Introduction
Thymic epithelial tumors are a rare form of neoplasm
consisting of two primary histological types: Thymoma and thymic
carcinomas (1). The lesions form a
rare category of heterogeneous lesions, presenting with a large
range of pathological and clinical characteristics. Thymomas are
the most frequently diagnosed primary anterior mediastinal tumors,
with an incidence of 1.5 cases per million individuals (2). Although thymic carcinomas are rarer
than thymomas, they are more invasive and have a poorer prognosis.
The five-year survival rates for all stages of thymoma and thymic
carcinomas are 78 and 40%, respectively (3–5).
Surgical resection, followed by radiation therapy,
are the preferred treatments for all subtypes of thymic carcinoma
without distant metastasis. Patients with unresectable tumors or
metastasis, however, are treated with systemic chemotherapy. Due to
the rarity of the disease, a standard chemotherapy regimen for
thymic carcinoma is yet to be established (6).
The present study describes a 63-year-old female
with thymic carcinoma who underwent a range of antitumor
treatments, including surgical resection, post-operative
radiotherapy, post-operative chemotherapy with
gemcitabine-carboplatin (GC) and gemcitabine-cisplatin (GP),
second-line chemotherapy with docetaxel and cisplatin (DP)
following relapse, tyrosine kinase inhibitor (TKI) treatment, and
finally chemotherapy with nab-paclitaxel (nab-P) and nedaplatin.
The patient demonstrated a good response to nab-P and remains alive
three years post-treatment. Written informed consent was obtained
from the patient.
Case report
In August 2011, a 63-year-old female underwent
thoracic computed tomography (CT) and was diagnosed with a mass in
the upper right mediastinum that measured 7.5×7 cm and was in close
proximity to the superior vena cava (Fig. 1A). The patient did not present with
any respiratory symptoms, such as a cough or chest pain. Complete
resection of the tumor was performed under general anesthetic in
September 2011 (Fig. 1B). During
surgery, tumor cell invasion into the superior vena cava and left
innominate vein, and pericardial adhesion were observed. The
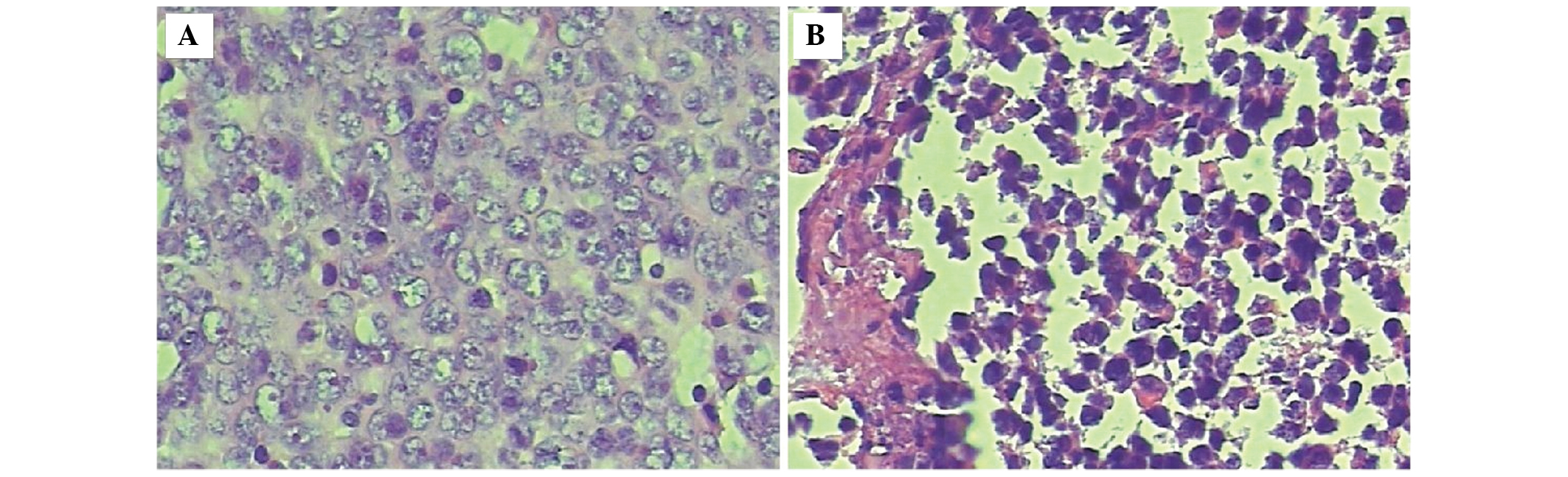
pathological evidence established a diagnosis of thymic squamous
cell carcinoma (Fig. 2A), with
positive lymph nodes under the clavicle. Treatment with GP (1.4 mg
gemcitabine, days 1 and 8; 100 mg cisplatin, day 1; one cycle
lasting 21 days) and GC (1.4 mg gemcitabine, days 1 and 8; 400 mg
carboplatin, day 1; three cycles lasting 63 days). Subsequent to
chemotherapy, the patient received post-operative radiotherapy to
the mediastinum with a total dosage of 56 Gy (2 Gy/day over 28
days).
At the follow-up visit, the patient had no
discomfort and the disease had not progressed. However, in late
February 2013, thoracic CT revealed several unequal nodules in the
right lung and under the pleura. The disease had recurred following
18 months of progression-free survival. Subsequent to two cycles of
chemotherapy with DP (docetaxel, 100 mg on day 1; cisplatin, 100 mg
on day 1 for two cycles lasting 42 days), the patient was
reexamined. This time, thoracic CT revealed the presence of
metastatic lesions in the right lung, which were larger than those
previously observed and were considered unsuitable for DP therapy.
Paraffin-embedded sections of the thymic carcinoma were then
analyzed for the 18–21 mutation of the EGFR gene. The results of
the amplification refractory mutation system (ARMS) revealed a
mutation in L858R of exon 21. The patient was administered
gefitinib and a month later was reexamined by thoracic CT. The
results indicated progression of the lesion and so treatment was
stopped. During the three-month, drug-free observation period, the
metastatic lesion in the right lung significantly progressed
(Fig. 3A). Furthermore, right-sided
pleural effusion, evidence of peritoneal metastasis (Fig. 3B), and symptoms of chest distress
and shortness of breath were evident. On August 16, 2013, a
percutaneous intrathoracic lung biopsy was performed following a CT
scan. The pathological evidence indicated the presence of squamous
cell carcinoma, which had originated from the same source as the
thymic squamous cell carcinoma (Fig.
2B). In addition, tissues obtained from the lung biopsy were
analyzed, but no mutations in the EGFR gene, ALK fusion gene or KIT
gene were revealed. At the beginning of September 2013, six cycles
of a chemotherapy regimen were initiated, consisting of nab-P and
nedaplatin, (nab-P 200 mg on days 1 and 8; nedaplatin 30 mg on days
1–3). Following treatment, the pleural effusion significantly
decreased, the lesion in right lung remained stable (Fig. 3C) and the metastatic lesions in the
peritoneum were reduced in size (Fig.
3D). The patient demonstrated a good response to nab-P and
remains alive three years post-treatment.
Discussion
Thymic carcinoma is a rare cancer with a poor
outcome, as it is usually discovered at an advanced stage. Due to
its rarity, the optimal treatment regimen for patients with thymic
carcinoma is uncertain. Several aggressive, multimodal treatment
strategies have been advocated, but future prospective studies with
larger numbers of patients are required in order to validate the
most effective therapeutic approach (1–3).
Surgical resection is the preferred curative
treatment for thymic tumors, with complete resection conferring the
most favorable clinical prognosis (7). At diagnosis, almost 30% of patients
present with a locally-advanced tumor, dissemination to the pleura
and the pericardium, and/or invasion of adjacent intrathoracic
components. Resection of the tumor is usually achieved through a
median sternotomy, with removal of the thymus and all adjoining
mediastinal fat bordered laterally by the phrenic nerves (8).
Due to the rarity of thymic malignancies, knowledge
concerning the outcomes of chemotherapy on these lesions has been
based upon retrospective studies, the majority of which are
outdated. Furthermore, only a limited number of prospective studies
have ever been conducted. The National Comprehensive Cancer Network
2013 guideline on thymomas and thymic carcinomas recommends that
first-line treatment should include a cisplatin, doxorubicin and
cyclophosphamide (CAP) regimen, a CAP with prednisone, cisplatin,
doxorubicin, vincristine and cyclophosphamide regimen, a cisplatin
and etoposide regimen, an etoposide, ifosfamide and cisplatin
regimen, or a carboplatin and paclitaxel (PC) regimen (9). Second-line chemotherapy is suggested
to include etoposide, ifosfamide, pemetrexed, octreotide,
prednisone, 5-fluorouracil and leucovorin, gemcitabine or
paclitaxel.
In 2011, Lemma et al (10) conducted a prospective multicenter
study in order to investigate the impact of the PC regimen in
patients with advanced and previously untreated thymic carcinoma.
The study included 23 patients with thymic carcinoma. Non of the
patients were in complete remission, five exhibited partial
responses and 12 experienced stable disease. The mean
progression-free survival time was five months and the median
survival time was 20 months. The PC regimen has moderate clinical
activity in patients with thymic malignancies, but this appears to
be less than expected when compared with anthracycline-based
therapy.
In the last ten years, there have been six studies
(11–16) that have reported gene mutations in
thymic carcinomas, including those in EGFR exons 18–21, HER-2 exons
19–20, Kras exon 2 and KIT exons 9, 11, 13 and 17. The results of
these studies revealed that thymic carcinoma gene mutations are
rare. A 2008 study tested for the presence of EGFR and KIT gene
mutations by direct sequencing in nine and 11 different thymic
cancer tissues, respectively (14).
One mutation was identified in exon 11 of the KIT gene, but none in
the EGFR gene. Another study, which analyzed 48 cases of thymic
carcinoma, identified only six that contained KIT gene mutations:
Four within exon 11 (V559A, L576P, Y553 N, W557R), one within exon
9 (E490 K) and one within exon 17 (D820E) (15). Targeted molecular therapy, for
example, with the TKI sunitinib, is a new paradigm in the treatment
of cancer, which may be useful for patients with thymic carcinoma.
However, there have only been three case studies to date describing
the success of sorafenib and sunitinib against thymic carcinoma
(15,17,18).
In the present study, an L858R mutation in exon 21 of the EGFR gene
was identified in the tissue of the thymic carcinoma, but the
patient did not respond to treatment with TKIs. Furthermore, no
mutations were identified in the EGFR, ALK fusion or KIT genes in
the metastatic tissues of the lung. Therefore, it was concluded
that the EGFR exon 21 L858R mutation in the thymic carcinoma tissue
was likely to be a false-positive ARMS result.
Nab-P (also known as Abraxane®) has a
mean particle size of 130 nm and was originally manufactured with
the aim of improving the therapeutic index of paclitaxel (19). In a previous study, nab-P
demonstrated a 10-fold increase in the mean concentration of free
paclitaxel in the serum compared with solvent-based-paclitaxel
(sb-P) alone (19). Nab-P, alone or
in combination with carboplatin (nab-P/C), has exhibited positive
outcomes in two phase III clinical trials that compared nab-P/C
with sb-P plus carboplatin as a first-line treatment for cases of
advanced NSCLC (20,21). As a result of these findings, the
U.S. Food and Drug Administration approved nab-P/C as a first-line
treatment for locally-advanced or metastatic disease in NSCLC
patients unsuitable for radiation therapy or curative surgery
(19).
To the best of our knowledge, the present study is
the first to describe the positive response of a patient with
thymic carcinoma to nab-P chemotherapy. As the number of effective
treatment options for thymic carcinoma is small, a controlled
trial, in which nab-P is analyzed for its clinical efficacy, is
required in the future.
Acknowledgements
This study was supported by grants from the
‘Twelve-Five Plan’ of the Major Program of Nanjing Medical Science
and Technique Development Foundation (Molecular Mechanism Study on
Metastasis and Clinical Efficacy Prediction of Non-small Cell Lung
Cancer) and Third Level Training Program of Young Talent Project of
Nanjing Health (no. QRX11226), the Nanjing Medical Science and
Technology Development Project (no. YKK12127), and the Young
Professionals Foundation of Nanjing Chest Hospital.
References
|
1
|
Ströbel P, Marx A, Zettl A and
Müller-Hermelink HK: Thymoma and thymic carcinoma: an update of the
WHO Classification 2004. Surg Today. 35:805–811. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Engels EA: Epidemiology of thymoma and
associated malignancies. J Thorac Oncol. 5(Suppl 4): S260–S265.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
No authors listed. Proceedings of the
First International Conference on Thymic Malignancies; August
20–21, 2009; Bethesda, Maryland, USA. J Thorac Oncol. 5(Suppl 4):
pp. S259–S370. 2010
|
|
4
|
Kondo K and Monden Y: Therapy for thymic
epithelial tumors: a clinical study of 1,320 patients from Japan.
Ann Thorac Surg. 76:878–885. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Masaoka A, Yamakawa Y, Niwa H, et al:
Thymectomy and malignancy. Eur J Cardiothorac Surg. 8:251–253.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ströbel P, Bauer A, Puppe B, et al: Tumor
recurrence and survival in patients treated for thymomas and thymic
squamous cell carcinomas: a retrospective analysis. J Clin Oncol.
22:1501–1509. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Girard N, Mornex F, Van Houtte P, Cordier
JF and van Schil P: Thymoma: a focus on current therapeutic
management. J Thorac Oncol. 4:119–126. 2009. View Article : Google Scholar
|
|
8
|
Rashid OM, Cassano AD and Takabe K: Thymic
neoplasm: a rare disease with a complex clinical presentation. J
Thorac Dis. 5:173–183. 2013.PubMed/NCBI
|
|
9
|
NCCN Guidelines on the Treatment of
Thymomas and Thymic Carsinomas. http://www.nccn.org/professionals/physician_gls/pdf/thymic.pdf.
Accessed May 18, 2014
|
|
10
|
Lemma GL, Lee JW, Aisner SC, et al: Phase
II study of carboplatin and paclitaxel in advanced thymoma and
thymic carcinoma. J Clin Oncol. 29:2060–2065. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pan CC, Chen PC and Chiang H: KIT (CD117)
is frequently overexpressed in thymic carcinomas but is absent in
thymomas. J Pathol. 202:375–381. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Suzuki M, Chen H, Shigematsu H, et al:
Aberrant methylation: common in thymic carcinomas, rare in
thymomas. Oncol Rep. 14:1621–1624. 2005.PubMed/NCBI
|
|
13
|
Girard N, Shen R, Guo T, et al:
Comprehensive genomic analysis reveals clinically relevant
molecular distinctions between thymic carcinomas and thymomas. Clin
Cancer Res. 15:6790–6799. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yoh K, Nishiwaki Y, Ishii G, et al:
Mutational status of EGFR and KIT in thymoma and thymic carcinoma.
Lung Cancer. 62:316–320. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ströbel P, Bargou R, Wolff A, et al:
Sunitinib in metastatic thymic carcinomas: laboratory findings and
initial clinical experience. Br J Cancer. 103:196–200. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schirosi L, Nannini N, Nicoli D, et al:
Activating c-KIT mutations in a subset of thymic carcinoma and
response to different c-KIT inhibitors. Ann Oncol. 23:2409–2414.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bisagni G, Rossi G, Cavazza A, et al: Long
lasting response to the multikinase inhibitor bay 43–9006
(Sorafenib) in a heavily pretreated metastatic thymic carcinoma. J
Thorac Oncol. 4:773–775. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li XF, Chen Q, Huang WX and Ye YB:
Response to sorafenib in cisplatin-resistant thymic carcinoma: a
case report. Med Oncol. 26:157–160. 2009. View Article : Google Scholar
|
|
19
|
Gardner ER, Dahut WL, Scripture CD, et al:
Randomized crossover pharmacokinetic study of solvent-based
paclitaxel and nab-paclitaxel. Clin Cancer Res. 14:4200–4205. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Socinski MA, Langer CJ, Okamoto I, et al:
Safety and efficacy of weekly nab®-paclitaxel in combination with
carboplatin as first-line therapy in elderly patients with advanced
non-small-cell lung cancer. Ann Oncol. 24:314–321. 2013. View Article : Google Scholar
|
|
21
|
Socinski MA, Bondarenko I, Karaseva NA, et
al: Weekly nab-paclitaxel in combination with carboplatin versus
solvent-based paclitaxel plus carboplatin as first-line therapy in
patients with advanced non-small-cell lung cancer: final results of
a phase III trial. J Clin Oncol. 30:2055–2062. 2012. View Article : Google Scholar : PubMed/NCBI
|