Introduction
Multiform glioblastoma is the most common primary,
highly invasive, malignant tumor of the central nervous system,
with an extremely poor prognosis. The median survival of patients
after surgical resection, radiation therapy and chemotherapy does
not exceed 12–15 months (1–3). The tumor is characterized by invasive
growth, infiltration of the brain substance and high resistance to
radiation and drug therapy, and thus, novel approaches are required
for the treatment of the disease (4). In previous studies, the phenomenon of
the directional migration of neural stem and progenitor cells in
tumor tissue has been a focus, and has presented a significant
opportunity for the targeted delivery of drug molecules to
tumor-specific genes, antibodies and other therapeutic agents
(5–9). In this way, the problem of selecting
the optimal cell lines for transplantation is particularly
important as the use of the patients own neural stem cells carries
a high risk of neoplastic transformation (10–12).
We believe that hematopoietic
CD34+/CD133+ stem cells may represent an
alternative, as their collection and maintenance presents little
difficulty, their use is not associated with ethical and legal
restrictions and they have been successfully used for the treatment
of cancer patients for >50 years (13).
In addition, studies have focused on neural stem and
progenitor cells of the human brain as the most likely origin of
malignant gliomas (5,14,15).
The ability of hematopoietic progenitor cells and human adult
mammals to migrate directionally in neoplastic foci identifies
fundamentally novel aspects of carcinogenesis processes in the
brain.
The aim of the present study was to obtain
experimental evidence of the ability of hematopoietic progenitors
of adult mammalian cells to cause the directed migration of rat
glioma C6 lines when co-cultured. The study was approved by the
ethics committee of the Far Eastern Federal University School of
Biomedicine (Vladivostok, Russia), from December 14, 2012.
Materials and methods
Hematopoietic stem cells of rats
Rat hematopoietic stem cells were provided by the
National Institute for Regenerative Medicine (Moscow, Russia). The
phenotype and purity of the cell population was characterized by a
FACScan flow cytometer (Becton-Dickinson, Franklin Lakes, NJ, USA)
using anti-CD34/anti-CD133 fluorescein isothiocyanate-conjugated
monoclonal antibodies. Prior to co-culture, the cells were stained
with a fluorescent marker, the Vybrant CFDA SE Cell Tracer (V12883;
Life Technologies, Grand Island, NY, USA), according to the
manufacturer’s instructions.
C6 glioma culture
The rat C6 glioma cell line has been used in
previous studies as it exhibits similar characteristics to human
gliblastoma cells, such as invasive growth and atypical nuclei
(16,17). The C6 glioma line was provided by
the School of Biomedicine, Far Eastern Federal University for the
experiment. An aliquot containing 1×106 tumor cells was
thawed for 5 min at 37°C and washed free of dimethyl sulfoxide
(Sigma-Aldrich, St. Louis, MO, USA), using Dulbecco’s modified
Eagle’s medium (DMEM; Gibco Life Technologies, Carlsbad, CA, USA)
containing 10% fetal bovine serum (FBS; Life Technologies) and 100X
antibiotic-antimycotic (10,000 U/ml; Life Technologies). The cells
were precipitated by centrifugation (120 × g for 3 min), fresh
medium (DMEM) was added and then the cells were seeded into 50-ml
culture flasks. Cultivation was continued until monolayer
formation. Next, the cells were detached by enzymatic dissociation
(0.05% trypsin-EDTA; MP Biomedicals, Santa Ana, CA, USA; 1:4; 10
min; 37°C), and after centrifugation (120 × g for 3 min) the
supernatant was discarded and the cells were resuspended in fresh
medium. Tumorigenicity was analyzed following the implantation of
0.5×106 C6 glioma cells into the brain of adult rats
using a stereotaxic device (Model 900 Small Animal Stereotaxic
Instrument; David Kopf Instruments, Tujunga, CA, USA) as described
previously (5).
Isolation of primary cultures of rat
fibroblasts
Primary culture fibroblasts were obtained from
12-day-old rat embryos (n=26). Female rats were anesthetized with
ether, and disinfected with alcohol. Under sterile conditions, the
abdomen was dissected and the uterine horns of the embryos were
removed and placed in Hank’s solution (Life Technologies)
supplemented with 100X antibiotic-antimycotic (Life Technologies).
The head, limbs and internal organs were removed from the embryos.
The remaining mass was separated into small sections using scissors
and subjected to enzymatic dissociation with 0.25% trypsin for 40
min at 37°C. Cells were precipitated by centrifugation (1,000 × g
for 5 min). The pellet was resuspended in complete medium (90%
DMEM/F12, 10% HEPES, 10% FBS, 2 mM L-glutamine, 0.8% glucose, 0.2
U/ml insulin and 10,000 U/ml antibiotic-antimycotic; Life
Technologies). The rats were provided by the Far Eastern Federal
University.
Isolation of primary cultures of rat
astrocytes
A total of 28 newborn female white rats (weight, 3–5
g) were used for the experiment. The rats were provided by the Far
Eastern Federal University. Under sterile conditions, the rats were
anesthetized, the head was separated from the body, the skull was
dissected and the brain was removed and placed in a petri dish
containing Hank’s solution. Next, the cerebral cortex was isolated
and purified from its vascular membranes, separated into small
pieces using scissors, washed twice with Hank’s solution, and
subjected to enzymatic dissociation with 0.05% trypsin-EDTA for 10
min at 37°C. Enzymatic dissociation was stopped by adding 5% FBS
(Hank’s solution), washing twice and subjecting the sections to
mechanical dissociation using the fused end of a Pasteur pipette.
The cell suspension was precipitated by centrifugation (120 × g for
3 min) and resuspended in complete medium [DMEM/F12 (90%), fetal
calf serum (10%), L-glutamine (2 mM), glucose (0.8%), insulin (0.2
U/ml) HEPES (25 mM), antibiotic-antimycotic (10,000 U/ml)].
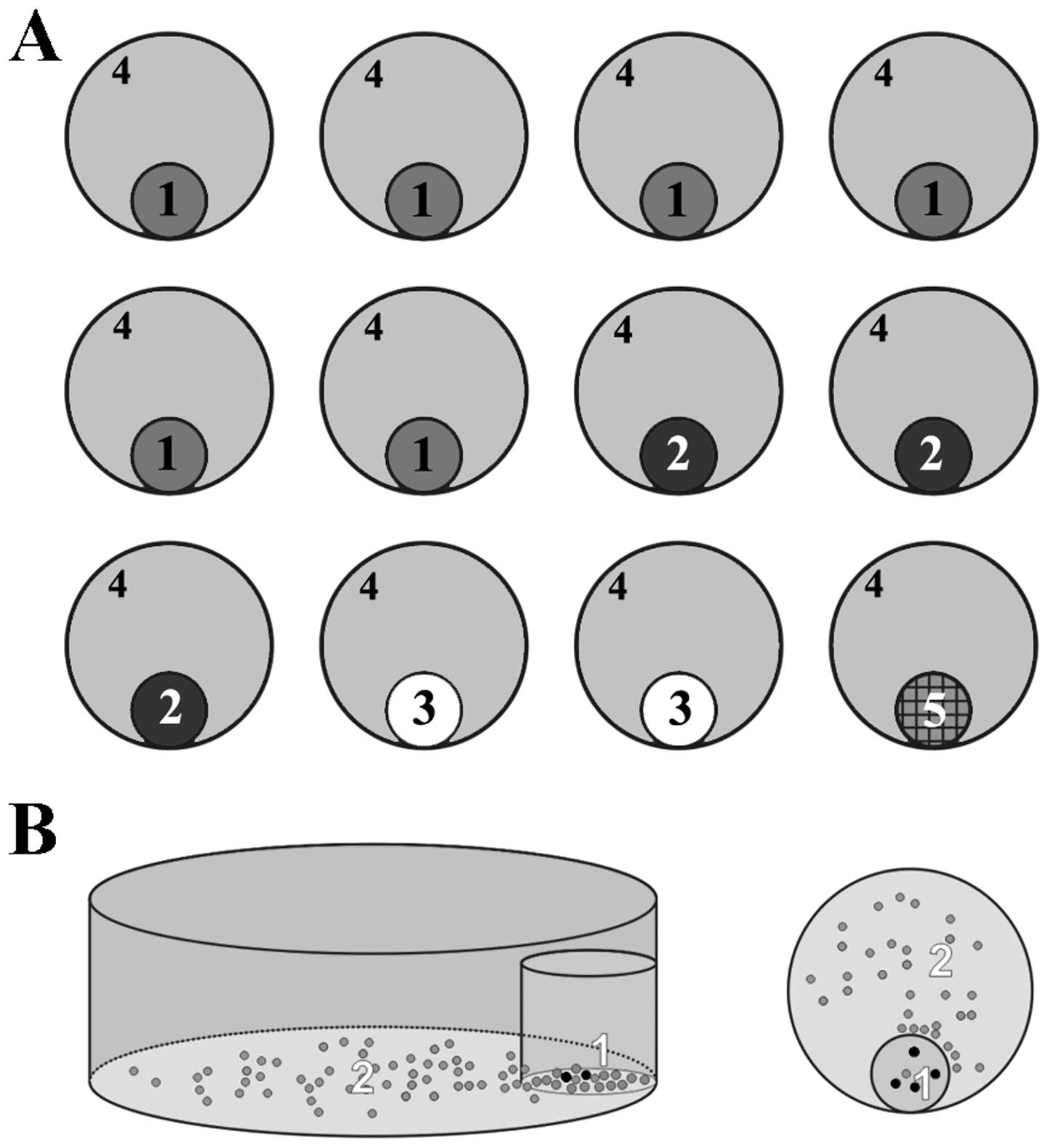
Establishment of co-cultures
Culture inserts (diameter, 12 mm; pore size, 0.4 μm;
EMD Millipore, Billerica, MA, USA), were used for the co-cultures.
The bottom of a 12-well tissue culture plate was coated with
polyethylenimine, and then with laminin (both Life Technologies).
Next, culture inserts were immobilized using a drop of sterile
paraffin, which was added to each well. A total of
0.5×106 tumor cells and normal fibroblasts and
astrocytes were added to the inside culture inserts, and one of the
inserts was left empty (Fig. 1A).
The plate with culture inserts was incubated for 24 h, then the
bottom of the wells were plated with 0.25×106
hematopoietic stem cells. Following incubation for 3 h, the
non-adherent cells from the bottom of the wells were removed. The
distribution of hematopoietic stem cells on the bottom of the wells
was analyzed visually with a confocal laser scanning microscope
(Zeiss LSM 710 META; Carl Zeiss, Jena, Germany) (Fig. 1B). Cell counts in the projection
area of the membrane culture inserts were performed using
Photo-Capt v.12.4 c 4 (Vilber Lourmat, Eberhardzell, Germany)
between the first and fifth days of culture.
Statistical analysis
Statistical analysis was performed using Statistica
6.0 software (StatSoft, Inc., Tulsa, OK, USA) and Microsoft Excel
2010 (Microsoft Corporation, Redmond, WA, USA).
Results
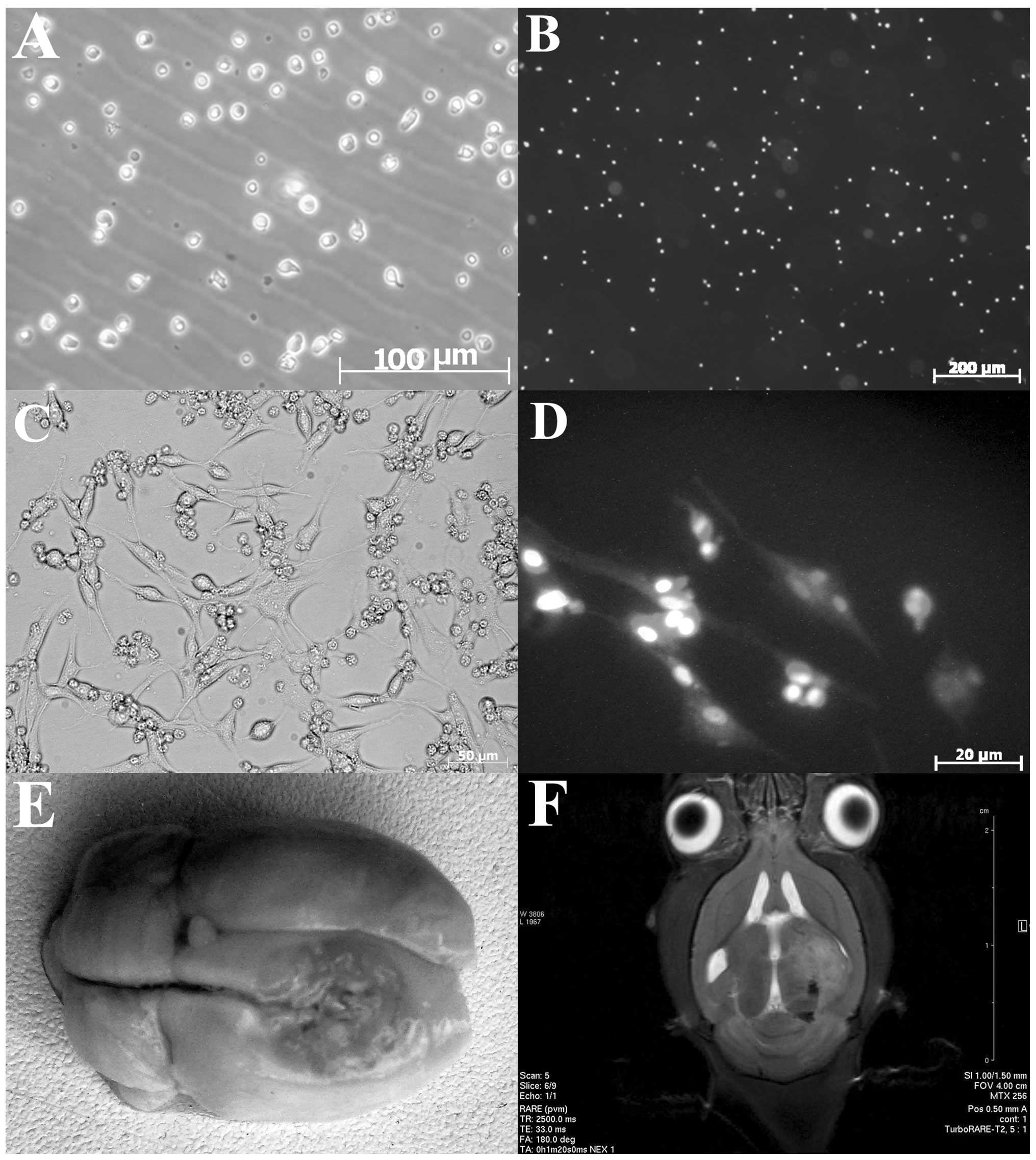
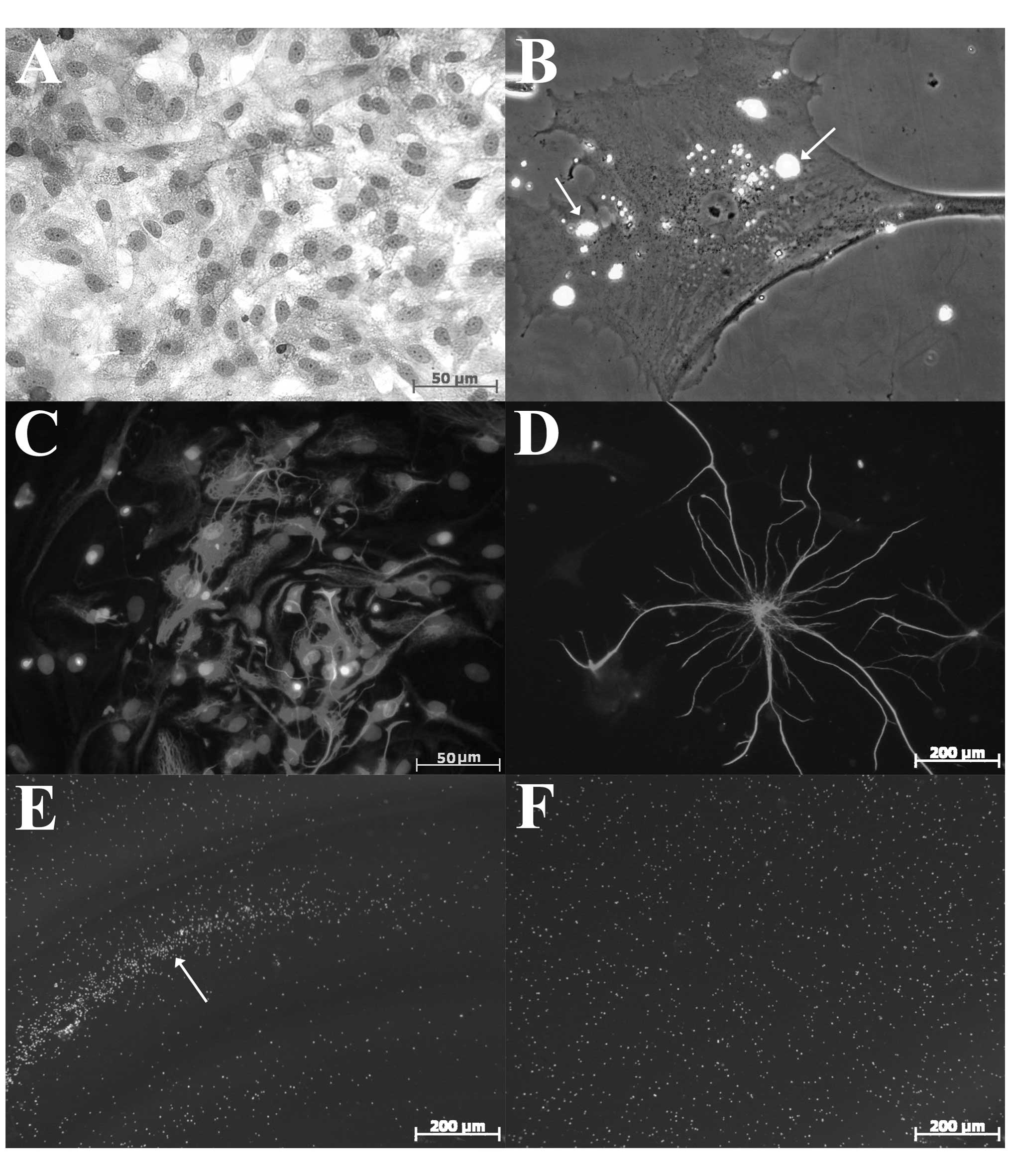
Hematopoietic stem cell culture
According to the data, the cytometry purity of the
hematopoietic stem cell CD34+/CD133+
populations was 88.9%. The cells stained with Vybrant®
CFDA SE tracer exhibited a stable fluorescence, which was observed
at low magnification (Fig. 2A and
B).
Primary culture of the C6 glioma
line
C6 glioma cell culture presented a heterogeneous
population of actively proliferating cells of different shapes and
sizes (Fig. 2C). Elongated cells
with outgrowths were clearly observed, and were surrounded by
small, round cells. Subsequent to 24 h of cultivation, a number of
cells with an astrocyte-like phenotype adhered to the bottom of the
culture inserts, while other cells formed numerous outgrowths of
different shapes and sizes. The cells were stained with monoclonal
rabbit antibodies against glial fibrillary acidic protein (GFAP)
(anti-GFAP antibody; ab33922; Abcam, Cambridge, UK). Microscopy at
low magnification (with the Zeiss LSM 710 META confocal laser
scanning microscope) and subsequent DAPI (D1306, Molecular Probes,
Eugene, OR, USA) staining allowed the visualization of numerous
neoplastic nuclei of various shapes and sizes (Fig. 2D). Stereotactic implantation of
3×104 C6 glioma cells into the brains of the adult rats
led to the development of tumors, which was accompanied by severe
asthenia, a rapid decrease in the animal’s body weight, the
development of severe edema and dislocation of brain structures,
which was confirmed by morphological data and neuroimaging studies
(Fig. 2D, E and F).
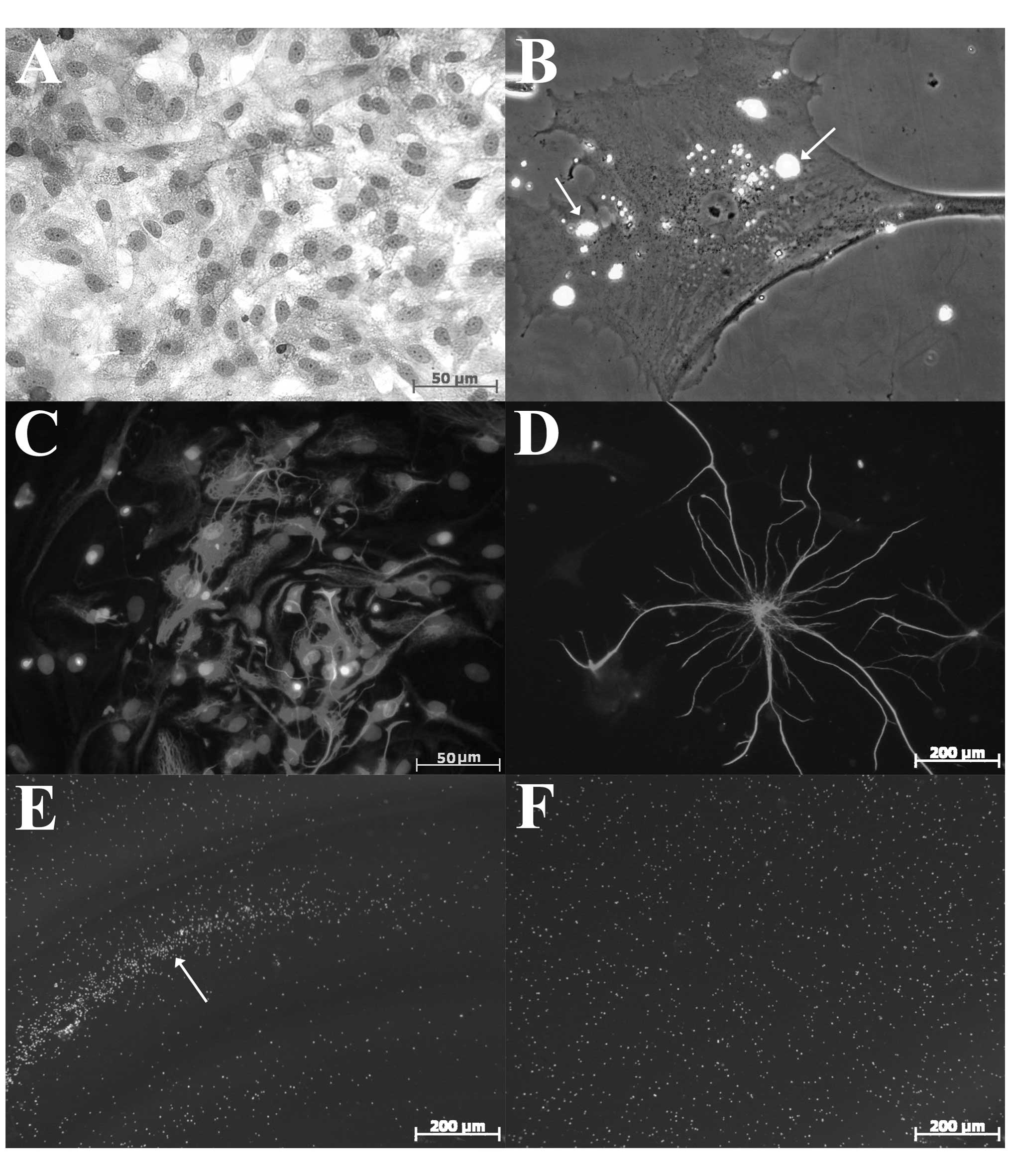
Primary culture of rat fibroblast
Hematoxylin and eosin staining of the rat
fibroblasts revealed cells of different sizes and shapes with
rounded cell nuclei (Fig. 3A).
Functional analysis of the cells conducted using
FluoSpheres® Collagen I-Labeled Microspheres (F-20892;
Life Technologies) according to the manufacturer’s instructions,
revealed active phagocytosis of collagen particles (Fig. 3B). This culture was used as the
control.
 | Figure 3Characteristics of cell lines and
control fibroblast cultures and astrocytes, and reaction of
different cell lines to co-culturing with glioma cells in the
experiment. (A) Rat fibroblasts (hematoxylin and eosin;
magnification, ×40). (B) Rat fibroblasts. Phagocytosis of collagen
immobilized on the surface of the fluorescent microparticles
FluoSpheres® Collagen I-Labeled Microspheres
(magnification, ×630). (C) Rat astrocytes stained with anti-GFAP
Mab and nuclei counterstained with DAPI (magnification, ×100). (D)
Rat astrocyte stained with anti-GFAP Mab (magnification, ×200). (E)
Formation of fluorescent cell shaft on the perimeter of culture
inserts containing glioma cells, by hematopoietic stem cells
stained with Vybrant® CFDA SE Cell Tracer
(magnification, ×10). (F) Co-culturing hematopoietic stem cells and
rat fibroblasts. The formation of the cell shaft was absent
(magnification, ×10). GFAP, glial fibrillary acidic protein; Mab,
monoclonal antibody. |
Primary cultures of rat astrocytes
Cultured rat astrocytes were stained with DAPI and
characterized using monoclonal antibodies against GFAP as a control
(Fig. 3C and D).
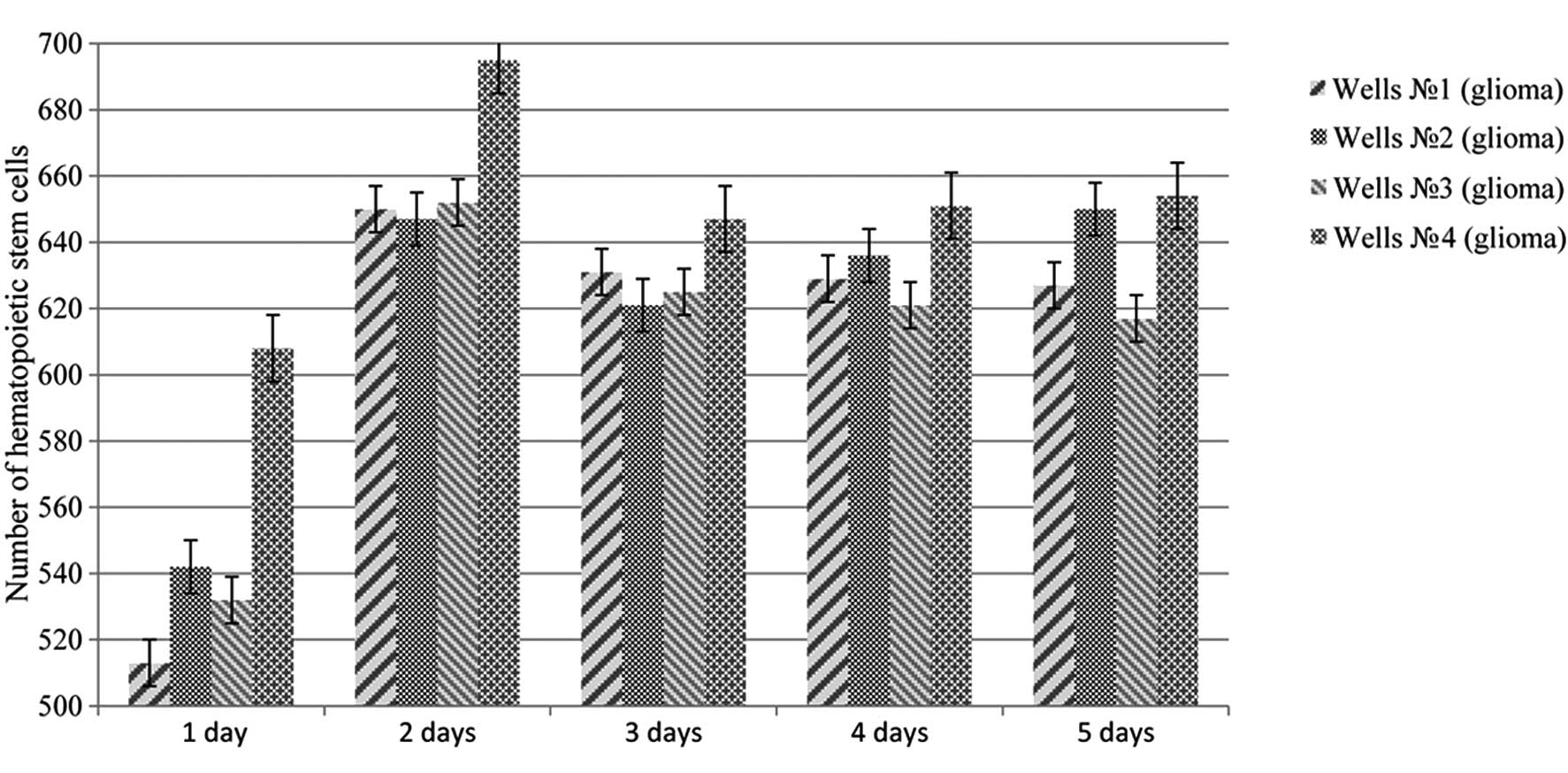
Migration of hematopoietic stem cells
co-cultured with astrocytes, fibroblasts and C6 glioma
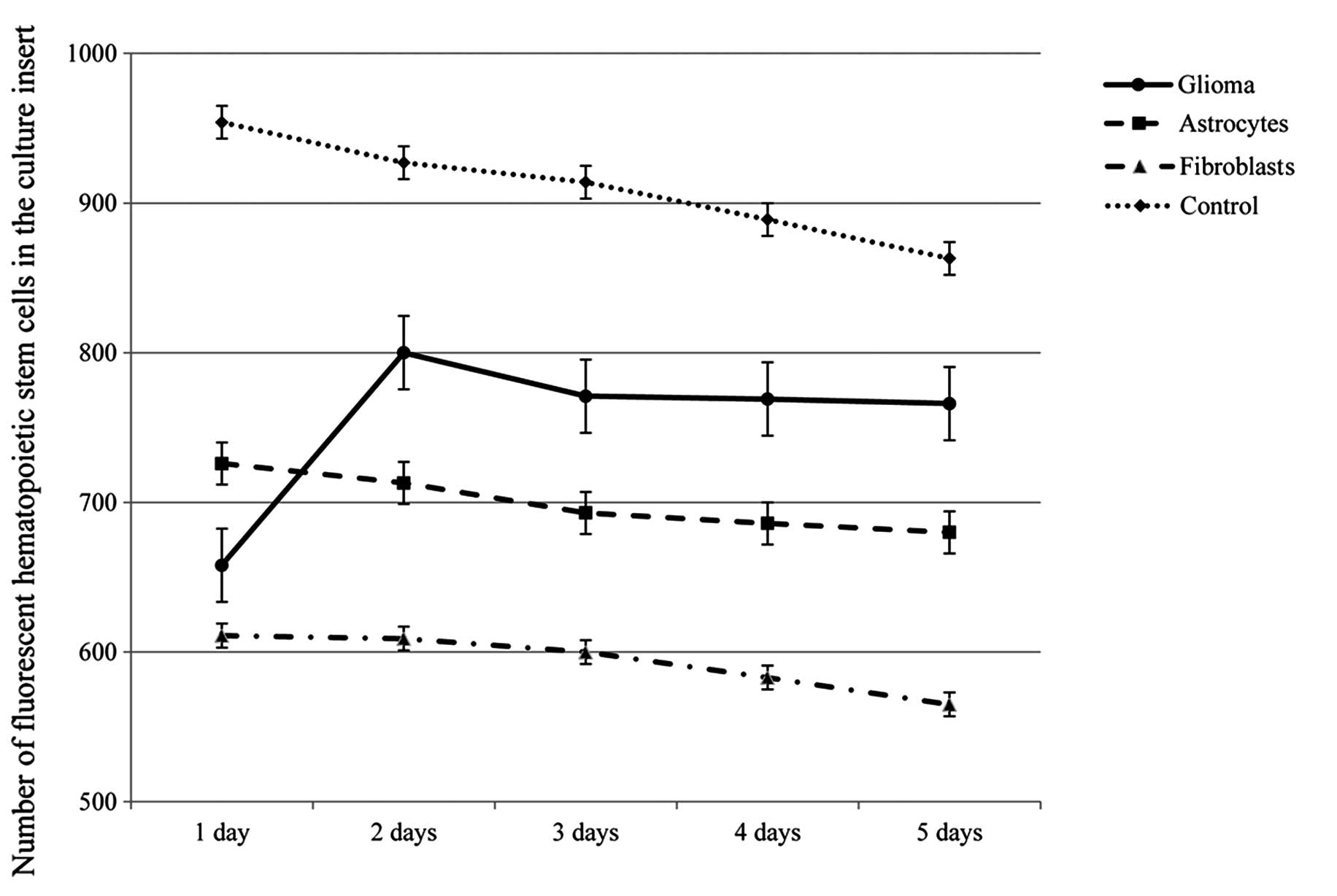
During the co-culture of the stem and tumor cells,
the formation of the cell shaft consisting of hematopoietic stem
cells, located on the perimeter of the culture insert, containing
the glioma culture (Fig. 3E) was
identified. This phenomenon, which was most significant on the
second day, was identified in all co-cultures containing glioma
cells, and absent in co-cultures containing fibroblasts and
astrocytes (Fig. 3E and F). A
fluorescent marker was used to count the cells, which showed a
significant increase (P<0.05) in the number of adult hemopoietic
progenitors in the field of the membrane in all co-cultures
containing glioma cells between the second and fifth days of the
experiment (Fig. 4). No significant
differences in the number of hematopoietic stem cells in
co-cultures with normal astrocytes and fibroblasts were identified
(Fig. 5). We hypothesized that the
directed migration of stem cells to co-cultured glioma caused the
production of various chemoattractants and cytokines by neoplastic
cells.
Discussion
Identifying the phenomenon of the directed migration
of stem cells to the area of injury, ischemic injury or neoplastic
tissue was an important step in understanding the biology of
carcinogenesis and regenerational processes in the brain of mammals
and humans. It has been found that >79 cytokines,
chemoattractants and growth factors, as well as ≥20 types of
receptors, control the migration and homing of stem cells (18,19).
The importance of stromal cell-derived factor-1α in this process
and the active participation of stem cell factor, hepatocyte growth
factor, vascular endothelial growth factor, monocyte
chemoattractant protein-1, high-mobility group box 1, urokinase
plasminogen activator, interleukin-6, the β1 and β2 integrins,
L-selectin and other ligands has been investigated (20). The main source of chemoattractants,
which attract stem cells, are damaged neurons, astrocytes,
microglia and degenerating elements of the extracellular matrix
that are released into the bloodstream. As can be observed in the
present experiment, the primary source of cytokines is tumor
tissue. The ability of neuroepithelial tumors to produce tenascin,
fibronectin, laminin, various types of collagen and other
biologically active molecules has been investigated previously
(21). In vivo, the main
source of multipotent cell elements is the mature brain germinal
zone. Tumors attract and actively recruit neural stem cells during
the mutational process, stimulating the expression of the majority
of oncogenes, and actively using their replication and migration
potential (22).
Hematopoietic stem cells and adult progenitor cells
of mammals and humans are significantly less involved in the
mutational process than neural stem cells, as evidenced by the
analysis of the proteomic profile. Furthermore, their high
regenerative potential, in combination with their ability to
maintain an association with normal nerve tissue allows their
consideration as the most promising cell line for the treatment of
the majority of neurological diseases and brain injuries (23,24).
In conclusion, the results of the present study
indicate the pathotropism of mammalian hemopoietic stem cells to C6
glioma, which represents potential for their clinical application.
However, the role of hematopoietic stem and progenitor cells in the
carcinogenesis of malignant neoplasms of the brain requires further
investigation.
Acknowledgements
This study was supported by the Ministry of Science
and Education of the Russian Federation [project no. 14.575.21.0038
(UIP RFMEF157514X0038)].
References
|
1
|
Schiff D and Purow B: Neuro-oncology: Five
new things. Neurol Clin Pract. 3:326–333. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Omuro A and DeAngelis LM: Glioblastoma and
other malignant gliomas: a clinical review. JAMA. 310:1842–1850.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yabroff KR, Harlan L, Zeruto C, Abrams J
and Mann B: Patterns of care and survival for patients with
glioblastoma multiforme diagnosed during 2006. Neuro Oncol.
14:351–359. PubMed/NCBI
|
|
4
|
Hayashi Y, Nakada M, Kinoshita M and
Hamada J: Surgical strategies for nonenhancing slow-growing gliomas
with special reference to functional reorganization: review with
own experience. Neurol Med Chir (Tokyo). 53:438–446. 2013.
View Article : Google Scholar
|
|
5
|
Aboody KS, Brown A, Rainov NG, Bower KA,
Liu S, Yang W, Small JE, Herrlinger U, Ourednik V, Black PM, et al:
Neural stem cells display extensive tropism for pathology in adult
brain: evidence from intracranial gliomas. Proc Natl Acad Sci USA.
97:12846–12851. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhao D, Najbauer J, Annala AJ, Garcia E,
Metz MZ, Gutova M, Polewski MD, Gilchrist M, Glackin CA, Kim SU and
Aboody KS: Human neural stem cell tropism to metastatic breast
cancer. Stem Cells. 30:314–325. 2012. View
Article : Google Scholar
|
|
7
|
Gutova M, Shackleford GM, Khankaldyyan V,
Herrmann KA, Shi XH, Mittelholtz K, Abramyants Y, Blanchard MS, Kim
SU, Annala AJ, et al: Neural stem cell-mediated CE/CPT-11
enzyme/prodrug therapy in transgenic mouse model of intracerebellar
medulloblastoma. Gene Ther. 20:143–150. 2013. View Article : Google Scholar
|
|
8
|
Frank RT, Najbauer J and Aboody KS:
Concise review: stem cells as an emerging platform for antibody
therapy of cancer. Stem Cells. 28:2084–2087. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tabatabai G and Weller M: Glioblastoma
stem cells. Cell Tissue Res. 343:459–465. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Soltanian S and Matin MM: Cancer stem
cells and cancer therapy. Tumour Biol. 32:425–440. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Holland EC, Celestino J, Dai C, Schaefer
L, Sawaya RE and Fuller GN: Combined activation of Ras and Akt in
neural progenitors induces glioblastoma formation in mice. Nat
Genet. 25:55–57. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Alexiou GA, Vartholomatos G, Karamoutsios
A, Batistatou A, Kyritsis AP and Voulgaris S: Circulating
progenitor cells: a comparison of patients with glioblastoma or
meningioma. Acta Neurol Belg. 113:7–11. 2013. View Article : Google Scholar
|
|
13
|
Grobben B, De Deyn PP and Slegers H: Rat
C6 glioma as experimental model system for the study of
glioblastoma growth and invasion. Cell Tissue Res. 310:257–270.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goffart N, Kroonen J and Rogister B:
Glioblastoma-initiating cells: relationship with neural stem cells
and the micro-environment. Cancers (Basel). 5:1049–1071. 2013.
View Article : Google Scholar
|
|
15
|
Zhao D, Najbauer J, Garcia E, Metz MZ,
Gutova M, Glackin CA, Kim SU and Aboody KS: Neural stem cell
tropism to glioma: critical role of tumor hypoxia. Mol Cancer Res.
6:1819–1829. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Barth RF and Kaur B: Rat brain tumor
models in experimental neuro-oncology: the C6, 9L, T9, RG2, F98,
BT4C, RT-2 and CNS-1 gliomas. J Neurooncol. 94:299–312. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cheng M and Qin G: Progenitor cell
mobilization and recruitment: SDF-1, CXCR4, α4-integrin, and c-kit.
Prog Mol Biol Transl Sci. 111:243–264. 2012. View Article : Google Scholar
|
|
18
|
Heese O, Disko A, Zircel D, et al: Neural
stem cell migration toward gliomas in vivo. Neuro Oncol. 7:476–484.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bajeto A, Barbieri F, Dorcaratto A, et al:
Expression of CXC chemokine receptors 1–5 and their ligands in
human glioma tissues: role of CXCR4 and SDF1 in glioma cell
proliferation and migration. Neurochem Int. 49:423–432. 2006.
View Article : Google Scholar
|
|
20
|
Cheng M, Zhou J, Wu M, Boriboun C, Thorne
T, Liu T, Xiang Z, Zeng Q, Tanaka T, Tang YL, et al: CXCR4-mediated
bone marrow progenitor cell maintenance and mobilization a
modulated by c-kit activity. Circ Res. 107:1083–1093. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kang R, Zhang Q, Zeh HJ III, Lotze MT and
Tang D: HMGB1 in cancer: good, bad or both? Clin Cancer Res.
19:4046–4057. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yin D, Zhang Z, Gao S and Li B: The role
of chemokine receptor CXCR4 and its ligand CXCL12 in the process of
proliferation and migration of oral squamous cell carcinoma. Hua Xi
Kou Qiang Yi Xue Za Zhi. 31:8–12. 2013.(In Chinese). PubMed/NCBI
|
|
23
|
Zheng H, Ying H, Yan H, Kimmelman AC,
Hiller DJ, Chen AJ, Perry SR, Tonon G, Chu GC, Ding Z, et al: p53
and Pten control neural and glioma stem/progenitor cell renewal and
differentiation. Nature. 455:1129–1133. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Greenbaum A, Hsu YM, Day RB, Schuettpelz
LG, Christopher MJ, Borgerding JN, Nagasawa T and Link DC: CXCL12
in early mesenchymal progenitors is required for hematopoietic
stem-cell maintenance. Nature. 495:227–230. 2013. View Article : Google Scholar : PubMed/NCBI
|