Introduction
Calcyclin binding protein (CacyBP) was initially
described as a binding partner of calcylin (S100A6) at
physiological Ca2+ concentrations in Ehrlich ascites
tumor cells (1). Three years later,
Matsuzawa and Reed (2) identified
that the human analog of mouse CacyBP interacts with Siah-1, and
this protein was termed Siah-1-interacting protein (SIP). Thus, the
protein is now referred to as CacyBP/SIP.
Various reports propose a role for CacyBP/SIP in
cellular processes, such as ubiquitination (2), proliferation (3), differentiation (4,5),
tumorigenesis, cytoskeletal rearrangement (6,7) and
transcriptional regulation (8). In
our previous study, it was identified that CacyBP is expressed at
higher levels in multidrug-resistant gastric cancer cells
(SGC7901/adriamycin) compared with the parental cell line (SGC7901)
(9). Thus, upregulation of CacyBP/SIP
may enhance the resistance of gastric cancer cells to various types
of chemotherapeutic agents, whereas downregulation of CacyBP/SIP
may partially reverse the drug-resistant properties of gastric
cancer cells (10). Thus, to
understand the function of CacyBP in cancer, our previous study
produced three monoclonal antibodies against CacyBP (11). Using these antibodies, it was
identified that numerous types of healthy tissue, including gastric
tissue, exhibited minimal expression of CacyBP/SIP, whereas
numerous types of cancerous tissue expressed, or even
overexpressed, CacyBP/SIP (12).
Additional studies have implicated CacyBP/SIP in
tumorigenesis, although whether it promotes or suppresses cancer
appears to depend on the cell type. For example, overexpressed
CacyBP/SIP suppressed the growth of renal and gastric cancer cells
(13,14). However, CacyBP/SIP expression levels
were significantly increased in pancreatic cancer tissue compared
with adjacent non-cancerous pancreatic tissue, and the expression
level was associated with the degree of tumor differentiation,
higher tumor, node, metastasis (TNM) stage and distal metastasis
(15). Additionally, CacyBP/SIP
expression levels were higher in more clinically advanced breast
cancer, including metastatic breast cancer (16).
Considering the opposing roles of CacyBP/SIP in
cancer tumorigenesis, the present study aimed to determine the
whether CacyBP acts as a suppressor or promoter of tumorigenesis in
gastric cancer. Thus, immunohistochemical analysis of tissue
samples from gastric cancer patients was performed to detect the
expression levels of CacyBP/SIP, and to compare CacyBP/SIP
expression levels between metastatic and non-metastatic cancer
tissue.
Materials and methods
Patients and tissue specimens
Formalin-fixed, paraffin-embedded tumor tissues were
obtained from the General Hospital of Ningxia Medical University
(Yinchuan, China). A total of 181 samples of gastric adenocarcinoma
tissue and adjacent non-cancerous gastric tissues were collected
from the same patients. The patients included 80 cases of
non-metastatic gastric cancer and 101 cases of gastric cancer that
had metastasized to the lymph nodes. None of the patients had
undergone preoperative radiotherapy or chemotherapy. In addition,
three frozen tissue samples of gastric adenocarcinoma were used in
the present study, which were obtained from the General Hospital of
Ningxia Medical University. The diagnoses of the paraffin-embedded
and fresh tissue specimens were independently established by two
experienced pathologists, according to the National Comprehensive
Cancer Network guidelines for gastric cancer (2013) (17). This study was approved by the ethics
committee of the General Hospital of Ningxia Medical University and
written informed consent was obtained from all patients.
Immunohistochemical staining and
evaluation
CacyBP/SIP expression levels were detected in the
5-µm paraffin-embedded tissue sections using PV-6002 Power Vision
Two-Step Histostaining Reagent, according to the manufacturer's
instructions (Dako North America, Inc., Carpinteria, CA, USA). The
antibody used for immunohistochemistry was a CacyBP/SIP-specific
mouse anti-human monoclonal antibody prepared in our laboratory as
previously described (clone EA1; dilution, 1:150; initial
concentration, 2.1 mg/ml) (11).
Negative controls were prepared by replacing the primary antibody
with pre-immune mouse serum (Beyotime Institute of Biotechnology,
Beijing, China). The immunohistochemical stains were independently
evaluated by two pathologists who were not aware of the status of
the samples (metastatic or non-metastatic). Cytoplasmic/nuclear
staining was considered to indicate positive CacyBP expression and
was scored on the following basis: 0, no detectable staining; 1+,
<25% positive cells; 2+, 25–49% positive cells; 3+, 50–74%
positive cells; 4+, >75% positive cells. In general, cases
demonstrating 3+ and 4+ staining were intensely stained, therefore,
the level of intensity was not considered when calculating the
score.
Clinicopathological assessment
The immunohistochemical results were compared
against patient data and pathology analysis of the tissue slices.
The slices were assessed for gender, age, degree of tumor
differentiation and TNM stage.
Western blot analysis
Tissue samples of gastric adenocarcinoma were lysed
in 300 µl freshly prepared extraction buffer [1% SDS, 1 mmol/l
Na3VO4 and 0.1 mol/l Tris (pH 7.4)] and the
proteins (40 µg/lane) were resolved on 12% SDS-polyacrylamide gels,
prior to being electrophoretically transferred to polyvinylidene
difluoride membranes (EMD Millipore, Bedford, MA, USA) for 20–50
min at 20 V. The membranes were incubated at 4°C overnight with one
of the following primary monoclonal antibodies: CacyBP/SIP
(dilution, 1:1,000) or mouse anti-canine β-actin (dilution,
1:2,000; cat. no. A2228; Sigma Aldrich, St. Louis, MO, USA).
Subsequently, the membranes were incubated with monoclonal goat
anti-mouse IgG secondary antibody (dilution, 1:2,000; cat. no.
RPN5782; GE Healthcare Life Sciences, Piscataway, NJ, USA) and were
detected using a SuperSignal West Pico Chemiluminescent Substrate
kit (Pierce Biotechnology, Inc., Rockford, IL, USA). For each
western blotting result, a minimum of three independent experiments
were conducted; representative images are indicated in the results
section.
Statistical analysis
Statistical analysis was performed using SPSS
software (version 10.0; SPSS Inc., Chicago, IL, USA). The
χ2 test and Fisher's exact test were used to determine
the significance of the difference in frequency of CacyBP/SIP
expression levels between non-metastatic and metastatic gastric
cancer. P<0.05 was considered to indicate a statistically
significant difference.
Results
Expression levels of CacyBP/SIP
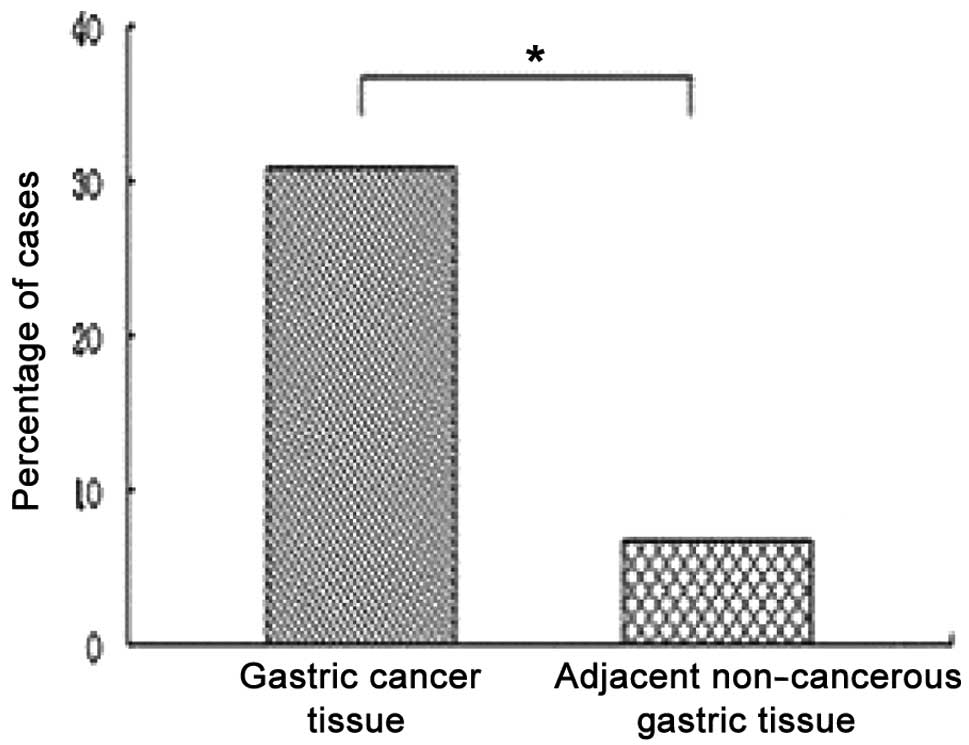
Among the 181 cases, the rates of CacyBP/SIP
expression were 31% (56/181) in cancerous and 7% (12/181) in
adjacent non-cancerous gastric tissues, thus, the CacyBP/SIP
expression rate was significantly higher in the cancerous gastric
tissue samples (P<0.05; Fig. 1).
In the majority of cancer cells, CacyBP/SIP-positive staining was
observed simultaneously in the cytoplasm and nuclei (Fig. 2A and B). Additionally, CacyBP/SIP
expression levels were examined by performing western blot analysis
on the cancerous and adjacent non-cancerous gastric tissues taken
from three patients. Western blotting demonstrated that CacyBP/SIP
expression levels were higher in the three cancerous gastric tissue
samples compared with the corresponding adjacent non-cancerous
gastric tissue samples (Fig. 3).
CacyBP/SIP expression levels and
clinicopathological features
The expression levels of CacyBP/SIP in the patient
samples were compared against the clinicopathological findings of
the patients (Table I). No
significant association was identified between CacyBP/SIP
expression and patient age (P=0.975), gender (P=0.185), degree of
tumor differentiation (P=0.076) or TNM stage (P=0.979).
 | Table I.Association of CacyBP/SIP expression
levels with clinicopathological features of gastric cancer
(n=181). |
Table I.
Association of CacyBP/SIP expression
levels with clinicopathological features of gastric cancer
(n=181).
| Category | | Level of CacyBP/SIP
expression, n | P-value |
|---|
|
|---|
| n (%) | 0 | 1+ | 2+ | 3+ | 4+ |
|---|
| Gender |
|
|
|
|
|
|
|
| Male | 109 (60) | 70 | 17 | 17 | 3 | 2 | 0.185 |
|
Female | 72 (40) | 53 | 11 | 6 | 2 | 1 |
|
| Age, years |
|
|
|
|
|
|
|
|
<50 | 59 (33) | 40 | 7 | 9 | 2 | 1 | 0.975 |
| ≥50 | 122 (67) | 83 | 20 | 14 | 3 | 2 |
|
| Tumor
differentiation |
|
|
|
|
|
|
|
|
Well-differentiated | 50 (28) | 38 | 5 | 5 | 1 | 1 | 0.076 |
|
Moderately differentiated | 39 (22) | 21 | 10 | 6 | 1 | 1 |
|
| Poorly
differentiated | 92 (50) | 64 | 12 | 12 | 3 | 1 |
|
| TNM stage |
|
|
|
|
|
|
|
| I +
II | 84 (46) | 57 | 12 | 10 | 3 | 2 | 0.979 |
| III +
IV | 97 (54) | 66 | 15 | 13 | 2 | 1 |
|
Expression levels of CacyBP/SIP in
metastatic gastric cancer
To investigate whether an association exists between
the expression levels of CacyBP/SIP and metastasis of gastric
cancer, the expression levels of CacyBP/SIP were compared between
primary tumor sites and the corresponding lymph node metastatic
sites in 101 patients with metastatic gastric cancer. CacyBP/SIP
expression was detected as cytoplasmic/nuclear staining of
variously differentiated cancer tissues (Fig. 2C and D), consistent with our previous
study (7). In the present study,
CacyBP/SIP was expressed at primary sites in 31% (31/101) of
patients and at metastatic sites in 26% (26/101) of patients, thus,
no significant difference was identified in the level of CacyBP/SIP
expression between the primary and metastatic sites of the same
metastatic gastric cancer patients (P=0.434; Table II).
 | Table II.Comparison of CacyBP/SIP expression
levels between primary and metastatic sites from the same gastric
cancer patients. |
Table II.
Comparison of CacyBP/SIP expression
levels between primary and metastatic sites from the same gastric
cancer patients.
| Tumor site | | Level of CacyBP/SIP
expression, n | P-value |
|---|
|
|---|
| n | 0 | 1+ | 2+ | 3+ | 4+ |
|---|
| Primary | 101 | 70 | 14 | 12 | 3 | 2 | 0.434 |
| Metastatic | 101 | 75 | 12 | 9 | 2 | 3 |
Subsequently, the expression levels of CacyBP/SIP
were compared between the primary tumor sites of 80 patients with
non-metastatic gastric cancer and the metastatic tumor sites of 101
patients with metastatic gastric cancer. As indicated in Table III, CacyBP/SIP was expressed in 34%
(27/80) of the non-metastatic gastric cancer patients and in 31%
(31/101) of the metastatic gastric cancer patients. No significant
difference was identified in the frequency of CacyBP/SIP expression
between the two groups of patients (P=0.662).
 | Table III.Comparison of CacyBP/SIP expression
levels at primary tumor sites in patients with metastatic gastric
cancer and patients with non-metastatic gastric cancer. |
Table III.
Comparison of CacyBP/SIP expression
levels at primary tumor sites in patients with metastatic gastric
cancer and patients with non-metastatic gastric cancer.
| Type of gastric
cancer | | Level of CacyBP/SIP
expression, n | P-value |
|---|
|
|---|
| n | 0 | 1+ | 2+ | 3+ | 4+ |
|---|
| Metastatic (lymph
node) | 101 | 70 | 14 | 12 | 3 | 2 | 0.662 |
| Non-metastatic | 80 | 53 | 13 | 11 | 2 | 1 |
|
Discussion
Previous studies identified that overexpression of
CacyBP/SIP inhibits the proliferation of gastric cancer cells,
suppresses tumorigenesis in vitro and prolongs the survival
of tumor-bearing nude mice (14,18).
Additionally, downregulation of CacyBP/SIP by RNA interference has
the opposite effects. These findings indicate that CacyBP/SIP acts
as a suppressor in gastric cancer, however, the expression of
CacyBP/SIP in gastric cancerous tissue is unknown. In the present
study, the expression levels of CacyBP/SIP were evaluated in
clinical samples from gastric cancer patients. The results
indicated that the level of CacyBP/SIP expression in gastric cancer
tissues is significantly higher compared with the adjacent
non-cancerous gastric tissues (31 vs. 7%; P<0.05); this was
confirmed by western blot analysis. However, subsequent analysis of
the clinicopathological features revealed that the expression
levels of CacyBP/SIP were not associated with clinicopathological
factors of gastric cancer, such as age, gender, tumor size, degree
of tumor differentiation or TNM stage. According to the results of
the present study, CacyBP/SIP may not act as a tumor suppressor in
gastric cancer as it is highly expressed in gastric cancer tissue.
These conflicting results require additional studies to be
performed to clarify the role of CacyBP/SIP in gastric cancer.
CacyBP/SIP expression was detected in only 31% of
the gastric cancer samples using immunohistochemistry, however, it
was detected in 100% of the samples using western blotting. This
discrepancy may be due to differences in the sensitivity of the two
assays or due to a statistical anomaly, as only three samples were
assessed using western blot analysis. Furthermore, a significantly
higher frequency of CacyBP/SIP expression was identified in the
nuclei of cancerous gastric tissue; thus, further studies are
required to explore the possible role of CacyBP/SIP in gastric
cancer.
Various studies have identified an association
between CacyBP/SIP expression levels and different types of cancer
metastasis. In the present study, the association between
CacyBP/SIP expression levels and gastric cancer metastasis was
investigated; however, no evidence of an association was detected.
No significant difference was identified in the expression levels
of CacyBP/SIP between primary and metastatic gastric cancer sites
from the same patients. In addition, no significant difference was
identified in the expression levels of CacyBP/SIP between
non-metastatic and metastatic gastric cancer tissue from different
patients.
Unlike breast and pancreatic cancer, in which
CacyBP/SIP is involved in metastasis, CacyBP/SIP does not appear to
be involved in the metastasis of gastric cancer. The progression of
breast and pancreatic cancer are associated with CacyBP/SIP
expression or overexpression, whereas the present study identified
that overexpression of CacyBP/SIP results in the suppression of
renal and gastric cancer cell growth. Thus, the present study
proposes that CacyBP/SIP behaves differently in different types of
cancer, and these differences should be the focus of future
studies. It is possible that CacyBP/SIP has tumor-specific roles,
similar to silent information regulator 1, nuclear factor-κB and
transforming growth factor-β (19–21).
Although CacyBP/SIP is important in the
tumorigenesis of cancer, the present study indicates that
CacyBP/SIP may promote tumor suppression as opposed to being
involved in the metastasis of gastric cancer. Furthermore,
CacyBP/SIP expression levels do not appear to be associated with
common clinicopathological features of gastric cancer. In
conclusion, the results of the present study indicate that
CacyBP/SIP plays a different role in gastric cancer than it does in
breast or pancreatic cancer.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81072040).
Abbreviations:
|
CacyBP/SIP
|
calcyclin binding protein/Siah-1
interacting protein
|
References
|
1
|
Filipek A and Kuźnicki J: Molecular
cloning and expression of a mouse brain cDNA encoding a novel
protein target of calcyclin. J Neurochem. 70:1793–1798. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Matsuzawa SI and Reed JC: Siah-1, SIP, and
Ebi collaborate in a novel pathway for beta-catenin degradation
linked to p53 responses. Mol Cell. 7:915–926. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang YJ, Liu WM, Zhou JX, et al:
Expression and hormonal regulation of calcyclin-binding protein
(CacyBP) in the mouse uterus during early pregnancy. Life Sci.
78:753–760. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Au KW, Kou CY, Woo AY, et al: Calcyclin
binding protein promotes DNA synthesis and differentiation in rat
neonatal cardiomyocytes. J Cell Biochem. 98:555–566. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Herington JL, Bi J, Martin JD and Bany BM:
Beta-catenin (CTNNB1) in the mouse uterus during decidualization
and the potential role of two pathways in regulating its
degradation. J Histochem Cytochem. 55:963–974. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schneider G, Nieznanski K, Kilanczyk E, et
al: CacyBP/SIP interacts with tubulin in neuroblastoma NB2a cells
and induces formation of globular tubulin assemblies. Biochim
Biophys Acta. 1773:1628–1636. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Filipek A, Schneider G, Mietelska A,
Figiel I and Niewiadomska G: Age-dependent changes in neuronal
distribution of CacyBP/SIP: comparison to tubulin and the tau
protein. J Neural Transm. 115:257–264. 2008. View Article : Google Scholar
|
|
8
|
Kilanczyk E, Filipek S, Jastrzebska B and
Filipek A: CacyBP/SIP binds ERK1/2 and affects transcriptional
activity of Elk-1. Biochem Biophys Res Commun. 380:54–59. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liang J, Luo G, Ning X, et al:
Differential expression of calcium-related genes in gastric cancer
cells transfected with cellular prion protein. Biochem Cell Biol.
85:375–383. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shi Y, Hu W, Yin F, et al: Regulation of
drug sensitivity of gastric cancer cells by human calcyclin-binding
protein (CacyBP). Gastric Cancer. 7:160–166. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhai H, Shi Y, Yu J, et al: Establishment
and characterization of calcyclin binding protein (CacyBP)
monoclonal antibody. Hybridoma (Larchmt). 25:91–94. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhai H, Shi Y, Jin H, et al: Expression of
calcyclin-binding protein/Siah-1 interacting protein in normal and
malignant human tissues: an immunohistochemical survey. J Histochem
Cytochem. 56:765–772. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sun S, Ning X, Liu J, et al: Overexpressed
CacyBP/SIP leads to the suppression of growth in renal cell
carcinoma. Biochem Biophys Res Commun. 356:864–871. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ning X, Sun S, Hong L, et al:
Calcyclin-binding protein inhibits proliferation, tumorigenicity,
and invasion of gastric cancer. Mol Cancer Res. 5:1254–1262. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen X, Han G, Zhai H, et al: Expression
and clinical significance of CacyBP/SIP in pancreatic cancer.
Pancreatology. 8:470–477. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang N, Ma Q, Wang Y, Ma G and Zhai H:
CacyBP/SIP expression is involved in the clinical progression of
breast cancer. World J Surg. 34:2545–2552. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ajani JA, Bentrem DJ, Besh S, et al:
National Comprehensive Cancer Network: Gastric cancer, version
2.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc
Netw. 11:531–546. 2013.PubMed/NCBI
|
|
18
|
Ning X, Sun S, Zhang K, et al: S100A6
protein negatively regulates CacyBP/SIP-mediated inhibition of
gastric cancer cell proliferation and tumorigenesis. PLoS One.
7:e301852012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Deng CX: SIRT1, is it a tumor promoter or
tumor suppressor? Int J Biol Sci. 5:147–152. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Perkins ND: NF-κB: tumor promoter or
suppressor? Trends Cell Biol. 14:64–69. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bachman KE and Park BH: Duel nature of
TGF-β signaling: tumor suppressor vs. tumor promoter. Curr Opin
Oncol. 17:49–54. 2005. View Article : Google Scholar
|