Introduction
Magnetic resonance cholangiopancreatography (MRCP)
has been widely used for the evaluation of the pancreatobiliary
system. At present, numerous techniques, including
three-dimensional (3D) and two-dimensional (2D) sequences, have
been used in MRCP. Certain studies have compared 2D and 3D MRCP for
the visualization of the pancreatobiliary system (1–12).
However, studies that have compared the use of 2D and 3D MRCP for
the visualization of pancreatic cystic lesions focused solely on
intraductal papillary mucinous neoplasm (IPMN) (5,8). The
two previous studies concluded that image quality of the pancreatic
duct of 3D MRCP was superior to that of 2D MRCP, 3D MRCP identified
the morphological details of IPMN with more confidence compared
with 2D MRCP. In addition, there was no increase in the level of
accuracy in predicting ductal communication of the lesion in 3D
MRCP, and 3D and 2D MRCP performed similarly for predicting benign
and malignant lesions. By contrast, certain case reports have
revealed that serous and mucinous cystadenoma may communicate with
the main pancreatic duct (13–16),
which may impact the choice of treatment strategy. Pancreatic
tumour enucleation has the benefit of minimal tissue trauma to the
pancreas when compared with resectioning the tumour, adn therefore
tumour enucleation is recommended for pancreatic cystic tumours
<2–3 cm with non-adherence to pancreatic main-ducts (17). Therefore, pre-operative imaging
evaluation of pancreatic cystic lesions is important.
In the present study, 2D and 3D MRCP were compared
in terms of the ability to visualize pancreatic cystic lesions,
including additional subtypes to IPMN.
Materials and methods
Patients
Between February 2009 and December 2011, 35
patients, consisting of 12 males and 23 females with an age range
of 24–71 years (mean age, 48.7 years), underwent MRCP as a
pre-operative evaluation. The patients all received a final
diagnosis of pancreatic cystic lesions that was confirmed by
surgery and pathology. The institutional review board of The
Affiliated Suzhou Hospital of Nanjing Medical University (Suzhou,
China) approved the present retrospective study and waived the
requirement for informed consent. The final diagnoses were mucinous
cystadenoma in eight patients, serous cystadenoma in nine, IPMN in
eight patients, comprising four branch-type and four combined-type
IPMNs, pancreatic retention cyst in three patients, pancreatic
pseudocyst in four patients, simple cyst in two patients and cystic
pancreatic splenosis in one patient.
Eight out of 35 patients were examined using only 2D
MRCP, the remaining 27 patients were assessed using 2D and 3D MRCP.
In total, 28 out of 35 patients had been evaluated using surgery or
pathology to determine whether the cystic lesions communicated with
the pancreatic main duct.
MR technique
All MR imaging (MRI) examinations were performed on
a 3.0-T MRI system with a torso phased array multicoil (Signa HDx;
GE Healthcare Life Sciences, Chalfont, UK). There was a fasting
period of at least four hours prior to imaging, and no oral
contrast material or antiperistaltic agents were administered.
An axial T2-weighted single-shot-fast-spin-echo
(SSFSE) sequence was used to localize the biliary and pancreatic
ductal system. The parameters consisted of a repetition time of
1055 msec, echo time of 600 msec, bandwidth of 62.50 Hz, slice
thickness of 6 mm and spacing of 1 mm, with the number of slices
being 21. The MRCP protocol was composed of 2D radial coronal
thick-slab breath-hold SSFSE and 3D respiratory triggering
fast-recovery-fast-spin-echo (FRFSE) using the array spatial
sensitivity encoding technique (ASSET).
The parameters for 2D MRCP were as follows. The
repetition time was 10,000 ms, the echo time was 900 ms, the
bandwidth was 62.50 Hz and the slice thickness was 50 mm, without
spacing and with a matrix size of 352×352, field of view (FOV) of
30 cm, ASSET of 2.00 phase acceleration (PH). The number of radical
slices was 10 and the partial radial spacing was 10°. The radial
direction was clockwise, the breath-hold duration was five short
breath-holds and there was fat saturation. The scan time of one
slab was 1s. The breath-holds were performed at the end of
inspiration, subsequent to two preceding full respirations. The
thick-slab sequences were acquired using a radial loop centered at
the level of biliopancreatic confluence. The first image of the
radial loop was obtained from the posterior border of the right
hepatic lobe.
The parameters for 3D MRCP were as follows. The echo
time was min, the bandwidth was 62.50 Hz, the slice thickness was
1.8 mm and the number of images was 60, with no spacing. The zero
filling interpolation was 2, the matrix size was 320×256, the FOV
was 32 cm and the ASSET was 2.00 PH. The respiratory interval was
1, the trigger point was 30 and the trigger window was 30. There
was an inter-sequence delay of 199 msec, a respiratory rate of
18–20 and there was fat saturation. The data were gathered at the
end-expiratory phase.
Imaging processing and evaluation
All source images were transferred to a workstation
(Advantage Windows 4.3 CT Workstation; GE Healthcare Life
Sciences). Post-processing of the source images obtained with the
respiratory-triggered 3D FRFSE sequence was performed using
multiplanar volume reformation with the maximum intensity
projection. The angle and range of the section thickness were
freely changeable by the assessor to visualize the pancreatobiliary
system.
Two assessors that were blinded to the clinical
history of the patients and the results of the evaluation provided
the other observer, independently reviewed each image on a display
monitor in a random order and evaluated the image quality using a
five-point scale. Image quality was ranked as: 1, poor
(non-interpretable); 2, suboptimal; 3, acceptable (minimal
artifacts); 4, good; and 5, excellent (no artifacts).
The delineation of the head, body and tail of the
pancreatic duct and the pancreatic cystic lesion were also
evaluated using the following grading system: 5, excellent
(complete delineation); 4, good (delineation of ≥90%); 3, fair
(delineation of <90%); 2, poor delineation; and 1, not
visualized.
The diagnostic confidence in whether there was
communication between the cystic lesion and the pancreatic main
duct was assigned on a five-point scale: 1, definitely absent; 2,
possibly absent; 3, indeterminate; 4, probably present; and 5,
definitely present.
Statistical analysis
Statistical analyses were performed using SPSS 15.0
software (SPSS, Inc. Chicago, IL, USA). P<0.05 was considered to
indicate a statistically significant difference. The comparison of
the image quality between 2D and 3D MRCP were performed using the
Mann-Whitney U test. The diagnostic capability of the 2D and 3D
MRCP images for predicting ductal communication of the lesion was
calculated by measuring the area under the receiver operating
characteristic (ROC) curve (Az). Calculation of the statistical
significance of the difference between the Az values for the 2D and
3D MRCP was performed using the Z-test. Analysis of the
inter-observer agreement between the two readers was performed
using the κ statistic.
Results
For each reader, the image quality of 3D MRCP was
judged to be higher compared with 2D MRCP (Table I; Figs.
1 and 2).
 | Table IComparison between 2D MRCP and 3D MRCP
image quality and the identification of the features of the cystic
lesions. |
Table I
Comparison between 2D MRCP and 3D MRCP
image quality and the identification of the features of the cystic
lesions.
| Image quality | Features of the
cystic lesions |
|---|
|
|
|
|---|
| Read 1 | Read 2 | κ | Read 1 | Read 2 | κ |
|---|
| 2D MRCP | 3.51 | 3.49 | 0.508 | 3.26 | 3.31 | 0.696 |
| 3D MRCP | 4.22 | 4.19 | 0.656 | 4.00 | 3.92 | 0.787 |
| P-value | 0.001 | 0.003 | | 0.004 | 0.011 | |
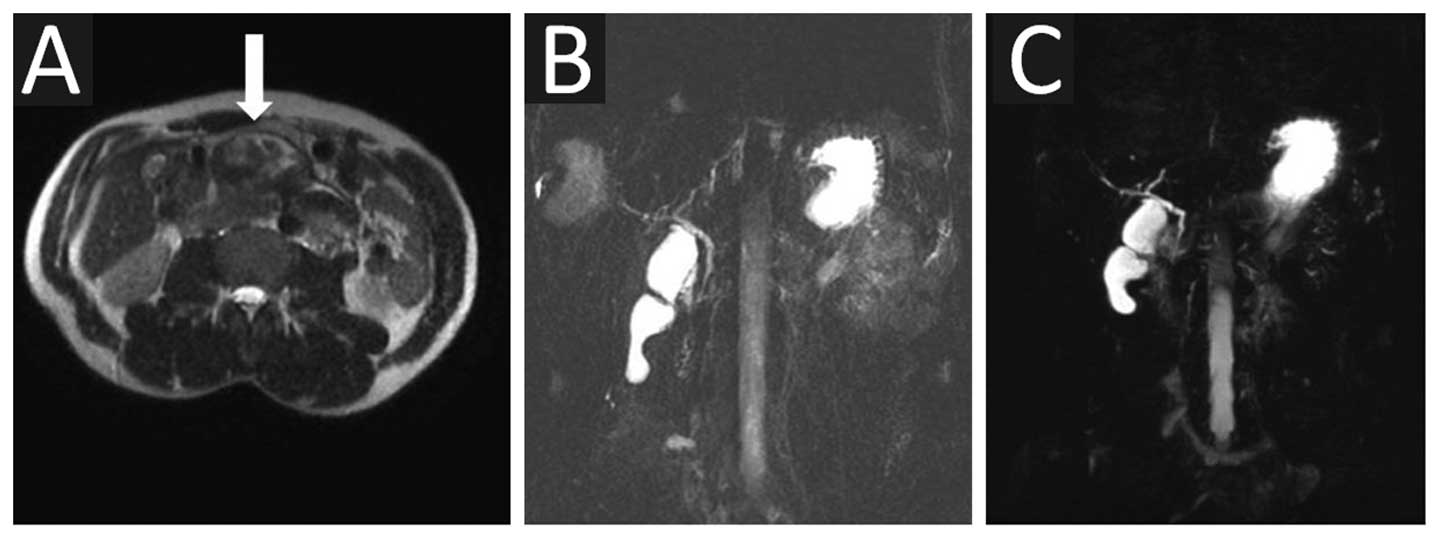
The cystic lesion features were visualized better on
3D MRCP compared with 2D MRCP (Table
I; Figs. 1 and 2), but the cystic lesions were not
visualized on MRCP in two out of eight cases that were examined
using 2D MRCP only. These two lesions comprised one retention cyst
and one pseudocyst. The cystic lesions were not visualized by MRCP
in two out of 27 cases that were examined using 2D and 3D MRCP,
comprising one splenosis and one pseudocyst. These lesions
exhibited the same imaging features on T2-weighted imaging, with
low or mixed-low signal intensity (Fig.
3). The same capability of visualizing the segment of
pancreatic main duct was exhibited by 3D and 2D MRCP (Table II; Fig.
4).
 | Table IIComparision between the visualization
of the pancreatic main duct on 2D MRCP and 3D MRCP. |
Table II
Comparision between the visualization
of the pancreatic main duct on 2D MRCP and 3D MRCP.
| Pancreatic duct
visualization |
|---|
|
|
|---|
| Head | Neck | Tail |
|---|
|
|
|
|
|---|
| Read 1 | Read 2 | κ | Read 1 | Read 2 | κ | Read 1 | Read 2 | κ |
|---|
| 2D MRCP | 3.17 | 3.20 | 0.863 | 3.17 | 3.25 | 0.882 | 3.17 | 3.48 | 0.809 |
| 3D MRCP | 3.37 | 3.26 | 0.848 | 3.17 | 3.19 | 0.713 | 3.11 | 3.33 | 0.806 |
| P-value | 0.210 | 0.660 | | 0.363 | 0.782 | | 0.117 | 0.314 | |
The 2D and 3D MRCP Az values for the prediction of
ductal communication between the cystic lesion and the pancreatic
main duct involved 25 cases for 2D MRCP, due to the exclusion of
seven cases that were not evaluated for communication and three
cases that did not demonstrate cystic lesions on MRCP. The Az value
for 3D MRCP involved 19 cases, due to the exclusion of seven cases
in which the communication was not evaluated and one case in which
MRCP did not reveal the cystic lesion. There was no statistically
significant difference between the prediction of ductal
communication with cystic lesions on 2D and 3D MRCP (Table III and Figs. 1 and 2). There were three cases in which MRCP
led to the erroneous prediction of ductal communication with
lesions, as these lesions were adjacent to the pancreatic main duct
(Fig. 4).
 | Table IIIComparision between the prediction of
communication between the pancreatic main duct and cystic lesion
made based on 2D MRCP and 3D MRCP. |
Table III
Comparision between the prediction of
communication between the pancreatic main duct and cystic lesion
made based on 2D MRCP and 3D MRCP.
| Az value |
|---|
|
|
|---|
| Read 1 | Read 2 | κ |
|---|
| 2D MRCP | 0.863 | 0.858 | 0.585 |
| 3D MRCP | 0.923 | 0.892 | 0.779 |
| P-value | 0.616 | 0.671 | |
Discussion
In comparison with 2D thick-slab MRCP, 3D MRCP using
ASSET exhibits superior image quality and the features of the
cystic lesions are better visualized. The 3D sequence provides the
merits of a high signal to noise ratio and intrinsically contiguous
sections that may be used to reconstruct images in any projection,
which yields the anatomical overview normally provided by
thick-slab 2D MRCP images (4,5,8). The
long acquisition time is the main disadvantage of primary 3D MRCP
compared with the 2D MRCP technique. ASSET, which is applied to
phase-encoded directions, overcomes this disadvantage of 3D MRCP,
as ASSET allows for a higher matrix to be maintained without
prolonging the imaging time (2).
The FRFSE sequence can increase the signal to noise ratio by
refocusing residual transverse magnetization into a final spin echo
and using a −90° fast-recovery pulse to flip back along the z-axis
to increase longitudinal magnetization and create a driven
equilibrium (4).
In the present study, MRCP did not reveal the cystic
lesions in two out of eight cases that were examined using only 2D
MRCP. These lesions comprised one pancreatic retention cyst and one
pseudocyst. By contrast, MRCP did not reveal the cystic lesions in
two out of 27 cases that were examined using 2D and 3D MRCP,
comprising one cystic pancreatic splenosis and one pseudocyst.
These lesions exhibited the same imaging features in that the
T2-weighted imaging demonstrated low or mixed-low signal intensity.
As MRCP typically appears heavy on T2-weighted imaging, the lesion
may be not revealed by MRCP if the lesion exhibits low signal
intensity on the T2-weighted image.
In the present study, 3D MRCP exhibited the same
capability for the visualization of the segment of pancreatic main
duct as 2D MRCP, which is in agreement with the results of the
study by Kim et al (12),
Palmucci et al (3) and
Sodickson et al (4), but
other studies have reported varying results (2,5,18). The
reasons for this may include that the pancreatic duct is sensitive
to respiration (17) and that 2D
MRCP exhibits superior in-plane resolution (4).
Previous studies have revealed that the ability of
2D and 3D MRCP to predict ductal communication with the cystic
lesion does not significantly differ between the two MRCP
techniques, although 3D MRCP exhibits a higher area under the ROC
curve (5,8). In the present study, the 2D and 3D
MRCP Az values for the prediction of communication between cystic
lesions and the pancreatic main duct were not statistically
different, either. Therefore, 3D MRCP requires additional technical
improvement for the visualization of extremely small anatomical
features.
The present study possessed certain limitations.
First, the present study demonstrated a patient selection bias in
that the majority of the studies performed MRCP upon the
identification of indeterminate CT findings. The sample size was
relatively small, and additional studies with an increased number
of cases may be required in the future. In addition, as 2D and 3D
MRCP were not applied together in all cases, the present study is
not a paired analysis.
To conclude, in comparison to 2D MRCP, 3D MRCP
provides an improved assessment of pancreatic cystic lesions.
However, 3D MRCP does not exhibit an improved capability for the
visualization of the pancreatic main duct and prediction of
communication between cystic lesions and the pancreatic main
duct.
References
|
1
|
Cova M, Stacul F, Cester G, et al: MR
cholangiopancreatography: comparison of 2D single-shot fast
spin-echo and 3D fast spin-echo sequences. Radiol Med. 106:178–190.
2003.PubMed/NCBI
|
|
2
|
Masui T, Katayama M, Kobayashi S, et al:
Magnetic resonance cholangiopancreatography: comparison of
respiratory-triggered three-dimensional fast-recovery fast
spin-echo with parallel imaging technique and breath-hold
half-Fourier two-dimensional single-shot fast spin-echo technique.
Radiat Med. 24:202–209. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Palmucci S, Mauro LA, Coppolino M, et al:
Evaluation of the biliary and pancreatic system with 2D SSFSE,
breathhold 3D FRFSE and respiratory-triggered 3D FRFSE sequences.
Radiol Med. 115:467–482. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sodickson A, Mortele KJ, Barish MA, et al:
Three-dimensional fast-recovery fast spin-echo MRCP: comparison
with two-dimensional single-shot fast spin-echo techniques.
Radiology. 238:549–559. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yoon LS, Catalano OA, Fritz S, et al:
Another dimension in magnetic resonance cholangiopancreatography:
comparison of 2- and 3-dimensional magnetic resonance
cholangiopancreatography for the evaluation of intraductal
papillary mucinous neoplasm of the pancreas. J Comput Assist
Tomogr. 33:363–368. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Choi JY, Kim MJ, Lee JM, et al: Magnetic
resonance cholangiography: comparison of two- and three-dimensional
sequences for assessment of malignant biliary obstruction. Eur
Radiol. 18:78–86. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi JY, Lee JM, Lee JY, et al:
Navigator-triggered isotropic three-dimensional magnetic resonance
cholangiopancreatography in the diagnosis of malignant biliary
obstructions: comparison with direct cholangiography. J Magn Reson
Imaging. 27:94–101. 2008. View Article : Google Scholar
|
|
8
|
Choi JY, Lee JM, Lee MW, et al: Magnetic
resonance pancreatography: comparison of two- and three-dimensional
sequences for assessment of intraductal papillary mucinous neoplasm
of the pancreas. Eur Radiol. 19:2163–2170. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Morita S, Ueno E, Suzuki K, et al:
Navigator-triggered prospective acquisition correction (PACE)
technique vs. conventional respiratory-triggered technique for
free-breathing 3D MRCP: an initial prospective comparative study
using healthy volunteers. J Magn Reson Imaging. 28:673–677. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reinhold C, Guibaud L, Genin G and Bret
PM: MR cholangiopancreatography: comparison between two-dimensional
fast spin-echo and three-dimensional gradient-echo pulse sequences.
J Magn Reson Imaging. 5:379–384. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Soto JA, Barish MA, Alvarez O and Medina
S: Detection of choledocholithiasis with MR cholangiography:
comparison of three-dimensional fast spin-echo and single- and
multisection half-Fourier rapid acquisition with relaxation
enhancement sequences. Radiology. 215:737–745. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim JH, Hong SS, Eun HW, Han JK and Choi
BI: Clinical usefulness of free-breathing navigator-triggered 3D
MRCP in non-cooperative patients: comparison with conventional
breath-hold 2D MRCP. Eur J Radiol. 81:e513–e518. 2012. View Article : Google Scholar
|
|
13
|
Berman L, Mitchell KA, Israel G and Salem
RR: Serous cystadenoma in communication with the pancreatic duct:
an unusual radiologic and pathologic entity. J Clin Gastroenterol.
44:e133–e135. 2010.PubMed/NCBI
|
|
14
|
Furukawa H, Takayasu K, Mukai K, et al:
Serous cystadenoma of the pancreas communicating with a pancreatic
duct. Int J Pancreatol. 19:141–144. 1996.PubMed/NCBI
|
|
15
|
Morel A, Marteau V, Chambon E, Gayet B and
Zins M: Pancreatic mucinous cystadenoma communicating with the main
pancreatic duct on MRI. Br J Radiol. 82:e243–e245. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vahlensieck M, Vogel J, Kreft B and Reiser
M: Mucinous cystadenoma of the pancreatic tail with ductal
communication. J Comput Assist Tomogr. 17:502–503. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Beger HG, Poch B and Vasilescu C: Benign
cystic neoplasm and endocrine tumours of the pancreas - when and
how to operate - an overview. Int J Surg. 12:606–614. 2014.
View Article : Google Scholar
|
|
18
|
Papanikolaou N, Karantanas AH, Heracleous
E, et al: Magnetic resonance cholangiopancreatography: comparison
between respiratory-triggered turbo spin echo and breath hold
single-shot turbo spin echo sequences. Magn Reson Imaging.
17:1255–1260. 1999. View Article : Google Scholar : PubMed/NCBI
|