Introduction
The incidence of penile carcinoma varies between
countries, with the highest morbidity in Africa and lowest in the
USA and Europe (1). The causes of
this variation remain unclear, but appear to be associated with
epidemiological factors and public health conditions. According to
a previous study, the morbidity associated with penile carcinoma is
correlated with poor education, a low income, inhabitance of a
rural region, a history of heavy smoking, chronic inflammation,
genital warts, penile tears, frequent phimosis and poor genital
hygiene habits (1). Penile
carcinoma has been the most common male urogenital malignant tumor
in China since the 1950s (2).
Concurrent with the economic development and the improvement of
sanitary conditions, the incidence of penile carcinoma has reduced
gradually in China, with a current morbidity rate similar to that
of western countries. Penile carcinoma accounts for ≤0.5% of all
male carcinoma cases in Europe and the USA, the majority of which
are squamous cell carcinomas (SCCs) (3). The most common type of SCC of the
penis is conventional SCC, accounting for 48–65% of cases, followed
by basaloid carcinoma, accounting for 4–10% of cases, warty
carcinoma, which accounts for 7–10% of cases and verrucous
carcinoma, which accounts for 3–8% of cases (1).
Penile verrucous carcinoma, a variant of
well-differentiated SCC, is characterized by slow growth and a
locally aggressive nature, but it rarely metastasizes to regional
nodes or distant regions (4,5). This
carcinoma is an extremely rare disease and is not well
characterized (6). The etiology,
diagnosis and treatment of penile verrucous carcinoma remain poorly
understood, particularly in the Chinese population. At present, the
mainstay for treatment of penile verrucous carcinoma continues to
be penectomy, which generally leads to psychosexual issues and
markedly diminishes the quality of life. Other therapies include
intra-aortic infusion chemotherapy, which has been demonstrated to
be effective and is considered as an organ-sparing treatment,
particularly for younger patients (4). In the present study, the tissues
obtained by penectomy from 10 cases of penile verrucous carcinoma
were retrospectively analyzed to assess the methods of diagnosis
and treatment of penile verrucous carcinoma in the Chinese
population.
Patients and methods
Patients
In total, 10 cases of penile verrucous carcinoma
treated at the Zhejiang Cancer Hospital (Hangzhou, Zhejiang, China)
were retrospectively analyzed. The patients were diagnosed and
treated in the hospital between December 1999 and December 2009.
The age of the patients ranged between 35 and 72 years old, with a
mean age of 51.5 years. Eight of the patients noticed a penile mass
and the other two were found to possess a neoplasm on the glans
penis when they underwent circumcision. All patients presented with
redundant prepuce or phimosis. The tumor diameter ranged between
0.8 and 4 cm. All tumors exhibited exophytic growth that appeared
cauliflower-like. The lesions involved the entoplastron of the
prepuce in six patients and the glans in four patients. Only one
patient presented with ulcers and local pain due to infection.
Neither inguinal lymph node nor distant metastasis was observed
using chest radiography or ultrasonic examination. All patients
provided written informed consent.
Methods
Diagnosis of penile verrucous carcinoma mainly
relies on biopsy. In the present study, eight patients underwent a
biopsy examination to obtain a definite diagnosis prior to surgery.
One of these patients received a biopsy examination due to
phimosis, but only a small sample of protruding tissue at the
osculum of the prepuce was removed and was pathologically diagnosed
as papilloma. An additional surgical exploration was subsequently
performed on this patient and a tumor with a diameter of ~4 cm
involving the entoplastron of the prepuce was found. Circumcision
was performed again. The histological examination revealed the
lesion to be penile verrucous carcinoma and partial penectomy was
subsequently performed.
One of the remaining two patients underwent
circumcision at Cangan People’s Hospital (Wenzhou, China) due to a
mass in the entoplastron of the prepuce. The histological
examination revealed the lesion to be verrucous carcinoma. Three
months later, a nodule was found in the coronary sulcus of the
penis. Biopsy examination at the Zhejiang Cancer Hospital also
revealed the tumor to be penile verrucous carcinoma and the patient
then underwent a partial penectomy.
The remaining patient had undergone a circumcision
due to phimosis in 1999. During the surgery, a cauliflower-like
neoplasm was found at the dorsal of glans nearing the coronary
sulcus, which was hypothesized to be condyloma acuminatum and was
excised locally. However, the histological examination revealed the
tumor to be squamous metaplasia with partial hyperkeratosis. The
papillomatous tumor recurred and was removed by partial penectomy
in 2002 and in 2004, respectively. The biopsy specimens yielded
similar findings. In 2006, the papillomatous tumor recurred again
and the histological examination revealed the presence of verrucous
carcinoma. Partial penectomy was performed.
All 10 patients received surgical treatment, eight
of which received partial penectomy. This included one patient who
underwent a partial penectomy due to penile verrucous carcinoma
three months after undergoing circumcision for phimosis, and one
patient who underwent several local excisions, as aforementioned,
and then underwent a partial penectomy. No patients received
ilioinguinal lymphadenectomy or chemotherapy.
Results
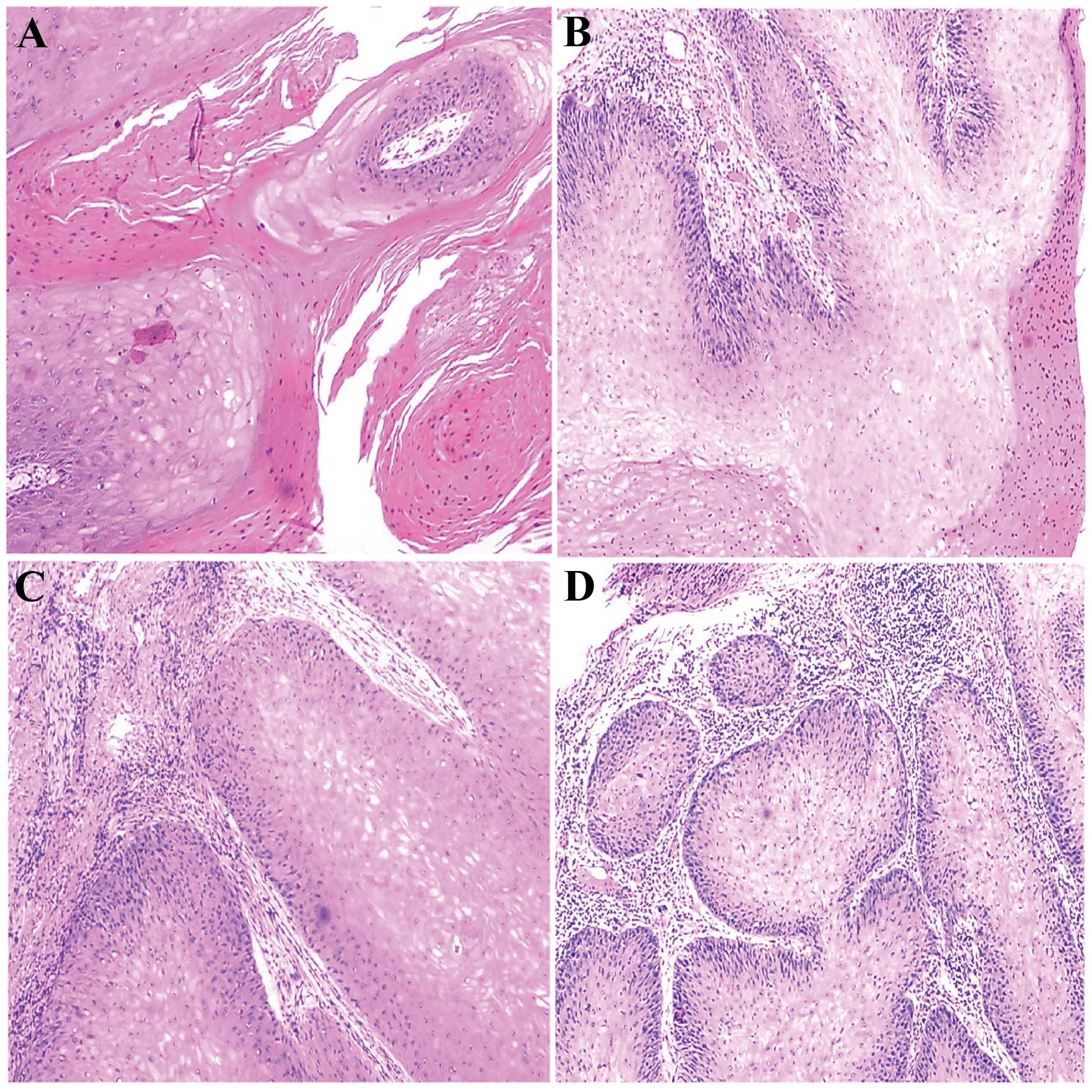
The surgical specimens were histologically examined
at the Department of Pathology (Zhejiang Cancer Hospital). All the
tumors revealed exophytic papillary lesions with a brittle texture
and the incisal surface was gray. Microscopic examination revealed
the tumor to be characterized by papillary growth at the surface
and locally aggressive invasion in the basement membrane of the
tumor. The tumor cells were well-differentiated and exhibited
little heteromorphism, with rare karyokinesis. The epithelium
presented rod-like interdigitation, hyperkeratosis and a
papilloma-like structure (Fig. 1A and
B). The epithelium grew downward into the underlying tissues in
a bulbous or drumstick process. Generally, the tumor exhibited
clear boundaries and rich lymphocytic infiltration in the
surrounding mesenchyme (Fig. 1C and
D). The patients were followed up for 8 months to 9 years. With
the exception of one patient that succumbed unassociated causes,
the patients presented no tumor recurrence or metastasis at the end
of the follow-up.
Discussion
Verrucous carcinoma, which was first described in
1948, has been reported in the oral cavity, anus, penis and female
genitalia (7–10). This carcinoma is an extremely rare
low-grade SCC that exhibits slow invasive growth and a lack of
metastasis, with penile verrucous carcinoma being the most common
type (11).
Penile verrucous carcinoma is a rare disease,
accounting for 2.4–24% of penile cancer (12,13),
which can occur in any part of the penis, but mainly occurs in the
glans penis. Phimosis and redundant prepuce are two important
causative factors for penile verrucous cancer (14,15).
The 10 patients enrolled in the present study all suffered from
phimosis or redundant prepuce, with the most common clinical
manifestation being a local exogenous mass. It is challenging to
identify penile verrucous cancer due to the exterior features
appearing extremely similar to those of condyloma acuminatum.
Penile verrucous carcinoma lesions often present as cauliflower- or
wart-like, and do not cause significant pain. However, verrucous
carcinoma grows slowly, without inhibition, and regions of the
carcinoma can invade the glans or even the shaft. Certain larger
penile verrucous carcinoma tumors possess an unpleasant odor and
result in pain due to necrosis and infection. The penile verrucous
carcinoma tumor cells are well-differentiated and are often
accompanied by squamous epithelial hyperplasia and keratinization.
Thus, verrucous carcinoma may be easily misdiagnosed if an
inappropriate biopsy were to be performed. One patient in the
present study was misdiagnosed with penile papilloma due to the
tissue being inappropriately extracted at the distal end of the
osculum of the prepuce. Therefore, deeper biopsies are recommended,
according to the tumor size, and the basement membrane of the
papillomatous tumor should be particularly considered during the
sampling. For patients that are highly likely to possess verrucous
carcinoma, but have not been diagnosed with the carcinoma, repeated
biopsies should be undertaken. Occasionally, the prepuce may be
opened to obtain suitable tissues if the lesion is accompanied by
phimosis. However, obtaining a diagnosis by histological
examination remains to be challenging if the patient suffers from
giant condyloma acuminatum (11).
Previous studies have indicated that penile
carcinoma is not only associated with human papilloma virus (HPV)
infection, but is also correlated with other factors, including
phimosis, chronic inflammation and lichen sclerosus (12,13).
HPV is considered to be closely associated with penile cancer and
condyloma acuminatum, which is involved in almost all cases of
penile verrucous cancer (16).
However, various types of HPV have been identified. Detection based
on polymerase chain reaction technology identified that the type of
HPV involved in penile verrucous cancer is a high-risk virus with
high carcinogenicity, while the type of HPV is usually low-risk in
condyloma acuminatum. Thus, for giant condyloma acuminatum that is
challenging to identify, identification of the HPV type may aid in
diagnosis (11). Studies have found
that local squamous epithelial hyperplasia and hornification may be
important for the development of penile verrucous carcinoma. In the
present study, nodules recurred four times on the glans penis in
one patient, and the first three histological examinations
identified the tumor as squamous epithelial hyperplasia and
hyperkeratosis, which was consistent with the literature (12,13).
The literature on verrucous carcinoma mostly focuses
on case reports and rarely on large-scale studies. Nevertheless,
surgical treatment for penile verrucous carcinoma has been
generally accepted as the mainstay for treatment. Provided that the
penile verrucous carcinoma is well-differentiated and exhibits good
biological behavior, maximized retention of the appearance and
function of the penis is an accepted surgical principle. Therefore,
a wide range of local and partial resections of the penis are the
most common surgical approaches, and full penectomy is seldom used
in the clinic. However, due to the relatively rare incidence of
penile verrucous carcinoma, surgeons often lack experience, which
leads to the unnecessary removal of part or the entirety of the
penis. If the margin is tumor-positive, the resection should be
extended. Penile verrucous carcinoma exhibits a potential for
recurrence, but the incidence rates vary between studies. If the
carcinoma recurs repeatedly, the patient may require an additional
resection or even full penectomy.
Shimizu et al (17) found that ~30% of verrucous
carcinomas are complicated with micro-lesions of invasive squamous
cell carcinoma, and that certain lesions will eventually progress
to other types of invasive squamous cell carcinoma. A previous
study (18) proposed that urethral
lesions may be an early event in the carcinogenesis of penile
cancer, as they appear on the head of the penis at the early stage
of penile cancer. Patients undergoing local excision should pay
additional attention to the recurrence of the lesion and be
followed-up closely. If any sign of recurrence is observed, the
penis should be further partially resected or totally removed. As
almost no distant metastasis is found in patients with verrucous
carcinoma, inguinal lymphadenectomy is seldom performed.
Previously, inguinal lymphadenectomy was performed
on certain patients, however, no evident lesions were found
(19). Thus, inguinal
lymphadenectomy is not recommended as a prophylactic treatment. As
for patients with localized inguinal lymphadenectasis,
anti-infection treatment may be undertaken initially and, if
necessary, lymph node biopsy may be performed. In the present
study, all 10 patients underwent surgical treatment with the
retention of the penis, but did not undergo lymph node dissection.
With the exception of one patient who succumbed to unassociated
causes, the patients had not experienced recurrence or metastasis
at the end of the follow-up. This study highlighted the clinical
and pathological features of penile verrucous carcinoma and its
treatment. It was found that partial penectomy may result in a good
prognosis and outcome. The study has provided a basis for further
investigation regarding the diagnosis and treatment of penile
verrucous carcinoma.
Acknowledgements
This study was funded by project support from the
Appropriate Technical Transformation of Zhejiang (grant no.
2013ZHB001), and the Outstanding Scientific Research and Talent
Cultivation of Zhejiang Cancer Hospital (grant no. 2012YC004).
References
|
1
|
Chaux A and Cubilla AL: Advances in the
pathology of penile carcinomas. Hum Pathol. 43:771–789. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wu JP: Wu Jieping’s Urology. First
edition. Shandong Science and Technology Press; Jinan, Shandong:
pp. 10132004
|
|
3
|
Mannweiler S, Sygulla S, Winter E and
Regauer S: Two major pathways of penile carcinogenesis: HPV-induced
penile cancers overexpress p16ink4a, HPV-negative cancers
associated with dermatoses express p53, but lack p16ink4a
overexpression. J Am Acad Dermatol. 69:73–81. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sheen MC, Sheu HM, Jang MY, et al:
Advanced penile verrucous carcinoma treated with intra-aortic
infusion chemotherapy. J Urol. 183:1830–1835. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fujimoto N, Nakanishi G, Ushida H, et al:
Penile verrucous carcinoma arising in HPV-negative condylomatous
papules. Eur J Dermatol. 21:436–438. 2011.PubMed/NCBI
|
|
6
|
Stankiewicz E, Kudahetti SC, Prowse DM, et
al: HPV infection and immunochemical detection of cell-cycle
markers in verrucous carcinoma of the penis. Mod Pathol.
22:1160–1168. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ackerman LV: Verrucous carcinoma of the
oral cavity. Surgery. 23:670–678. 1948.PubMed/NCBI
|
|
8
|
Cuesta KH, Palazzo JP and Mittal KR:
Detection of human papillomavirus in verrucous carcinoma from
HIV-seropositive patients. J Cutan Pathol. 25:165–170. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gualco M, Bonin S, Foglia G, et al:
Morphologic and biologic studies on ten cases of verrucous
carcinoma of the vulva supporting the theory of a discrete
clinico-pathologic entity. Int J Gynecol Cancer. 13:317–324. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kraus FT and Perezmesa C: Verrucous
carcinoma. Clinical and pathologic study of 105 cases involving
oral cavity, larynx and genitalia. Cancer. 19:26–38. 1966.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gross G and Pfister H: Role of human
papillomavirus in penile cancer, penile intraepithelial squamous
cell neoplasias and in genital warts. Med Microbiol Immunol.
193:35–44. 2004. View Article : Google Scholar
|
|
12
|
Chaux A and Cubilla AL: The role of human
papillomavirus infection in the pathogenesis of penile squamous
cell carcinomas. Semin Diagn Pathol. 29:67–71. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Velazquez EF, Chaux A and Cubilla AL:
Histologic classification of penile intraepithelial neoplasia.
Semin Diagn Pathol. 29:96–102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen MF, Chen WC, Wu CT, et al:
Contemporary management of penile cancer including surgery and
adjuvant radiotherapy: an experience in Taiwan. World J Urol.
22:60–66. 2004. View Article : Google Scholar
|
|
15
|
Schwartz RA: Verrucous carcinoma of the
skin and mucosa. J Am Acad Dermatol. 32:1–21. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Seixas AL, Ornellas AA, Marota A, et al:
Verrucous carcinoma of the penis: retrospective analysis of 32
cases. J Urol. 152:1476–1479. 1994.PubMed/NCBI
|
|
17
|
Shimizu A, Tamura A and Ishikawa O:
Invasive squamous cell carcinoma arising from verrucous carcinoma.
Recognition of verrucous carcinoma of skin as an in situ carcinoma.
Eur J Dermatol. 16:439–442. 2006.PubMed/NCBI
|
|
18
|
Velazquez EF, Soskin A, Bock A, et al:
Epithelial abnormalities and precancerous lesion of anterior
urethra in patients with penile carcinoma: a report of 89 cases.
Mod Pathol. 18:917–923. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hatzichristou DG, Apostolidis A, Tzortzis
V, et al: Glansectomy: an altemative surgical treatment for
Buschke-Löwenstein tumors of the penis. Urology. 57:966–969. 2001.
View Article : Google Scholar : PubMed/NCBI
|