Introduction
Primary central nervous system lymphoma (PCNSL) is a
rare hematopoetic tumor, which accounts for <1% of all brain
tumors, that arises within and is limited to the central nervous
system (1). The incidence rate of
PCNSL is <5 cases per 1 million people, this incidence appears
to be increasing (2,3) An important risk factor for PCNSL is an
alteration of the function of the immune system, and HIV infection
is a powerful risk factor for acquiring PCNSL (2). The outcome of PCNSL remains
unsatisfactory with a survival of <20–30% after 5 years and a
median survival of 10–20 months (3). The disease is highly malignant and may
rapidly lead to mortality if diagnosis and treatment are delayed
(1,4). The clinical manifestation of PCNSL is
variable; patients typically exhibit cognitive decline and
headaches (5,6) and may present with psychiatric
symptoms in combination with focal neurological deficits, including
aphasia, hemiparesis and ataxia (7). Although the majority of patients
respond to radiotherapy, relapse is almost inevitable (4). Chemotherapy is applied for the
treatment of relapse after radiotherapy, however, in elderly
patients a high risk of treatment-related complications exists
(6).
The present study reports the case of a 58-year-old
patient with a history of major depressive disorder (MDD) and
coexisting rheumatoid arthritis, who presented with recurrent
depressive disorder, fatigue, dizziness, vomiting and a staggering
gait. Written informed consent was obtained from the patient.
Case report
In March 2012, a 58-year-old male was referred to
the inpatient psychiatric service of the Second Affiliated Hospital
of Zhejiang University School of Medicine (Hangzhou, China) with
depressive symptoms. Six years previously, January 2006, the
patient had been diagnosed with major depressive disorder (MDD),
which had improved through treatment with fluoxetine. Subsequently,
MDD recurred twice (August 2007 and February 2009), each ocassion
lasting for two months, and a favorable response to fluoxetine (20
mg/day) was exhibited. The patient had ceased fluoxetine treatment
voluntarily two years prior to the current admission (January
2010), due to full recovery from depression. However, four months
prior to this admission (December 2011), further fluoxetine
treatment (20 mg/day) was prescribed by a local psychiatric clinic
after the patient presented with depressed mood and anhedonia. One
month later, the patient complained of unimproved depression,
fatigue and occasional vomiting, and was prescribed an increased
dosage of fluoxetine (40 mg/day); however, the patient also
experienced dizziness concurrent with the depressive symptoms. In
addition, the patient been diagnosed with rheumatoid arthritis, for
which methotrexate (10 mg once a week) and celecoxib (200 mg/day)
were administered intermittently for two years; the patient’s
symptoms fluctuated during this time.
The neurological examination showed staggering gait
with normal motor strength of the extremities. No cerebellar
ataxia, peripheral neuropathy or positive Babinski reflexes were
observed. A mental status examination revealed depressed mood with
suicidal ideation, psychomotor retardation and lack of energy. The
patient exhibited fatigue and mental dullness during the
examination. Psychological testing indicated severe depression,
with a score of 29 on the 17-item Hamilton Rating Scale for
Depression (8), and cognitive
impairment, with a Mini Mental State Examination (9) score of 20/30.
The initial diagnosis was recurrent depressive
disorder, however, a thorough physical examination was conducted to
exclude the possibility of somatic or neurological origin. Blood
analysis including hemocytology, liver and kidney function,
antinuclear antibodies and thyroid hormone were all within the
normal ranges. However, rheumatoid factor (66.8 IU/ml; normal
range, 0–25 IU/ml), C-reactive protein (30.8 mg/l; normal range,
0–10 mg/l) and cyclic citrullinated peptide (800 IU/ml; normal
range, 0–25 IU/ml) were shown to be elevated. The serum toxicology
screen, human immunodeficiency and serum syphilis antibody tests
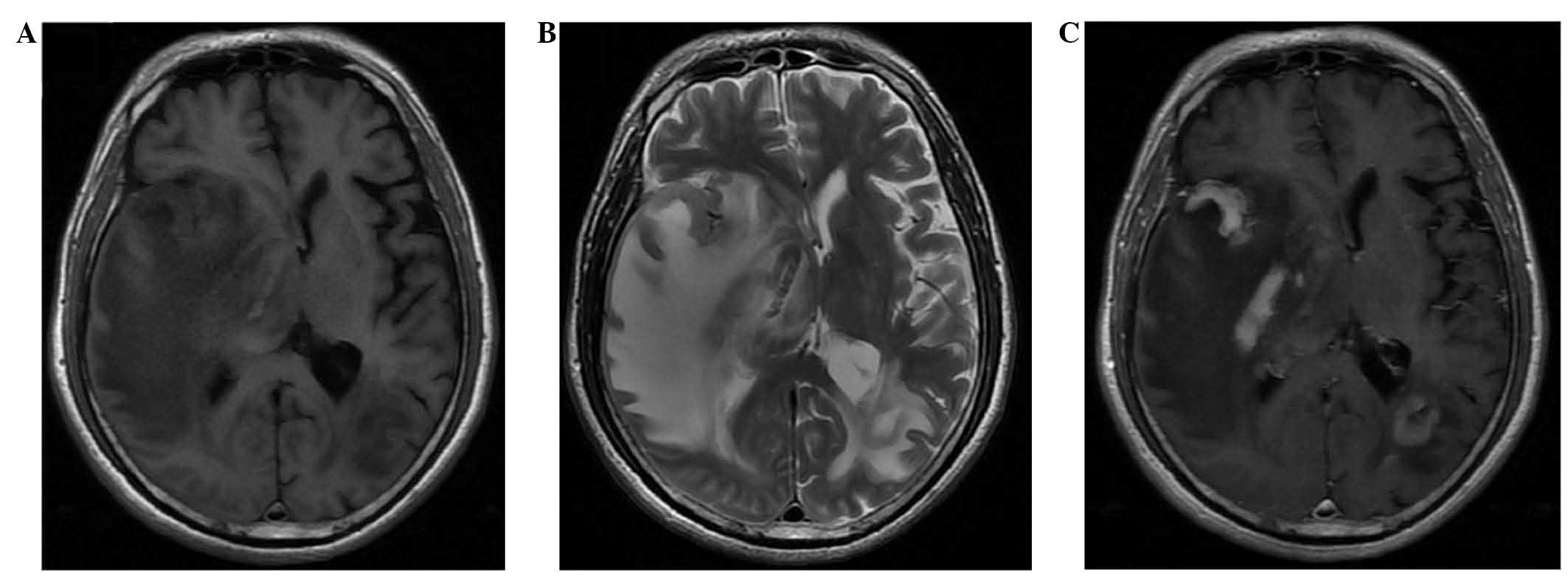
were negative. Magnetic resonance imaging (MRI) of the brain
revealed multiple lesions with marked edema in the temporal,
parietal and occipital lobes (Fig.
1).
These findings indicated the presence of brain
tumors, and the patient was transferred to the inpatient
neurosurgical service. Fluoxetine treatment was discontinued, and a
craniotomy was conducted for open biopsy and resection of the
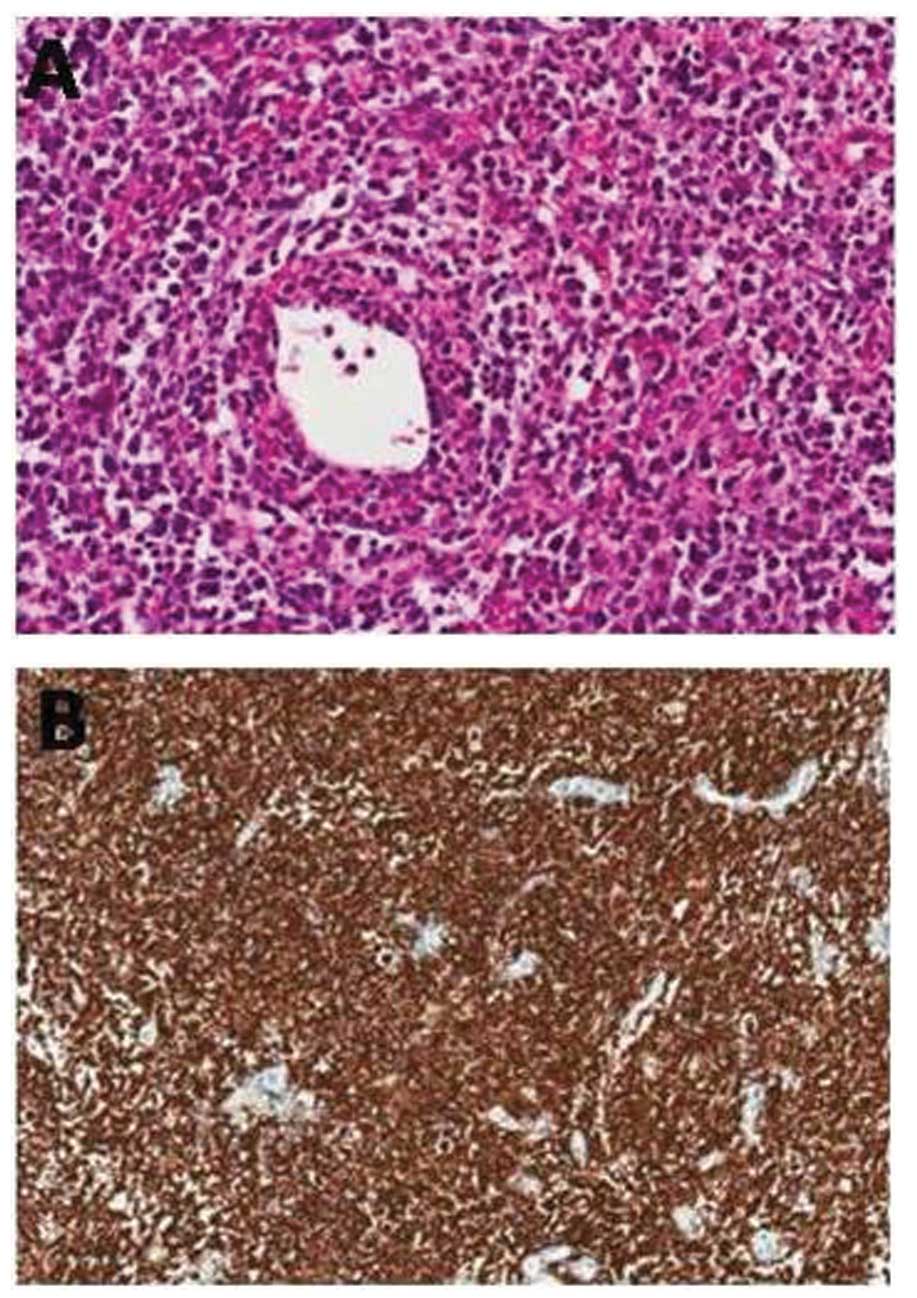
temporal lobe lesion. A pathological examination of the biopsy
specimen confirmed the diagnosis of diffuse large B cell lymphoma,
and immunohistochemical staining revealed that the tumor cells were
positive for CD20 and bcl-6 and negative for CD3 and Epstein-Barr
virus (EBV)-EBV-encoded non-polyadenylated RNA (Fig. 2). A positron emission tomography
scan was negative for systemic lymphoma, and a slit lamp
examination revealed no evidence of ocular lymphoma. Therefore, a
final diagnosis of PCNSL was determined. The patient received whole
brain radiotherapy (45 Gy total, administered in 21 fractions, five
times a week) following surgery. During the one year follow-up, no
clinical or radiographic evidence of PCNSL recurrence was observed,
and the patient’s mental state was stable without antidepressant
therapy. No recurrence or worsening of MDD has been observed to
date.
Discussion
PCNSL is a highly malignant disease which may
rapidly lead to mortality if diagnosis and treatment are not
immediately administered (1,4). A
variety of clinical manifestations may be observed in PCNSL
patients, including psychiatric symptoms in combination with focal
neurological deficits (7,10,11).
One study found that 43% of patients presented with
neuropsychiatric symptoms during the course of PCNSL (7). However, a number of studies have
reported psychiatric symptoms as the initial and dominating
presentation in PCNSL. Melinz et al (12) reported a PCNSL patient presenting
with mania, whilst Fisher et al (13) reported PCNSL involving the limbic
system, presenting with depression and intermittent vomiting.
The present study describes a case of PCNSL
mimicking recurrent depressive disorder in a 58-year-old male with
a past history of MDD; the psychiatric symptoms of PCNSL were
difficult to distinguish from common psychiatric disorder, and
therefore delayed the diagnosis. However, other symptoms, including
fatigue, dizziness, vomiting and a staggering gait indicated that
the initial diagnosis of MDD recurrence may be incorrect. These
symptoms, concurrent with the lack of response to antidepressant
drugs that had previously been an effective treatment in this
patient, suggested the possibility of another medical
condition.
As with all masses in the CNS, the location of PCNSL
lesions determines the clinical presentation (7). The neuropsychological changes appear
to be associated with diffuse involvement of the periventricular
white matter or the corpus callosum by a tumor (14). In the current study, MRI revealed
that the tumor had invaded a number of brain regions, primarily
located in the temporal, parietal and occipital lobes. As the
temporal lobe is a part of the limbic system, which is involved in
regulating emotion (15), it is
possible that the infiltration of the tumor into the temporal lobe
may have caused the recurrent depressive symptoms in this case.
An important risk factor for PCNSL is an alteration
of the function of the immune system; however, PCNSL may occur in
immunocompetent or immunocompromised patients (16,17).
Long-term immunosuppressive therapy or an underlying disease with
associated immunosuppression are high-level risk factors for PCNSL
(10). In the present study, the
patient suffered from active rheumatoid arthritis, for which he was
treated with an immunosuppressant over a period of two years. Drug-
or disease-induced immunosuppression may increase the risk of
developing PCNSL. Therefore, the possibility of PCNSL must be
considered when assessing patients with depressive symptoms who
have coexisting immunosuppressive conditions or are receiving
immunosuppressive therapies. Vigilance is essential during
diagnostic evaluation and a thorough examination for signs of
physical disorder must be conducted. In particular, MRI of the
brain is useful for the detection of PCNSL presenting with initial
psychiatric symptoms.
In conclusion, the present case demonstrates that
PCNSL may affect mood in the early stages, and patients may present
with depression as the initial and dominating symptom. Brain MRI is
a useful adjuvant examination for the detection of depression that
is caused by other physical disorders, and must be used in patients
with the clinical manifestation of MDD who have coexisting
immunosuppressive conditions, to allow for the early detection of
PCNSL and an improved prognosis.
References
|
1
|
DeAngelis LM: Brain tumors. N Engl J Med.
344:114–123. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Olson JE, Janney CA, Rao RD, Cerhan JR,
Kurtin PJ, Schiff D, Kaplan RS and O’Neill BP: The continuing
increase in the incidence of primary central nervous system
non-Hodgkin lymphoma: a surveillance, epidemiology, and end results
analysis. Cancer. 95:1504–1510. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ferreri AJ and Marturano E: Primary CNS
lymphoma. Best Pract Res Clin Haematol. 25:119–130. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gocmen S, Gamsizkan M, Onguru O, Sefali M
and Erdogan E: Primary dural lymphoma mimicking a subdural
hematoma. J Clin Neurosci. 17:380–382. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gelabert-González M, Castro Bouzas D,
Serramito-García R, Frieiro Dantas C and Aran Echabe E: Primary
central nervous system lymphoma. Neurologia. 28:283–293. 2013.
View Article : Google Scholar
|
|
6
|
O’Brien PC and Seymour JF: Progress in
primary CNS lymphoma. Lancet. 374:1477–1478. 2009. View Article : Google Scholar
|
|
7
|
Eichler AF and Batchelor TT: Primary
central nervous system lymphoma: presentation, diagnosis and
staging. Neurosurg Focus. 21:E152006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hedlund JL and Viewig BW: The Hamilton
Rating Scale for Depression: a comprehensive review. J Operational
Psychiat. 10:149–165. 1979.
|
|
9
|
Schäfer N, Glas M and Herrlinger U:
Primary CNS lymphoma: a clinician’s guide. Expert Rev Neurother.
12:1197–1206. 2012. View Article : Google Scholar
|
|
10
|
Rovner BW and Folstein MF: Mini-mental
state exam in clinical practice. Hosp Pract (Off Ed).
22:991031061101987.
|
|
11
|
Bataille B, Delwail V, Menet E, et al:
Primary intracerebral malignant lymphoma: report of 248 cases. J
Neurosurg. 92:261–266. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Melinz K, Bonelli RM, Niederwieser G,
Kenner L and Reisecker F: Primary high-grade B-cell lymphoma of the
CNS. Case report and review of the literature. Nervenarzt.
73:779–784. 2002.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fisher R and Harper C: Depressive illness
as a presentation of primary lymphoma of the central nervous
system. Aust N Z J Psychiatry. 17:84–90. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Küker W, Nägele T, Korfel A, et al:
Primary central nervous system lymphomas (PCNSL): MRI features at
presentation in 100 patients. J Neurooncol. 72:169–177. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Frühholz S, Trost W and Grandjean D: The
role of the medial temporal limbic system in processing emotions in
voice and music. Prog Neurobiol. 123:1–17. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Batchelor T and Loeffler JS: Primary CNS
lymphoma. J Clin Oncol. 24:1281–1288. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Schabet M: Epidemiology of primary CNS
lymphoma. J Neurooncol. 43:199–201. 1999. View Article : Google Scholar : PubMed/NCBI
|