Introduction
In advanced esophageal cancer, the complication of
dysphagia is present at an increasing rate as the condition
progresses. Oral meal intake becomes difficult, therefore, patients
typically present with a nutritional disorder. Furthermore,
dysphagia often leads to the aggravation of Karnofsky performance
status (1) and a decrease in
patient quality of life (2–6). The optimal palliative treatment for
this type of dysphagia has yet to be established, however, stent
placement (2), intracavitary
radiotherapy (ICRT) (3) or external
beam radiation therapy (EBRT) (4)
are currently employed. In cases where it is not possible to use
these treatment strategies or when their effects are insufficient,
enteral nourishment via a gastrostomy tube or central vein
nourishment is performed (7).
A previous study conducted in multiple institutions
determined that ICRT may provide longer-term symptom improvement
for cases of inoperable advanced esophageal cancer with dysphagia,
compared with metallic stent placement (5). Thus, ICRT for the palliative treatment
of advanced esophageal cancer with dysphagia has been performed
since 2005 at the University of Tokyo Hospital (Tokyo, Japan). The
aim of the present study was to evaluate the efficacy of esophageal
ICRT at a dose of 6 Gy/fraction for relieving the symptom of
dysphagia in cases of advanced esophageal cancer.
Patients and methods
Study cohort
In the present study, a retrospective analysis of 24
patients exhibiting esophageal cancer with dysphagia was performed
in a single institute (University of Tokyo Hospital). The subjects
received esophageal ICRT with an iridium (Ir)-192 source for the
palliation of dysphagia. The dysphagia scores were compared prior
to and following irradiation to determine the effect of esophageal
ICRT on symptom alleviation. The dysphagia score was determined
based on the medical treatment records of the Hospital Information
System, irradiation records, and a questionnaire completed by the
patient (or a member of the patient’s family). Patients who
received definitive (50 Gy in 25 fractions or 50.4 Gy in 28
fractions) or palliative (30 Gy in 10 fractions) EBRT a minimum of
three months prior to ICRT were included in the present study.
Palliative ICRT was performed even for patients who developed
dysphagia again or for the first time after undergoing EBRT.
However, patients who received EBRT after ICRT were not included in
the present study. Furthermore, patients who had received
chemotherapy with the aim of prolonging life and who exhibited
cancer-induced esophageal stenosis initially underwent palliative
EBRT as opposed to palliative ICRT. An enhanced computed tomography
(CT) scan, fluorodeoxyglucose-positron emission tomography scan,
esophagography and upper endoscopy were performed to facilitate the
selection of EBRT targets with definitive and palliative intent.
This study was approved by the ethics committee of the University
of Tokyo Hospital.
Questionnaire
An original questionnaire was designed for use in
the present study and consisted of five questions, as follows: Q1.
Do you think that dietary intake improved following ICRT?
(significant improvement/marginal improvement/no change/marginal
deterioration/significant deterioration); Q2. How long was the
improvement maintained? (approximately one day/approximately one
week/two to three weeks/approximately one month/two to three
months/four to five months/longer than five months); Q3. How would
you describe the condition of dietary intake prior to ICRT?
(normal/marginal dysphagia/only rice gruel/only water/nothing); Q4.
What is the condition of dietary intake after ICRT?
(normal/marginal dysphagia/only rice gruel/only water/nothing); and
Q5. Did you experience any side-effects from ICRT? [yes (please
state side-effect/s)/no]. Question numbers three and four were used
to estimate the dysphagia score prior to and following ICRT.
Esophageal ICRT
Esophageal ICRT was performed using high dose rate
(HDR) Ir-192 irradiation equipment [microSelectron®
Digital (HDR V3); Elekta Ltd., Veenendaal, The Netherlands]. A
mitral stenosis (MS) double balloon-type esophageal ICRT applicator
(outer diameter, 20 mm; T405175; Create Medic Co., Ltd., Yokohama,
Japan) and an MS-type bronchial ICRT applicator (size, M; T405181;
Create Medic Co., Ltd.) were used. Although T405181 was developed
as a bronchial ICRT applicator, it was used for esophageal ICRT in
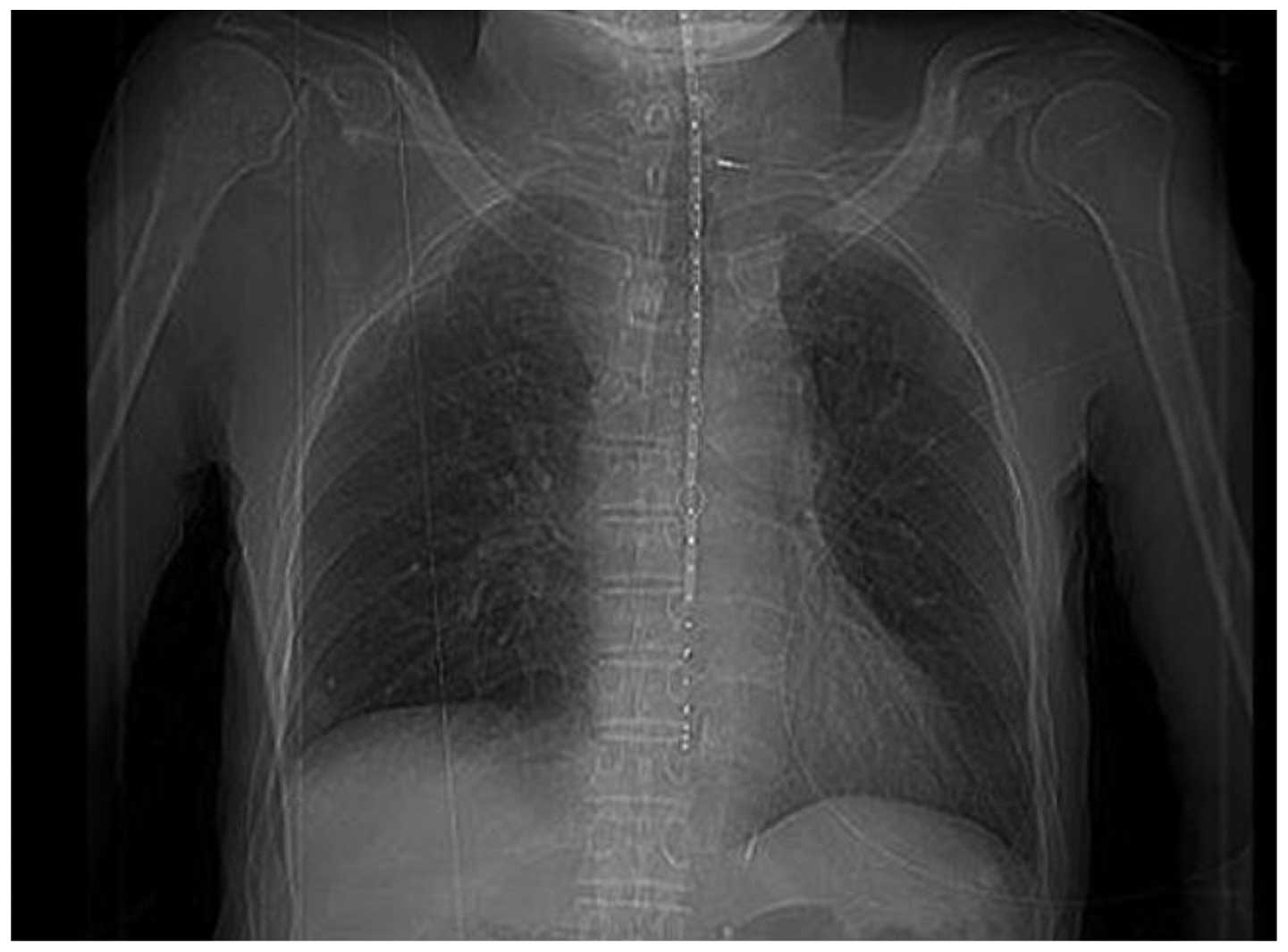
the present study (Fig. 1). The
dose was administered at 5 mm submucosally and the treatment length
was almost equal to the tumor length (±3–5 mm). The dose
distribution of ICRT is indicated in Fig. 2.
Applicator insertion
Hydroxyzine hydrochloride (50 mg; Atarax-P
Parenteral Solution®; Pfizer Japan Inc., Tokyo, Japan)
and an atropine sulfate injection of 0.5 mg (volume, 1 ml) were
administered as anesthesia. No stent was inserted prior to ICRT,
instead a balloon applicator with a 20-mm outer diameter was used.
Treatment planning was conducted using PLATO® and
Oncentra® Brachy software (Chiyoda Corporation, Tokyo,
Japan), and values for the dose (Gy) delivered to 90% of the
clinical target volume (CTV) (D90%), the D100% and the volume (%)
of CTV receiving 100% of the prescribed dose (V100%) were
calculated, with the gross tumor volume regarded as equal to the
CTV. Furthermore, the tumor location was identified as a lesion of
thickened esophageal wall by enhanced CT scan or a lesion with
esophageal stenosis by esophagography using barium.
Dysphagia was evaluated based on the aforementioned
questionnaire and patient medical records, and dysphagia scores
were defined as previously described by Knyrim et al
(5) using the following scores: 0,
able to consume a normal diet/no dysphagia; 1, able to swallow
certain solid foods; 2, able to swallow only semi-solid foods; 3,
able to swallow liquids only; and 4, unable to swallow
anything/total dysphagia. The evaluation was performed prior to and
following ICRT, with the evaluation after ICRT performed when the
greatest response occurred; thus, the evaluation time was not
uniform.
Statistical analysis
A paired t-test was performed to determine whether a
significant difference existed between the mean pre- and post-ICRT
dysphagia scores of 24 patients with esophageal cancer. All
statistical analyses were performed using SAS software version 9.1
(SAS Institute Japan Ltd., Tokyo, Japan). The Common Terminology
Criteria for Adverse Events, version 4.0, was used to evaluate
toxicities (8), the expected
toxicities were esophageal pain, esophageal stenosis, esophageal
obstruction, esophageal ulcer, esophageal fistula, esophageal
perforation, esophageal hemorrhage, esophagitis, or esophageal
necrosis. P<0.05 was considered to indicate a statistically
significant difference.
Results
Patient characteristics are indicated in Table I. The median age of the patients in
the present study was 70.5 years (range, 52–88 years) and the
median follow-up time was 167 days (range, 60–1,001 days). Of the
13 patients that underwent EBRT, the median radiation dose was 50.4
Gy (range, 30–60 Gy) and the median single fraction dose was 1.8 Gy
(range, 1.8–3.0 Gy), with 8/13 patients receiving 50.4 Gy in 28
fractions. Furthermore, ICRT was performed in one patient with no
symptoms of dysphagia, as the esophageal wall thickness adjacent to
the primary tumor appeared significant on the CT scan.
 | Table IPatient characteristics (n=24). |
Table I
Patient characteristics (n=24).
| Characteristic | No. of cases |
|---|
| Gender |
| Male | 22 |
| Female | 2 |
| Age, yearsa |
| ≤59 | 4 |
| 60–69 | 6 |
| 70–79 | 7 |
| ≥80 | 7 |
| Karnofsky performance
status, % |
| 70 | 2 |
| 80 | 10 |
| 90 | 12 |
| Pathological
type |
| Squamous cell
carcinoma | 21 |
| Adenocarcinoma | 2 |
| Unknown | 1 |
| Primary tumor
site |
| Cervix | 1 |
| Upper thoracic | 4 |
| Middle thoracic | 5 |
| Lower thoracic | 14 |
| External beam
radiation therapy |
| Without | 11 |
| With | 13 |
The single fraction dose of esophageal ICRT was 4 Gy
in one case and 6 Gy in all other cases. All patients were treated
with single fraction doses and additional ICRT was performed
according to the effect of the previous fraction. Accordingly, the
mean number of fractions administered was 1.7 (maximum, four
fractions). Independent of EBRT, the mean and median prescribed
ICRT doses per fraction were 9.7 and 6.0 Gy, respectively (range,
4.0–10.0 Gy). Furthermore, the mean treatment length was 8.2 cm
(range, 1.0–18 cm), and the median D90%, D100% and V100% per
fraction were 4.2 Gy (range, 3.4–5.0 Gy), 2.9 Gy (range, 2.3–3.5
Gy) and 80% (range, 74–86%), respectively.
The post-ICRT shift in dysphagia scores indicated in
Fig. 3 was determined using the
data from questions three and four of the questionnaire. In all
patients, the dysphagia score was stable or improved from pre- to
post-ICRT, and the average dysphagia score (mean ± standard
deviation) markedly decreased from 2.54±1.33 to 1.65±1.42 in the
24-patient cohort (P=0.083; paired t-test; Fig. 4). No significant difference was
identified in the improvement of the dysphagia score between
patients with and without EBRT, or between patients receiving a
total ICRT dose of >9.7 Gy and <9.7 Gy (mean value, 9.7
Gy).
The improvement in dysphagia was evaluated using
question one of the questionnaire. Six cases were considered to
have significantly improved, seven cases were marginally improved,
no change occurred in four cases, and no patients stated marginal
or significant deterioration of dysphagia. Furthermore, seven cases
did not provide an answer to question one.
In addition, the duration time of dysphagia
indicated in Fig. 5 was determined
using data from question two of the questionnaire. The duration of
dysphagia was approximately one week in three patients, two to
three weeks in four patients, and approximately one, two to three,
four to five and longer than five months in two patients,
respectively. In the patient with the maximal reaction, the
duration of dysphagia was >10 months, with continuing
improvement observed until the completion of follow-up.
Using data obtained from question five of the
questionnaire, no complications of ICRT were noted in 17 cases,
however, pain occurred in four cases, appetite loss in four cases
and nausea in two cases. These complications were transient (i.e.,
improvement was observed between 24 h and a few weeks) and did not
require the administration of therapeutic agents.
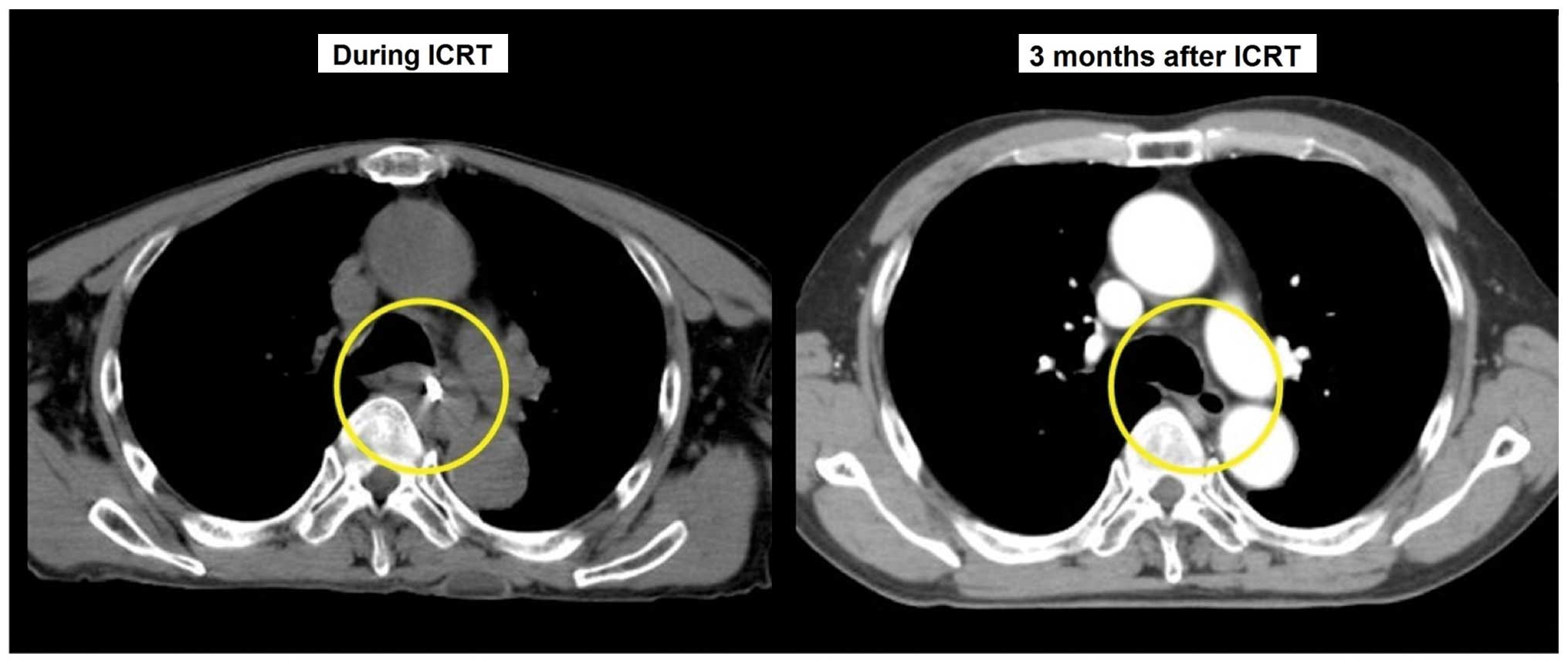
Fig. 6 shows a CT
scan of a patient (age, 68 years old) demonstrating a marked
improvement in esophageal wall thickness at three months post-ICRT
compared with during ICRT.
Pain was the most frequent side-effect of esophageal
ICRT (15% of cases), possibly due to pharyngitis and/or
esophagitis. No severe complications requiring hospital treatment
occurred. Neither esophageal pain, bleeding, fistulas, perforation,
stenosis, obstruction, necrosis, nor esophagitis of grades 3–5 were
observed.
Discussion
In total, >50% of patients with esophageal cancer
exhibit inoperable disease at presentation (5). The majority of these patients require
palliative treatment to relieve progressive dysphagia or fistula
formation. Therefore, the aim of the present study was to determine
the effectiveness of ICRT for the palliative treatment of
symptomatic esophageal cancer, using a questionnaire for patients
(or their family members) and medical records from the Hospital
Information System. It was determined that an improvement in the
symptom of dysphasia occurred with the application of small
fractions of ICRT, indicating its possible clinical value.
At present, the endoscopic placement of a covered
self-expanding metal stent is the preferred treatment strategy for
an esophagorespiratory fistula (9).
Alternative commonly used strategies for the palliation of
dysphagia include laser therapy (10), EBRT in combination with ICRT
(11) and ICRT as a single
treatment (12). One of the
disadvantages of laser therapy is the fact that repeated sessions
are required to achieve and maintain adequate palliation (10). Furthermore, combining EBRT and ICRT
is a process that is often too intensive for patients with an
inoperable disease state, metastatic disease or a poor medical
condition. Therefore, in numerous patients with such a disease
state, a self-expanding metal stent is inserted or single-dose ICRT
is performed to palliate dysphagia (7). These two treatment strategies have
proved to be effective, with few complications (7,9–12),
however, their relative effectiveness is unknown. According to a
study by Siersema et al (9),
dysphagia improved in all 100 studied patients four weeks after the
insertion of a self-expanding metal stent. Although laser therapy
can result in successful tumor recanalization in >90% of
appropriately selected patients and a return to the consumption of
solids is observed in the majority of patients following treatment
with the neodymium-doped yttrium aluminum garnet laser, laser
therapy must be repeated every 4–6 weeks as the tumor regrows
(10). According to a study by Homs
et al (12), six weeks after
the administration of 6–20 Gy HDR ICRT (median dose, 15 Gy)
prescribed 5 mm submucosally, patients demonstrated significantly
improved dysphagia scores, with a decrease from a median score of
three to a score of two (n=104; P<0.001). Additionally, the
incidence of early major complications was low. Similarly, in
studies using HDR ICRT for the palliation of patients with
inoperable esophageal carcinoma (13–15),
dysphagia improved in 90–100% of cases by administering 20 Gy in
three fractions, and 12, 12.5 and 15 Gy in a single fraction.
As ICRT was administered with palliative intent,
imaging examinations, such as CT scans, were not performed in order
to evaluate the antitumor efficacy of ICRT in the present study. A
significant difference was not observed in the improvement of
dysphagia score between the patients with and without EBRT, and
between the total ICRT dose received. This may be as patients who
repeatedly received palliative ICRT 2–4 times and who were
prescribed the higher total ICRT dose, or who were administered
with EBRT prior to ICRT, experienced flare-ups in the symptom of
dysphagia subsequent to ICRT or EBRT. Therefore, an association
between dose and symptom relief was not identified in the present
study.
Palliative ICRT was performed for all 24 patients in
the present study who exhibited advanced esophageal cancer with
dysphagia. Although the questionnaire was completed by only 17 of
the 24 patients, the dysphagia state was evaluated for all
patients, as the score was based on the medical records from the
Hospital Information System, as well as the questionnaire. The
current study identified a trend in the improvement of the symptom
of dysphagia following esophageal ICRT from 2.54±1.33 to 1.65±1.42,
however, the difference was not significant. Pain was the most
frequent (15% of cases) side-effect of the esophageal ICRT,
possibly due to pharyngitis and/or esophagitis. No severe
complications requiring hospital treatment occurred.
The treatment results are generally in agreement
with those of previously conducted studies, however, the single
fraction doses of 4–6 Gy used in the present study are relatively
low compared with the treatment doses used in previous studies
(5,12–14).
In the current study, 13/24 patients received EBRT. In such
patients, the tumors may achieve radioresistance and the
radio-tolerability of healthy tissue may be reduced. Therefore, it
is important to determine if a lower total treatment dose and
single fraction doses are sufficient to achieve the same efficacy
for such patients. However, the number of patients investigated in
the present study was small and therefore insufficient to draw such
conclusions from.
In conclusion, in the present study a trend was
identified in the improvement of the symptom of dysphagia following
esophageal ICRT in advanced esophageal cancer patients, however,
the results were not signficant. The present study considers that
an ICRT dose per fraction of 6 Gy prescribed 5 mm beneath the
esophageal mucous membrane may be sufficient for the palliative
treatment of dysphagia in advanced esophageal cancer patients,
however, a higher dose of 12–15 Gy has been recommended in previous
studies, so further elucidation is required.
References
|
1
|
Friendlander AH and Ettinger RL: Karnofsky
performance status scale. Spec Care Dentist. 29:147–148. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bayraktar O, Bayraktar B, Atasoy D,
Erenler I, Ozdemir IA, Boluk S, Bayraktar OU, Bayraktar A, Tortum
OB and Yigitbasi R: Covered self-expandable metallic stents could
be used successfully in the palliation of malignant cervical
esophageal strictures: preliminary report. Surg Laparosc Endosc
Percutan Tech. 23:e41–e44. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Amdal CD, Jacobsen AB, Sandstad B, Warloe
T and Bjordal K: Palliative brachytherapy with or without primary
stent placement in patients with oesophageal cancer, a randomized
phase III trial. Radiother Oncol. 107:428–433. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Eldeeb H, Reza S, Shmueli U, Logsdail G,
Hinks P and Mukherjee S: External beam radiotherapy versus
brachytherapy in the management of malignant oesophageal dysphagia:
a retrospective study. J BUON. 17:508–511. 2012.PubMed/NCBI
|
|
5
|
Homs MY, Steyerberg EW, Eijkenboom WM,
Tilanus HW, Stalpers LJ, Bartelsman JF, van Lanschot JJ, Wijrdeman
HK, Mulder CJ, Reinders JG, et al: Single-dose brachytherapy versus
metal stent placement for the palliation of dysphagia from
oesophageal cancer: multicentre randomised trial. Lancet.
364:1497–1504. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Knyrim K, Wagner HJ, Bethge N, Keymling M
and Vakil N: A controlled trial of an expansile metal stent for
palliation of esophageal obstruction due to inoperable cancer. N
Engl J Med. 329:1302–1307. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Allum WH, Griffin SM, Watson A and
Colin-Jones D; Association of Upper Gastrointestinal Surgeons of
Great Britain and Ireland; British Society of Gatroenterology;
British Association of Surgical Oncology. Guidelines for the
management of oesophageal and gastric cancer. Gut. 50(Suppl 5):
v1–v23. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Common Terminology Criteria for Adverse
Events (CTCAE) version 4.0. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf#search='CTCAE'.
Accessed ?
|
|
9
|
Siersema PD, Hop WC, van Blankenstein M,
et al: A comparison of 3 types of covered metal stents for the
palliation of patients with dysphagia caused by esophagogastric
carcinoma: a prospective, randomized study. Gastrointest Endosc.
54:145–153. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Spencer GM, Thorpe SM, Blackman GM, et al:
Laser augmented by brachytherapy versus laser alone in the
palliation of adenocarcinoma of the oesophagus and cardia: a
randomised study. Gut. 50:224–227. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schraube P, Fritz P and Wannenmacher MF:
Combined endoluminal and external irradiation of inoperable
oesophageal carcinoma. Radiother Oncol. 44:45–51. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Homs MY, Eijkenboom WM, Coen VL, et al:
High dose rate brachytherapy for the palliation of malignant
dysphagia. Radiother Oncol. 66:327–332. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Harvey JC, Fleischman EH, Bellotti JE and
Kagan AR: Intracavitary radiation in the treatment of advanced
esophageal carcinoma: a comparison of high dose rate vs. low dose
rate brachytherapy. J Surg Oncol. 52:101–104. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kulhavy M, Sur RK, Levin CV, Donde B and
Luhana F: Optimization of single-fraction high dose rate
intraluminal brachytherapy in palliation of advanced esophageal
cancer: a preliminary report. Endocurie Hypertherm Oncol.
11:235–239. 1995.
|
|
15
|
Leung JT and Kuan R: Brachytherapy in
oesophageal carcinoma. Australas Radiol. 39:375–378. 1995.
View Article : Google Scholar : PubMed/NCBI
|