to 50–100 HU at 10 min and <50
HU at 15 min (Fig. 2A–D).
Three-dimensional (3D) CT images were reconstructed from the CT-LG
images at each time point. The oval-shaped lymph nodes with greater
diameters than those of the lymphatic vessels were easily
identified (Fig. 1D). Thus it
effectively displayed the vessels from the submucosa of the
pyriform sinus directed to each node located in the para-laryngeal
areas. Unsmoothed surfaces in the metastasis nodes were easily
observed.
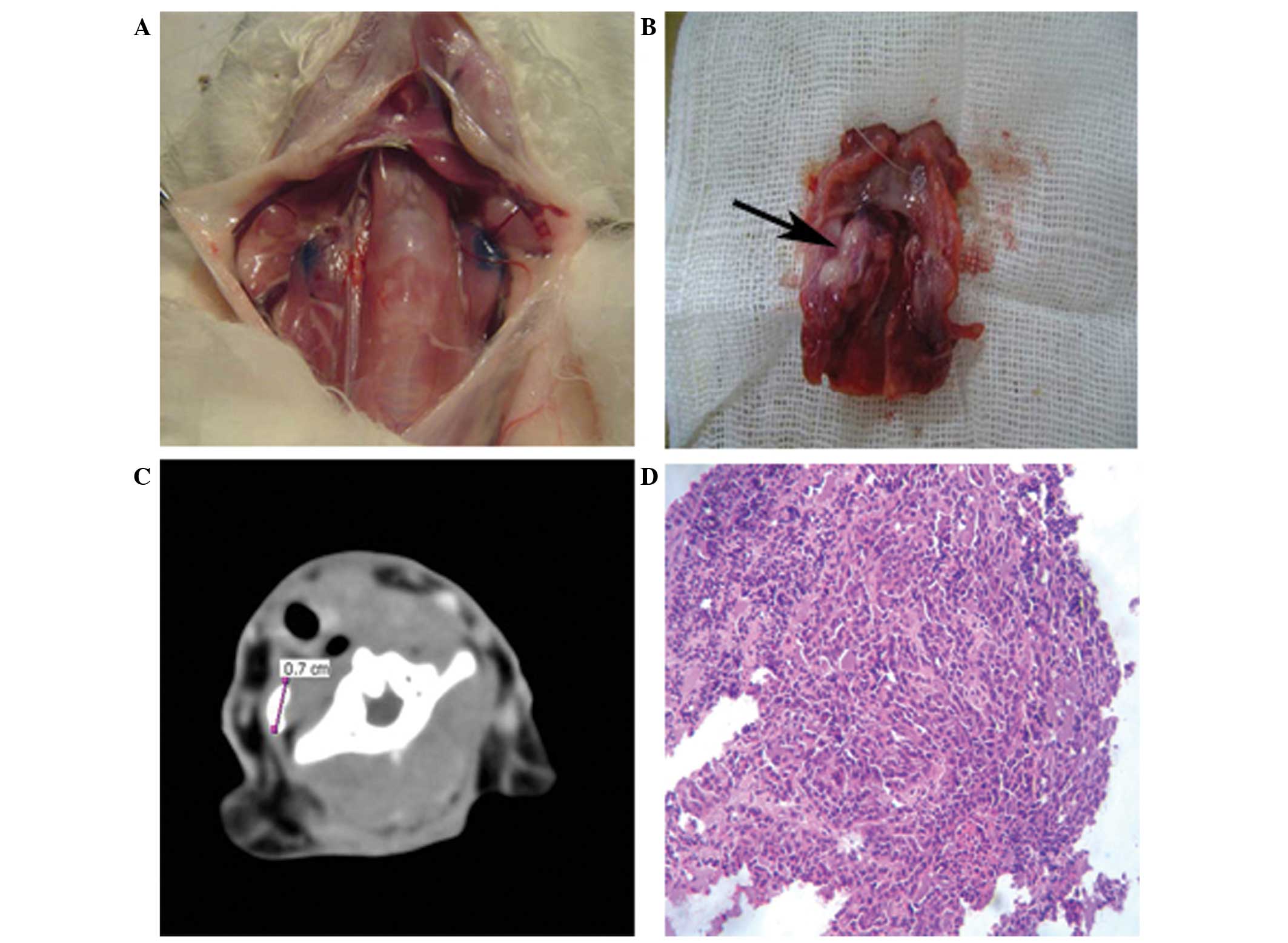
Gross appearance and histology
Deep cervical lymph nodes were located laterally,
with 1–2 oval lymph nodes per side, into the larynx and cricoid
cartilage below the sterno-thyroid muscle. However, the blue-stain
nodes were only one for each side (Fig.
3A). Following a subsequent CT scan, the nodes were observed to
be enhanced. The other two groups of nodes, including the
para-tracheal and sub-mandibular lymph nodes, could not be observed
with the blue-stain. The occurrence of the ipsilaterally located
deep lymph node metastases was observed in 100% of the animals in
all the groups. Contralateral metastasis rates were 80% on day 14,
60% on day 21 and 100% on day 28 (Table
I). It was in accordance with the CT image. The median diameter
of the nodes on the CT images was 0.533±0.056 cm, while 0.541±0.066
cm by the histological method. No significant differences were
found between histology and CT scanning (Fig. 3C).
 | Table INumber of lymph nodes at different
times following computed tomography (CT) lymphography. |
Table I
Number of lymph nodes at different
times following computed tomography (CT) lymphography.
| | Deep cervical lymph
nodes | Filling defected | Smoothed |
|---|
| |
|
|
|
|---|
| Group | n | Ipsilateral | Contralateral | Ipsilateral | Contralateral | Ipsilateral | Contralateral |
|---|
| 1 | 5 | 5 | 5 | 5 | 4 | 0 | 1 |
| 2 | 5 | 5 | 5 | 5 | 3 | 0 | 2 |
| 3 | 5 | 5 | 5 | 5 | 5 | 0 | 0 |
Tumors were visible in the pyriform sinus at the
primary site (Fig. 3B). Eight
tumors were placed on the left side, while seven were inoculated at
the right side. Although all tumors were implanted submucosally,
five rabbits in group 1 still showed surface ulceration and
paraglottic space invasion. In group 2, we found thyroid cartilage
destruction and invasion of the tumor outside of the sinus. On day
28, the tumors were found to adhere to adjacent nodes. However, the
medial wall and contralateral pyriform sinus were not invaded.
Since it was difficult to discriminate the tumor from its
surrounding tissues, the present study did not statistically
analyze the diameters of the tumors. Microscopically, the tumors
were poorly differentiated squamous cell carcinoma and invaded the
pyriform sinus, with some showing multi-focal necrosis (Fig. 3D).
Discussion
Three types of CT scan method were used in this
study, which were scanning without contrast agent, venous contrast
and CT-LG. On plain CT images, cervical lymph nodes were not
clearly identified in all rabbits. This also occurred in the venous
enhancement, even for the lymph nodes >1 cm. This may be due to
the contrast agent through the blood circulation, with components
of the metabolic loss. By diffusion into the lymphatic system, its
concentration is lower in the lymphatic system than in the blood.
However, deep cervical lymph nodes were clearly enhanced with
CT-LG. This phenomenon reflects the advantages of indirect LG. The
contrast agent filling defected could be observed on metastasis
nodes. The vessels directing from tumors to lymph nodes were
developed on 3D images. This can provide information on the
internal structure and drainage of lymph nodes.
In addition, indirect CT-LG can be used to identify
sentinel lymph nodes. Torchia et al (9) reported the detection of sentinel lymph
nodes of pig tongue carcinomas. In the present study, a rabbit
animal model was used. Since the distribution of rabbit cervical
lymph nodes is similar to that of humans (10), this is a good model for lymph node
metastasis research. In the rabbit model of auricular and tongue
VX2 carcinoma, the sentinel lymph nodes are same as the parotid
lymph nodes (11,12). Our previous study indicated that
pyriform sinus carcinoma metastasizes primarily in the deep
cervical lymph nodes (13). By
analysis of the CT-LG image, it was revealed that superficial
cervical lymph nodes still could not be revealed. This also
occurred in the histological evaluation with methylene blue
injection. The deep cervical lymph nodes were the first group of
lymph nodes to develop metastases. According to this, deep cervical
lymph nodes could be concluded as the sentinel lymph nodes of
pyriform sinus carcinoma. This was in accordance with our former
study, and also with the viewpoint of the study by Dunne et
al (10).
Furthermore, the present study revealed that the
numbers of the lymph nodes identified on the CT scan were quite
different from those identified by histology. This may be due to
the contrast agent concentration and infusion rate in the second
leg of the lymph nodes not achieving the imaging requirements. This
phenomenon can be attributed to the nature of the contrast agent.
The present study used the water soluble non-ionic contrast agent
Omnipaque™, which exhibited a shorter reaction time. The peak
appeared immediately following injection (1 and 3 min), and at 5
min began to disappear. This finding is consistent with the study
by Suga et al (14).
Contrast agent combined with lymphatic system carrier could be used
to extend developing time due to its larger molecular weight
(15). Therefore, more focus should
be given to studies on developing contrast agents, as this may
result in improved use of indirect LG. This study presents the
preliminary experience of indirect CT-LG in rabbit pyriform sinus
carcinoma, which may be valuable to further clinical studies.
Acknowledgements
The authors thank Dr Guixiang Zhang from the First
People’s Hospital of Shanghai Jiao Tong University for providing
the VX2 carcinoma tissue, as well as Dr Jian Wang for analyzing the
images. The project was supported by the National Natural Science
Foundation of China (no. 81001201), Health Bureau of New Pudong
District, Shanghai, China (no. PW2012D-4) and Shanghai Municipal
Education Commission, China (no. 13ZZ008).
References
|
1
|
Li XM, Di B, Shao YL, et al: Clinical
pathology feature and prognostic factors of cervical lymph node
metastases in hypopharyngeal carcinoma. Chin J Otorhinolaryngol.
39:741–745. 2004.
|
|
2
|
Tu GY, Xu ZG and Liu SY: Cervical lymph
node metastasis of cancer: from whole neck dissection to minimally
invasive surgery. Zhonghua Zhong Liu Za Zhi. 33:715–717. 2011.
|
|
3
|
Gourin CG and Terris DJ: Carcinoma of the
hypopharynx. Surg Oncol Clin N Am. 13:81–98. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Buckley JG and MacLennan K: Cervical node
metastases in laryngeal and hypopharyngeal cancer: a prospective
ananlysis of prevalence and distribution. Head Neck. 22:380–385.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cheng Y, Wang BQ, Li SJ, et al: A
comparative study of sentinel lymph node detection in laryngeal and
hypopharyngeal carcinoma by lymphoscintigraphy method and blue dye.
Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 45:42–46. 2010.(In
Chinese). PubMed/NCBI
|
|
6
|
Yoshimoto S, Hasegawa Y, Matsuzuka T, et
al: Sentinel node biopsy for oral and laryngopharyngeal squamous
cell carcinoma: a retrospective study of 177 patients in Japan.
Auris Nasus Larynx. 39:65–70. 2012. View Article : Google Scholar
|
|
7
|
Guermazi A, Brice P, Hennequin C, et al:
Lymphography: an old technique retains its usefulness.
Radiographics. 23:1541–1558. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Moghimi SM and Bonnemain B: Subcutaneous
and intravenous delivery of diagnostic agents to the lymphatic
system: applications in lymphoscintigraphy and indirect
lymphography. Advanced Drug Delivery Review. 37:295–312. 1999.
View Article : Google Scholar
|
|
9
|
Torchia MG, Nason R, Danzinger R, Lewis JM
and Thliveris JA: Interstitial MR lymphangiography for the
detection of sentinel lymph nodes. J Surg Oncol. 78:151–157. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dunne AA, Plehn S, Schulz S, et al: Lymph
node topography of the head and neck in New Zealand White rabbits.
Lab Anim. 37:37–43. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Taniguchi I, Sakurada A, Murakami G, et
al: Comparative histology of lymph nodes from aged animals and
humans with special reference to the proportional areas of the
nodal cortex and sinus. Ann Anat. 186:337–347. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jefferis AE and Berenbaum MC: The rabbit
VX2 tumor as a model for carcinoma of the tongue and larynx. Acta
Oto-laryngol (Stockh). 108:152–160. 1989. View Article : Google Scholar
|
|
13
|
Shen N, Wu H, Xu X, et al: Cervical lymph
node metastasis model of pyriform sinus carcinoma. ORL J
Otorninolaryngol Relat Spec. 71:129–134. 2009. View Article : Google Scholar
|
|
14
|
Suga K, Ogasawara N, Yuan Y, et al:
Visualization of breast lymphatic pathways with an indirect
computed tomography lymphography using a nonionic monometric
contrast medium iopamidol: preliminary results. Invest Radiol.
38:73–84. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Harika R, Weissleder K, Poss CZ, et al: MR
lymphography with a lymphotropic T1-type, MR contrast
agent-GD-DTPA-PGM. Magn Reson Med. 33:88–92. 1995. View Article : Google Scholar : PubMed/NCBI
|