Introduction
Ovarian cancer is a gynecological malignancy with a
high rate of mortality. Due to a lack of notable symptoms in the
early stages, 60% of patients present with advanced-stage disease
at diagnosis (1). The primary
clinical treatment for ovarian cancer is cytoreductive surgery
combined with platinum-based chemotherapy. Chemotherapy is a
significant part of the radical treatment approach for ovarian
cancers, however, platinum-based chemotherapies are prone to drug
resistance; a factor that affects treatment efficacy and
contributes to poor prognoses. At present, the five-year survival
rate for ovarian cancer is 30–50% (2). Therefore, in order to improve the
prognoses of these patients, the issue of drug-resistance must be
addressed. Previous studies have identified that the abnormal
regulation of autophagy is directly associated with tumorigenesis
(3–5). Therefore, autophagy has become a novel
target for the investigation of tumorigenesis, the inhibition of
tumor growth and for determining how to overcome
chemotherapy-associated drug resistance. However, the mechanism
involved in the regulation of autophagy is complex.
BECN1, an autophagy-related gene located on
human chromosome 17q21, encodes the protein Beclin-1, which
participates in the formation of phages and can inhibit tumor
growth by increasing the rate of autophagy. BECN1 has
therefore been identified as a candidate tumor suppressor gene for
ovarian cancer (6). Previous
studies have revealed that the expression of Beclin-1 is
downregulated in breast (7),
prostate (8) and nasopharyngeal
(9) carcinomas. Further studies
have revealed that a loss of Beclin-1 expression results in reduced
autophagy activity and increased tumorigenesis (10). The PTEN gene, located on
chromosome 10, is a tumor suppressor gene with dual specificity
phosphatase activity. The phosphatase and tensin homolog (PTEN)
protein is involved in the regulation of a variety of cellular
signal transduction pathways, and is closely associated with cell
growth and differentiation, and with tumorigenesis. Furthermore,
PTEN is able to initiate autophagy and therefore inhibit tumor
growth. In the present study, the protein expression of Beclin-1
and PTEN in ovarian cancer tissues was detected using
immunohistochemistry. The study aimed to investigate the role of
Beclin-1 and PTEN, and the association with resistance in ovarian
cancer. The effect of autophagic changes in cases of drug-resistant
ovarian cancer was also examined, in order to further elucidate on
the mechanism of drug resistance and aid in the eventual overcoming
of ovarian cancer.
Materials and methods
Patient characteristics
In total, 40 tissue samples were obtained from
patients with ovarian cancer who had undergone cytoreductive
surgical resection at the Shengjing Hospital of China Medical
University (Shenyang, China) between January 2007 and May 2012. The
cases were classified as serous carcinoma (n=24), mucinous
carcinoma (n=8), clear cell carcinoma (n=4), endometrial carcinoma
(n=2) or undifferentiated carcinoma (n=2). The age range of the
patients was 35 to 58 years old, with a median age of 48 years old.
The pathological surgical staging was performed according to the
2009 International Federation of Gynecology and Obstetrics system
as follows: Stage I, two cases; stage II, 10 cases; stage III, 24
cases; and stage IV, four cases (11).
The telephone or hospital examination follow-ups of
the 40 cases of ovarian cancer began at diagnosis and ended on
December 31, 2012. The patients were pathologically diagnosed with
ovarian cancer and divided into a chemotherapy-sensitive (n=20) or
chemotherapy-resistant (n=20) group, according to the results of
the pre- or post-operative normative chemotherapy and the
post-operative follow-up. The grouping standards were as follows:
i) Achievement of clinical remission following the initial
platinum-based chemotherapy was necessary for study inclusion; and
ii) cases with relapse at six months or more following the end of
the chemotherapy program were taken as the chemotherapy-sensitive
group, and cases with relapse within six months were used as the
chemotherapy-resistant group. This study was approved by the ethics
committee of Shengjing Hospital of China Medical University and
written informed consent was obtained from all patients.
Immunohistochemical analysis
The Beclin-1 polyclonal rabbit (1:100 dilution) and
PTEN monoclonal mouse (1:75 dilution) antigen solutions were
purchased from Proteintech (Chicago, IL, USA). The
immunohistochemistry Power Vision kit and 3,3′-diaminobenzidine
reagent were purchased from Beijing Golden Bridge Zhongshan
Biotechnology Co., Ltd. (Beijing, China).
Phosphate-buffered saline solution was used for the
negative control, and normal known-positive ovarian tissue samples
were used for the positive control. Using the Power Vision kit, the
experimental procedure was performed according to the
manufacturer’s instructions. A total of 10 randomly selected
high-magnification fields were analyzed under an optical microscope
(AX70; Olympus Corporation, Tokyo, Japan) 48 h after sealing.
PTEN-positive cells were identified by clear-brown granules located
in the nucleus or cytoplasm, and Beclin-1-positive cells were
identified by brown particles distributed throughout the cytoplasm.
The percentage of positive cells to total cells was counted and
awarded points according to the following criteria: <10%, 0
points; 10–20%, 1 point; 21–50%, 2 points; and >50%, 3 points.
The intensity of staining was also awarded points according to the
following system: no color, 0 points; pale yellow, 1 point; brown,
2 points; and tan, 3 points. The total score for each case was the
sum of the points for the percentage of positive cells and the
staining intensity. A score of ≤3 was regarded as negative for
PTEN/Beclin-1 expression, whereas a score of >3 was regarded as
positive for PTEN/Beclin-1 expression.
Statistical analysis
The statistical analysis was performed using SPSS
11.0 (SPSS, Inc., Chicago, IL, USA). The association between the
clinicopathological parameters and the protein expression of
Beclin-1 and PTEN was analyzed using Student’s t-test. The
Spearman’s ρ test was used for the correlation analysis.
Results
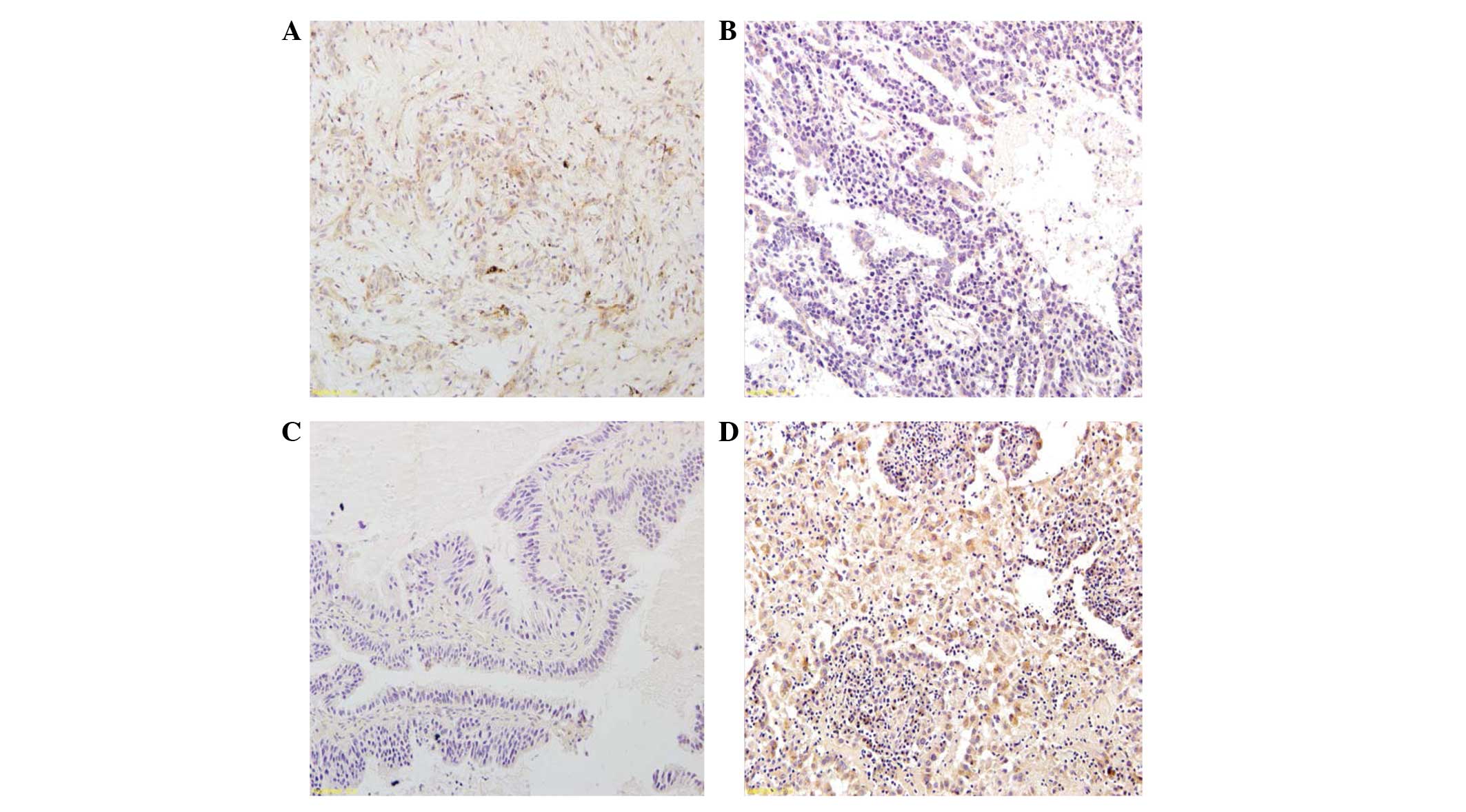
In the 40 cases of ovarian cancer included in the
present study, the expression of Beclin-1 was revealed to be
primarily located in the cytoplasm. The positive rate of Beclin-1
expression was significantly lower in the chemotherapy-resistant
group (35.0%) compared with the chemotherapy-sensitive group
(50.0%) (P<0.05). The expression of PTEN was identified to be
primarily located in the nucleus or cytoplasm. The positive rate of
PTEN expression was significantly lower in the
chemotherapy-resistant group (30.0%) compared with the
chemotherapy-sensitive group (65.0%) (P<0.05; Table I; Fig.
1).
 | Table IExpression of Beclin-1 and PTEN in
chemoresistant and chemosensitive groups. |
Table I
Expression of Beclin-1 and PTEN in
chemoresistant and chemosensitive groups.
| | Beclin-1 | PTEN |
|---|
| |
|
|
|---|
| Group | n | − | + | % positive | − | + | % positive |
|---|
| Resistant | 20 | 13 | 7 | 35.0 | 14 | 6 | 30.0 |
| Sensitive | 20 | 10 | 10 | 50.0 | 7 | 13 | 65.0 |
The correlation analysis revealed that the intensity
of Beclin-1 expression was positively correlated with the
expression of PTEN in the 40 cases of ovarian cancer (P<0.05;
Table II).
 | Table IIAssociation between Beclin-1 and PTEN
expression. |
Table II
Association between Beclin-1 and PTEN
expression.
| Beclin-1 |
|---|
|
|
|---|
| Protein | + | − |
|---|
| PTEN |
| + | 12 | 5 |
| − | 7 | 16 |
Discussion
Autophagy is a lysosomal degradation process for
cellular macromolecules and damaged organelles, and an alternative
form of programmed cell death to apoptosis in eukaryotes. Changes
in the activity of signaling, transport and negative regulatory
pathways of macrophages have been revealed to be associated with
tumor occurrence and development. Furthermore, the abnormal
expression of autophagy genes has been identified to activate or
inhibit the formation of certain tumors (12).
The PTEN protein is encoded by the PTEN tumor
suppressor gene located on chromosome 10 (13). Since the discovery of the gene in
1997, PTEN has gained particular attention for its role in
cancer (14). Previous studies have
demonstrated that the gene is associated with endometrial (15) and prostate cancers (16), and with malignant gliomas (17). According to the literature, genetic
alterations in PTEN, such as mutation, loss of
heterozygosity, hypermethylation, microsatellite instability or
translational modifications result in the ‘silencing’ of gene
expression (18). Previous studies
revealed that the inhibition of autophagy was removed by inhibiting
the change of PTEN 4,5-phosphatidylinositol diphosphate (PIP2) to
3,4,5-triphosphate phosphatidylinositol (PIP3) to participate in
autophagy regulation. It has been demonstrated that PTEN and
other autophagy-related genes are expressed in normal ovarian
tissues, benign ovarian tumors and borderline ovarian tumors, but
are downregulated in cases of ovarian cancer. This suggests that
the decreased expression of autophagy-related proteins, such as
PTEN, may be closely correlated with the development of ovarian
cancer (19,20). In addition, PTEN protein expression
has been identified to be positively correlated with the
differentiation state of ovarian cancers (21). A previous study demonstrated that a
chemical, EF24, conferred sensitivity to drug-resistant ovarian
cancer cells via the upregulation of PTEN expression (22). Furthermore, Wu et al
(23) upregulated PTEN protein
expression in a cisplatin-resistant ovarian cancer C13K cell line
via the in vitro liposomal transfection of the PTEN
gene. The C13K cells exhibited increased sensitivity to
cisplatin-induced apoptosis compared with empty vector-transfected
cells. An in vitro study by Yan et al (24) demonstrated that PTEN protein
overexpression increased the sensitivity of the chemoresistant cell
lines, CI3* and A2780cp, to cisplatin-induced apoptosis through the
upregulation of p53, rather than the inhibition of Akt protein
activation. It was further revealed that low PTEN expression was
apparent in the OVCAR-3/CDDP drug-resistant ovarian cancer cell
line compared with the normal OVCAR-3 ovarian cancer cell line. The
phosphoinositide 3-kinase (PI3K)/Akt pathway is an important
pathway involved in the regulation of autophagy, and has been
revealed to be inhibited by PTEN. The study identified that PTEN
protein expression was significantly lower in the drug-resistant
ovarian cancer tissues compared with the drug-sensitive group. This
suggested that PTEN was involved in the mechanism of drug
resistance in ovarian cancer tissues via the process of
autophagy.
The ~150-kb human BECN1 gene is a homolog of
the atg6/vps30 yeast gene and is located on chromosome 17q21.
BECN1 has been revealed to be involved in the development of
tumors by the regulation of autophagy (25). At present, autophagy as a barrier
for impeding tumorigenesis or tumor adaptive responses remains
controversial (26). On the one
hand, tumor cells are often restricted due to rapid growth, and
therefore autophagy offers an adaptive response for tumor cell
survival. On the other hand, certain studies have demonstrated that
tumor progression is inhibited by the stimulation of non-apoptotic
cell death processes, namely autophagy (27). Therefore, autophagy both inhibits
tumor formation and promotes tumor development, and this
association remains controversial. Recently, the dynamic role of
autophagy in cancer was proposed by Kimmelman (28). The study suggested that autophagy
initially acts as a barrier to prevent the initiation of tumors,
but that following the formation of lesions, it positively affects
malignancy and tumor maintenance. A recent study revealed that
Beclin-1 expression levels differed between types of tumor cell.
The expression of Beclin-1 was identified to be downregulated in a
variety of tumor cells, such as those of breast, ovarian and
prostate cancers, and gliomas (4).
Despite this, high levels of autophagy activity were maintained in
other cancer cells. In a study by Ahn et al (29), samples from 103 patients with
colorectal cancer, and 60 with gastric cancer, were
immunohistochemically analyzed. Beclin-1 expression was observed in
95 and 83% of the colorectal and gastric cancer samples,
respectively. By contrast, little or no expression was revealed in
the normal gastric and colorectal tissues. Tang et al
(30) identified that the mRNA and
protein expression levels of Beclin-1 were upregulated in hepatitis
B virus-mediated liver cancer, which suggested a role for Beclin-1
in tumor formation. The present study revealed that Beclin-1
protein expression was significantly lower in the drug-resistant
group of ovarian cancer tissues compared with the drug-sensitive
group. Furthermore, the differences in expression were significant,
which suggested that decreased Beclin-1 expression, and the
activity of macrophages, may be associated with chemotherapy
resistance and poor prognoses in patients with ovarian cancer.
Conversely, an upregulation in the expression of the Beclin-1
protein may increase the sensitivity of ovarian cancers to
chemotherapy, which could improve treatment efficiency and
prognoses.
The present study indicated that Beclin-1 and PTEN
may be co-involved in the regulation of autophagy, and therefore
affect the occurrence and development of cancer. Autophagic protein
turnover is regulated by type I and III PI3Ks. Type I PI3K, and the
downstream signal conversion components Akt and target of
rapomycin, can inhibit autophagy. PTEN induces autophagy by
negative regulation of the type I PI3K. By contrast, the type III
PI3K is necessary for the autophagic formation of lysosomal
vacuoles. Beclin-1 regulates autophagic activity by modulating the
precursor structure of Apg proteins, primarily by the formation of
complexes with the type III PI3K. Therefore, Beclin-1 and PTEN may
possess similar roles in the self-regulation of macrophage activity
(31). The results of the present
study revealed that the protein expression of Beclin-1 and PTEN
exhibited a significant correlation. This indicated that the
proteins may participate together in the mechanism of drug
resistance observed in platinum-resistant ovarian cancers.
In summary, the protein expression of Beclin-1 and
PTEN was downregulated, which suggested that a decrease in
autophagic activity may be associated with drug-resistant ovarian
cancers. At present, the specific mechanisms that regulate
autophagy remain unclear. Further study will aid in clarifying the
role of autophagy, which may provide novel solutions for treating
chemotherapy-resistant ovarian cancers, and establish a reliable
theoretical basis for the development of novel drugs.
The expression of the Beclin-1 and PTEN proteins, in
drug-resistant and drug-sensitive ovarian cancers, was detected
using immunohistochemistry and analyzed for potential correlations.
The results revealed that Beclin-1 and PTEN protein expression was
significantly lower in the chemotherapy-resistant group compared
with the chemotherapy-sensitive group. Furthermore, the difference
in expression was identified to be significant and positively
correlated. The results suggested that Beclin-1 and PTEN protein
expression decreased in the drug-resistant ovarian cancer tissues.
Therefore, it was concluded that the occurrence of drug resistance
in ovarian cancers was closely associated with a low expression of
PTEN and Beclin-1. In conclusion, a reduction in autophagic
activity, induced by the interaction between Beclin-1 and PTEN, may
lead to drug resistance in cases of ovarian cancer.
Acknowledgements
This study was funded by the Doctor Started Natural
Science Foundation (no. 20071047), the Higher Education Department
Research Program (no. 2009A724), the Liaoning Science and
Technology Program (no. 2010225032) and the National Natural
Science Foundation of China (nos. 81372486 and 81302270).
References
|
1
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lee S, Choi EJ, Jin C and Kim DH:
Activation of PI3K/Akt pathway by PTEN reduction and PIK3CA mRNA
amplification contributes to cisplatin resistance in an ovarian
cancer cell line. Gynecol Oncol. 97:26–34. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hara T, Nakamura K, Matsui M, et al:
Suppression of basal autophagy in neural cells causes
neurodegenerative disease in mice. Nature. 441:885–889. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huang X, Bai HM, Chen I, Li B and Lu YC:
Reduced expression of LC3B-II and Beclin 1 in glioblastoma
multiforme indicates a down-regulated autophagic capacity that
relates to the progression of astrocytic tumors. J Clin Neurosci.
17:1515–1519. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Koren I and Kimchi A: Cell biology.
Promoting tumorigenesis by suppressing autophagy. Science.
338:889–890. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lin HX, Qiu HJ, Zeng F, et al: Decreased
expression of Beclin 1 correlates closely with Bcl-xL expression
and poor prognosis of ovarian carcinoma. PLoS One. 8:e605162013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yao Q, Chen J, Lv Y, et al: The
significance of expression of autophagy-related gene Beclin, Bcl-2,
and Bax in breast cancer tissues. Tumour Biol. 32:1163–1171. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xu LW, Qian M, Jia RP, et al: Expression
and significance of microsomal prostaglandin synthase-1 (mPGES-1)
and Beclin-1 in the development of prostate cancer. Asian Pac J
Cancer Prev. 13:1639–1644. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wan XB, Fan XJ, Chen MY, et al: Elevated
Beclin 1 expression is correlated with HIF-1alpha in predicting
poor prognosis of nasopharyngeal carcinoma. Autophagy. 6:395–404.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yue Z, Jin S, Yang C, Levine AJ and Heintz
N: Beclin 1, an autophagy gene essential for early embryonic
development, is a haploinsufficient tumor suppressor. Proc Natl
Acad Sci USA. 100:15077–15082. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pecorelli S: Revised FIGO staging for
carcinoma of the vulva, cervix, and endometrium. Int J Gyneeol
Obstet. 105:103–111. 2009. View Article : Google Scholar
|
|
12
|
Kondo Y and Kondo S: Autophagy and cancer
therapy. Autophagy. 2:85–90. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li DM and Sun H: TEP1, encoded by a
candidate tumor suppressor locus, is a novel protein tyrosine
phosphatase regulated by transforming growth factor beta. Cancer
Res. 57:2124–2129. 1997.PubMed/NCBI
|
|
14
|
Li DM and Sun H: TEP1, encoded by a
candidate tumor suppressor locus, is a novel protein tyrosine
phosphatase regulated by transforming growth factor beta. Cancer
Res. 57:2124–2129. 1997.PubMed/NCBI
|
|
15
|
Lee H, Choi HJ, Kang CS, Lee HJ, Lee WS
and Park CS: Expression of miRNAs and PTEN in endometrial specimens
ranging from histologically normal to hyperplasia and endometrial
adenocarcinoma. Mod Pathol. 25:1508–1515. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Patel R, Gao M, Ahmad I, Fleming J, Singh
LB, Rai TS, McKie AB, Seywright M, Barnetson RJ, Edwards J, et al:
Sprouty2, PTEN, and PP2A interact to regulate prostate cancer
progression. J Clin Invest. 123:1157–1175. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Molina JR, Agarwal NK, Morales FC, Hayashi
Y, Aldape KD, Cote G and Georgescu MM: PTEN, NHERF1 and PHLPP form
a tumor suppressor network that is disabled in glioblastoma.
Oncogene. 31:1264–1274. 2012. View Article : Google Scholar
|
|
18
|
Yang L, Kuang LG, Zheng HC, et al: PTEN
encoding product: a marker for tumorigenesis and progression of
gastric carcinoma. World J Gastroenterol. 9:35–39. 2003.PubMed/NCBI
|
|
19
|
Laudański P, Kowalczuk O,
Klasa-Mazurkiewicz D, et al: Selective gene expression profiling of
mTOR-associated tumor suppressor and oncogenes in ovarian cancer.
Folia Histochem Cytobiol. 49:317–324. 2011. View Article : Google Scholar
|
|
20
|
Skírnisdóttir I and Seidal T: Prognostic
impact of concomitant p53 and PTEN on outcome in early stage (FIGO
I-II) epithelial ovarian cancer. Int J Gynecol Cancer.
21:1024–1031. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gadducci A, Guerrieri ME and Genazzani AR:
New insights on the pathogenesis of ovarian carcinoma: molecular
basis and clinical implications. Gynecol Endocrinol. 28:582–586.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Selvendiran K, Tong L, Vishwanath S, et
al: EF24 induces G2/M arrest and apoptosis in cisplatin-resistant
human ovarian cancer cells by increasing PTEN expression. J Biol
Chem. 282:28609–28618. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wu HJ, Wu HT, Weng DH, et al: Reversal of
drug resistance in human ovarian cancer ceils by wild-type PTEN
gene and its mechanisms. Zhonghua Fu Chan Ke Za Zhi. 42:612–616.
2007.(In Chinese). PubMed/NCBI
|
|
24
|
Yan X, Fraser M, Qiu Q and Tsang BK:
Over-expression of PTEN sensitizes human ovarian cancer cells to
cisplatin-induced apoptosis in a p53-dependent manner. Gynecol
Oncol. 102:348–355. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Scarlatti F, Maffei R, Beau I, Codogno P
and Ghidoni R: Role of non-canonical Beclin 1-independent autophagy
in cell death induced by resveratrol in human breast cancer cells.
Cell Death Differ. 15:1318–1329. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sun Y, Liu JH, Jin L, et al:
Over-expression of the Beclin1 gene upregulates chemosensitivity to
anti-cancer drugs by enhancing therapy-induced apoptosis in cervix
squamous carcinoma CaSki cells. Cancer Lett. 294:204–210. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Levine B and Kroemer G: Autophagy in the
pathogenesis of disease. Cell. 132:27–42. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kimmelman AC: The dynamic nature of
autophagy in cancer. Genes Dev. 25:1999–2010. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ahn CH, Jeong EG, Lee JW, et al:
Expression of beclin-l, an autophagy-related protein, in gastric
and colorectal cancers. APMIS. 115:1344–1349. 2007. View Article : Google Scholar
|
|
30
|
Tang H, Da L, Mao Y, et al: Hepatitis B
virus X protein sensitizes cells to starvation-induced autophagy
via up-regulation of beclin 1 expression. Hepatology. 49:60–71.
2009. View Article : Google Scholar
|
|
31
|
Edinger AL and Thompson CB: Defective
autophagy leads to cancer. Cancer Cell. 4:422–424. 2003. View Article : Google Scholar
|