Introduction
Inflammatory myofibroblastic tumor (IMT) of the
bladder is an uncommon benign tumor, which was initially reported
by Roth in 1980 (1). IMT is a rare
neoplasm of mesenchymal origin, which presents as a benign mass
that is composed of fibrous tissues and myofibroblasts, with marked
infiltration of inflammatory cells, particularly plasma cells. IMT
most commonly occurs in the lungs of children and adolescents,
however, it may occur in any part of the body (2). To date, only 30 cases of IMT have been
reported in China, and only 150 cases have been reported worldwide
(3). The occurrence of bladder cancer
during pregnancy is rare, with an incidence rate of 0.235%
(4,5)
and IMT of the urinary bladder during pregnancy is even more rare.
Radical resection is the treatment of choice for patients with IMT
in this region, to prevent local recurrence (6). The choice between transurethral
resection and partial cystectomy depends on the depth of the tumor
invasion, however complete surgical resection is important in order
to avoid local recurrence (6–8). Patients with IMT of the urinary bladder
may undergo computed tomography (CT) scanning and a cystoscopy in
order to obtain a biopsy prior to surgery to aid with diagnosis
(7,9,10). Local
tumor recurrence for IMT of the urinary bladder is 4%, with a good
patient prognosis following complete surgical resectioning
(11). To the best of our knowledge,
no study concerning IMT of the urinary bladder during pregnancy has
been previously reported. The current study describes the case of a
31-year-old pregnant female with IMT of the urinary bladder.
Written informed consent was obtained from the patient.
Case report
A 31 year-old pregnant female who had not
menstruated for 31 weeks, presented to The Affiliated Hospital of
Chifeng College (Chifeng, China) on December 7th, 2013 with
painless gross hematuria which had been present for 10 days. The
patient did not have dysuria, a fever or weight loss and there was
no previous or family history of urologic neoplasms. Physical
examination indicated that the patient was anemic (hemoglobin
plasma level, 37 g/l; normal range, 110–160 g/l) and the blood
pressure was low (88/62 mmHg; normal range 90–139/60–89 mmHg). The
fetal heart rate (FHR) was 160 beats per minute (normal range,
110–160 beats per minute). The routine blood examination indicated
that the hemoglobin was 37 g/l. A tumor of 8.0×5.3 cm in diameter
was identified in the right and front wall of bladder on
ultrasound. The ultrasound also indicated normal fetal development.
Pelvic CT imaging revealed a 5.8×6.3 cm tumor in the bladder, with
an enhanced-CT value of 40.4–60.5 HU (Fig. 1). The patient received a blood
transfusion and also received a continuous bladder irrigation to
avoid obstruction of the catheter, which prevented blood clot
formation. Cystoscopy was not performed due to the patient's weak
physical condition and the associated risk of a premature birth and
subsequently, a biopsy was not obtained prior to surgery. Following
the initial workup, on December 13th, 2013 a cesarean section was
performed as well as the partial cystectomy of bladder. A male
infant of 1.5 kg was born and a 8.0×7.0 cm tumor was removed from
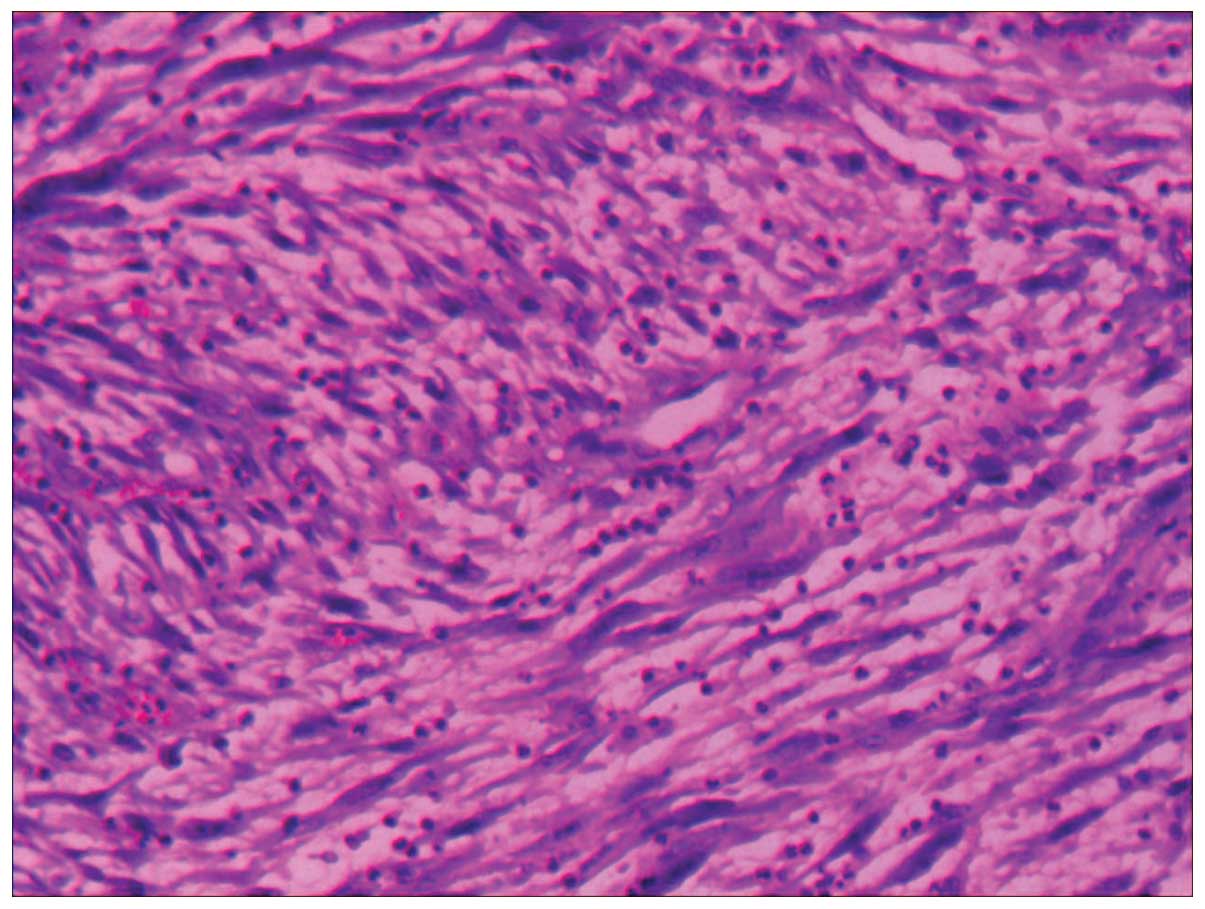
the bladder (Fig. 2). The
pathological report indicated that the growth was IMT of the
urinary bladder (Fig. 3) and a
positive cellular reaction for CD (34), CD (68), P (53), SMA and
α-AT was demonstrated by immunohistochemistry. The patient was
discharged from hospital one month following the surgery. A
follow-up cystoscopy examination was performed one year after
surgery, with subsequent follow-up cystoscope examinations
performed every three months, which revealed no tumor
recurrence.
Discussion
IMT is a rare neoplasm, which was initially reported
by Bahadori and Liebow (12) in a
lung lesion in 1973. IMT can affect any age group, however, it is
more common in infants and young adults, with 93% of IMT cases
occuring in individuals aged <20 years (13). Cases of IMT have been described in
almost all regions of the body and the most common site for IMT is
the lung (14). If present in the
genitourinary tract, this tumor type most commonly occurs is the
urinary bladder (15). The exact
etiology of IMT is unknown, however, it is hypothesized to occur
secondary to infection, trauma or surgery (16,17). IMT
is often difficult to differentiate from malignant tumors including
teratoma, liposarcoma and lymphoma prior to surgery, due to the
nonspecific radiological features exhibited by the tumor (18). Urological tumors are extremely
uncommon in pregnancy and no other instances of this condition have
been previously reported. Preoperative examination is of great
importance when IMT during pregnancy is suspected; this must
include ultrasound, cystoscopy and CT. Cystoscopy is particularly
important as it may indicate the size and position of the tumor.
Additionally, pathological results may also be obtained by
cystoscopy. Furthermore, cystoscopy does not cause harm to the
patient or fetus (4). The most common
method of treatment for IMT of bladder is partial cystectomy of the
bladder or transurethral resection of the tumor, which prevents
local recurrence (19). Intravesical
therapy is controversial following surgery. IMT exhibits aggressive
behavior, therefore it may be confused with malignancy. The method
of determining a definitive diagnosis for IMT is pathological
examination; additionally, histologically IMT is characterized by
myofibroblastic spindle cells and inflammatory cells. The
recurrence rate of IMT is 25% (20),
and due to this significant local recurrence rate, follow-up after
surgery is required.
To the best of our knowledge, this study presents
the first case of IMT of the urinary bladder during pregnancy to be
reported. Thus, future studies which investigate the diagnosis and
treatment of the disease are required to increase knowledge with
regard to this rare disease and the prognosis of such following
surgery.
References
|
1
|
Roth JA: Reactive pseudosarcomatous
response in urinary bladder. Urology. 16:635–637. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ozsan I, Ozsoy M, Sahin E, et al:
Inflammatory myofibroblastic tumor of the gallblader. Balkan Med J.
30:323–326. 2013.PubMed/NCBI
|
|
3
|
Bo Liu, Jihong Liu, Changzhe Ke, et al:
Inflammatory myofibroblastic tumor of urinary bladder: a case
report and review of the literature. Chin J Urol. 5:335–337.
2007.
|
|
4
|
Mitra S, Williamson JG, Bullock KN and
Arends M: Bladder cancer in pregnancy. J Obstet Gynaecol.
23:440–442. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hendry WF: Management of urological tumors
in pregnancy. Br J Urol. 80:(Suppl 1). 24–28. 1997.PubMed/NCBI
|
|
6
|
Kim HW, Choi YH, Kang SM, et al: Malignant
inflammatory myofibroblastic tumor of the bladder with rapid
progression. Korean J Urol. 53:657–661. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wu S, Chen L, Wan Q, et al: Inflammatory
myofibroblastic tumor of the urinary bladder in a patient with the
left renal cell carcinoma: A case report. Exp There Med.
7:1010–1012. 2014.
|
|
8
|
Machioka K, Kitagawa Y, Izumi K, et al:
Inflammatory myofibroblastic tumor of the urinary bladder with
benign pelvic lymph node enlargement: a case report. Case Rep
Oncol. 7:571–575. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pradhan MR, Ranjan P, Rao RN, et al:
Inflammatory myofibroblastic tumor of the urinary bladder managed
by laparoscopic partial cystectomy. Korean J Urol. 54:797–800.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yi XL, Lu HY, Wu YX, et al: Inflammatory
myofibroblastic tumor with extensive involvement of the bladder in
an adolescent: a case report. World J Surg Oncol. 11:2062013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Teoh JY, Chan NH, Cheung HY, et al:
Inflammatory myofibroblastic tumors of the urinary bladder: a
systematic review. Urology. 84:503–508. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bahadori M and Liebow AA: Plasma cell
granulomas of the lung. Cancer. 31:191–208. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sanders BM, West KW, Gingalewski C, et al:
Inflammatory pseudotumor of the alimentary tract: clinical and
surgical experience. J Pediatr Surg. 36:169–173. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Coffin CM, Watterson J, Priest JR and
Dehner LP: Extrapulmonary inflammatory myofibroblastic tumor
(inflammatory pseudotumor): A clinic pathologic and
immuno-histochemical study of 84 cases. Am J Surg Pathol.
19:859–872. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yagnik V, Chadha A, Chaudhari S and Patel
K: Inflammatory myofibroblastic tumor of the urinary bladder. Urol
Ann. 2:78–79. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jones EC, Clement PB and Young RH:
Inflammatory pseudotumor of the urinary bladder. A
clinicopathological, immunohistochemical, ultrastructural, and flow
cytometric study of 13 cases. Am J Surg Pathol. 17:264–274. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hojo H, Newton WA Jr, Hamoudi AB, et al:
Pseudosarcomatous myofibroblastic tumor of the urinary bladder in
children: a study of 11 cases with review of the literature. An
Intergroup Rhabdomyosarcoma Study. Am J Surg Pathol. 19:1224–1236.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen CK, Jan CI, Tsai JS, et al:
Inflammatory myofibroblastic tumor of the lung - a case report. J
Cardiothorac Surg. 5:552010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Inoue T, Kinoshita H, Horikoshi M, et al:
A case of inflammatory myofibroblastic tumor of the urinary
bladder. Hinyokika Kiyo. 57:141–145. 2011.(In Japanese). PubMed/NCBI
|
|
20
|
Lawrence B, Perez-Atayde A, Hibbard MK, et
al: TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic
tumors. Am J Pathol. 157:377–384. 2000. View Article : Google Scholar : PubMed/NCBI
|