Introduction
Vestibular schwannomas (VSs) are histologically
benign tumors that originate from the vestibular division of the
eighth cranial nerve. The tumors may occur sporadically, most
commonly in the fifth decade of life and later, or as part of the
clinical complex in neurofibromatosis type 2 (NF2), which occurs
bilaterally and in young individuals. Sporadic or non-NF2 VSs are
extremely rare in pediatric patients (1).
Currently, there are a variety of treatment options
for the management of VSs, including observation with serial
imaging, radiosurgery and microsurgery (2). The range of tumor volumes and growth
patterns make the management of these lesions an issue that is much
debated. Due to the clinical heterogeneity among patients with VSs,
no standard patient management has been reported (3). Pediatric patients with small VSs can be
challenging to neurosurgeons.
In the present study we discuss the presentation,
treatment course and follow-up outcome for a pediatric patient with
sporadic unilateral VSs and reviewed other related literature. This
study aims to explore the current treatment paradigm for sporadic
Vss in the pediatric population. Written informed consent was
obtained from the patient's family for publication of this case
study and the accompanying images.
Case report
In March 2009, a 15-year-old male, previously in
good health, presented to Tongji Hospital, Huazhong University of
Science and Technology (Wuhan, China) with complaints of left-sided
progressive hearing loss that had been apparent for six months.
Upon examination, left-sided sensorineural hearing loss of 60 dB
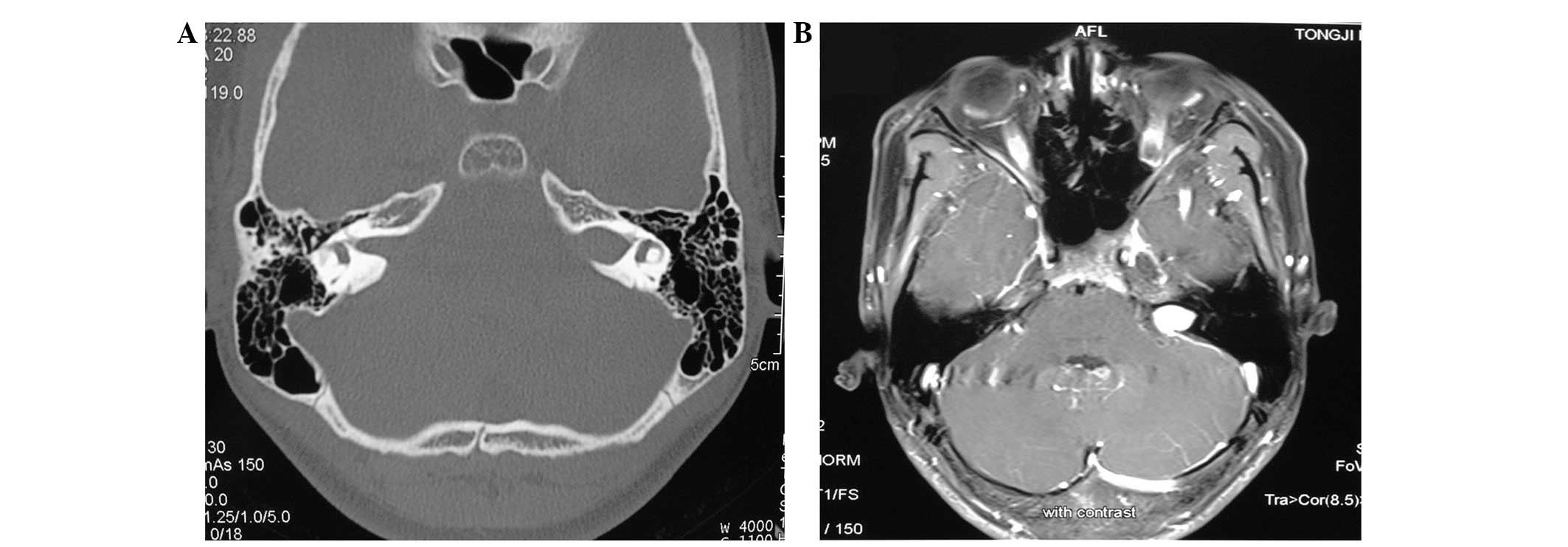
was found, with no other neurological impairments. Cerebral
computed tomography revealed an enlarged inner auditory canal on
the left side (Fig. 1A). Magnetic
resonance imaging (MRI) with gadolinium diethylenetriamine
penta-acetic acid demonstrated a mass that was entirely located in
the inner auditory canal, measuring 10 mm at its largest diameter
(Fig. 1B). Homogeneous enhancement
was documented on contrast MRI. The patient had no family history
of NF2 and gene mutation analysis showed no signs of the condition.
Following a discussion on the risks and benefits of microsurgery
versus γ-knife surgery, and subsequent to conservative observation
with a series of images, the patient chose radiosurgery treatment,
which was administered once at a dose of 11.7 Gy. Following
radiosurgery, the patient was discharged with left-sided hearing
loss. No other neurological complaints or findings were observable
on a physical examination. At 36 months post-treatment, the patient
exhibited no identifiable tumor enlargement.
Discussion
VSs represent 0.8% of all tumors in pediatric
patients (<16 years of age). They are more common in young males
than young females, although VSs are more common in females overall
(4). The present study reports a case
of VS in a male patient. An extensive literature review reveals
only one reported case of small (≤10-mm) non-NF2 VS in the
pediatric population as part of a case series (5). Furthermore, Walcott et al
(1) reported seven cases of larger
VSs in the pediatric population, Holman et al (4) reported 20 cases of small pediatric VSs
with NF2 and 13 cases of larger sporadic VSs in the pediatric
population and Hueng et al (6)
reported three adult cases of sporadic VSs. The present study is
the first case report with a clinical description and radiological
images of this entity. Unlike in adults, children may easily
neglect the early symptoms of VS, such as unilateral hearing loss
or tinnitus; instead the tumors are often identified by the more
overt signs caused by the space-occupying nature of the tumor. This
delay in diagnosis, usually for longer than months or years, has
often resulted in tumors that are large in size (5).
Within the literature, the treatment strategies for
small VSs are varied, making it difficult for a neurosurgeon to
decide the best course of action (4,7,8). In a study from the US, the strongest
predictors of treatment modality were patient age and tumor size
(3). The treatment decision rests on
the availability of information with regard to the characteristics
of the patient and the tumor. The decision is often hard due to
inconsistencies in the data on the natural history of VS, the
mechanism of hearing loss, and the hearing and facial function
preservation rates associated with treatment (9). This variability is a major obstacle to
practicing evidence-based medicine. The dilemma in treatment
decision-making is complicated in children due to implications for
the impairment of childhood development and lifelong disability.
The first concern is preservation of facial nerve function, which
is paramount, particularly in children, as it is often regarded as
the most important index for quality of life post-operatively
(5).
It has been suggested that certain factors,
including the preference of the patient toward risk-aversion, the
relative weight of discomfort at the present time versus the
possible loss of function in the future, and the degree of comfort
with regard to an uncertain long-term prognosis following radiation
or during observation, will heavily effect the treatment decision
(10). For the present patient, a
summary of information on all three management options was
provided. While radiosurgery was recommended to this pediatric
patient with a small tumor, observation and surgery were also
discussed, and the pros and cons of these treatment options were
conveyed. This dialogue can avoid later dispute concerning the
treatment of other individuals using means that the patient had not
been told about, which can easily lead to distrust and even
discrepancy.
All three treatment options may have been of optimal
use for this case in the present medical environment. More
objective data on treatment comparisons in VS management in the
future will provide further evidence to aid patients and
neurosurgeon in the decision-making process with a rational basis.
Outcome measures should include quality of life, using a scaling
system specifically designed for this entity. The treatment
strategies for small VSs in pediatric patients should be tailored
to the clinical, personal and social requirements of the patient.
However, a rigid treatment protocol is not practical at present,
and the treatment decision-making for this type of lesion is always
an art form in itself.
To conclude, in the present case the treatment
method without randomized controlled trial evidence was chosen on
an individual basis, taking into consideration the patient's
preferences, clinician experience and the availability of
radiosurgical equipment. γ-knife radiosurgery was confirmed to
provide long-term tumor control for sporadic small sized vestibular
schwannoma in pediatric patients. The risk for loss of hearing is
high, whereas the risk for other cranial nerve complications is
low. Therefore, radiosurgical treatment should be considered for
the management of sporadic small VS in pediatric patients if
imaging indicates a small tumor size. Future studies using large
patient cohorts are required to establish a standard treatment
procedure for this condition.
References
|
1
|
Walcott BP, Sivarajan G, Bashinskaya B,
Anderson DE, Leonetti JP and Origitano TC: Sporadic unilateral
vestibular schwannoma in the pediatric population. Clinical
article. J Neurosurg Pediatr. 4:125–129. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Araiza Navarrete JA, Aquirre Amador LA,
Escamilla Ocañas CE, Martínez Menchaca HR, Treviño Alanís MG and
Rivera Silva G: Vestibular schwannoma. Gac Med Mex. 148:192–193.
2012.[(In Spanish)]. PubMed/NCBI
|
|
3
|
Babu R, Sharma R, Bagley JH, Hatef J,
Friedman AH and Adamson C: Vestibular schwannomas in the modern
era: epidemiology, treatment trends, and disparities in management.
J Neurosurg. 119:121–130. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Holman MA, Schmitt WR, Carlson ML,
Driscoll CL, Beatty CW and Link MJ: Pediatric cerebellopontine
angle and internal auditory canal tumors: clinical article. J
Neurosurg Pediatr. 12:317–324. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mazzoni A, Dubey SP, Poletti AM and
Colombo G: Sporadic acoustic neuroma in pediatric patients. Int J
Pediatr Otorhinolaryngol. 71:1569–1572. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hueng DY and Sytwu HK: Vestibular
schwannoma growth and hearing loss. J Neurosurg. 120:7862014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hasegawa T, Kida Y, Kato T, Iizuka H,
Kuramitsu S and Yamamoto T: Long-term safety and efficacy of
stereotactic radiosurgery for vestibular schwannomas: evaluation of
440 patients more than 10 years after treatment with Gamma Knife
surgery. J Neurosurg. 118:557–565. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hayashi M, Chernov MF, Lipski SM, Tamura
N, Yomo S, Horiba A, Tsuzuki S, Izawa M, Okada Y, Muragaki Y, et
al: Do we really still need an open surgery for treatment of
patients with vestibular schwannomas? Acta Neurochir Suppl.
116:25–36. 2013.PubMed/NCBI
|
|
9
|
Robinett ZN, Walz PC, Miles-Markley B,
Moberly AC and Welling DB: Comparison of long-term quality-of-life
outcomes in vestibular schwannoma patients. Otolaryngol Head Neck
Surg. 150:1024–1032. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rutherford SA and King AT: Vestibular
schwannoma management: What is the ‘best’ option? Br J Neurosurg.
19:309–316. 2005. View Article : Google Scholar : PubMed/NCBI
|