Introduction
Papillomatosis primarily presents as multiple
lesions that arise in the oral cavity, larynx and vulva, and to a
lesser extent, in segments of the trachea. It most frequently
occurs in children or adolescents (1). Solitary papilloma is extremely rare and
its occurrence in the trachea is even rarer, accounting for
<0.5% of all lung tumors (2).
Tracheal papilloma is a benign neoplastic condition that is
characterized by continuous papillomatous growth of the bronchial
epithelium (3). In 3–5% of patients,
respiratory papillomas may undergo malignant degeneration to become
a squamous cell carcinoma. The prognoses of these particular
patients are relatively poor (4).
Transformation is believed to be associated with infection by the
human papilloma virus (HPV) and smoking. However, the mechanism
underlying transformation is not fully understood (5).
To the best of our knowledge, the present study is
the first to describe the malignant conversion of a solitary
tracheal papilloma into a squamous cell carcinoma in an adult
patient who was subsequently treated by radiotherapy.
Case report
On August 20, 2011, a 54-year-old male was admitted
to the Mianyang Central Hospital (Mianyang, China) with a cough,
sputum and dyspnea that had been apparent for one month. The
patient was a farmer and had been smoking >20 cigarettes per day
for >30 years; however, the patient had not been exposed to
other risk factors, including carcinogenic agents,
immunosuppressants or radiation. The patient had been previously
diagnosed with pneumonia and treated accordingly, until the
symptoms of dyspnea worsened and hemoptysis developed.
A physical examination revealed that the patient had
a temperature of 38.0°C (100.4°F) (normal range, 36.3–37.2°C), a
respiratory rate of 20 breaths/min (normal range, 16–20
breaths/min), a heart rate of 80 beats/min (normal range, 60–100
beats/min) and a blood pressure of 110/65 mmHg (normal range,
90–140/60–90 mmHg). A chest examination revealed a moist rale and
decreased tactile fremitus in the lower left chest. Examination of
the head, ears, oral cavity and throat was unremarkable. No
swelling of the lymph nodes was detected in the neck.
A complete blood count revealed a white blood cell
count of 8.51×109/l, with 81.9% neutrophils. Chest
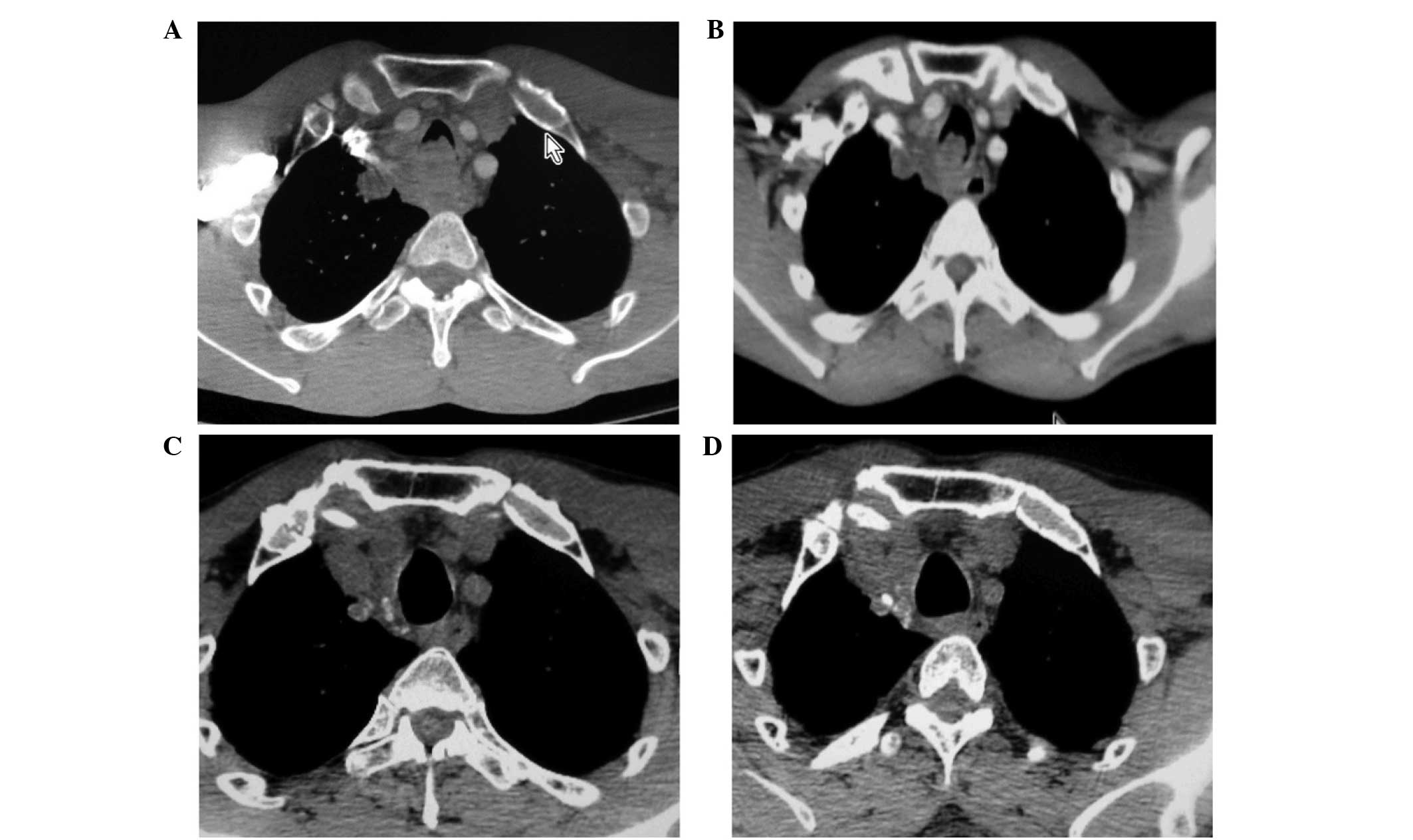
computed tomography (CT) revealed a 5.6×3.0×4.7-cm mediastinal
soft-tissue mass, which had invaded the trachea, a swollen nodule
in the upper right mediastinum and pneumonia in the inferior lobe
of the left lung (Fig. 1A). Flexible
bronchofiberscopy revealed a 4-cm red, granular mass on the
posterior tracheal wall that was 5 cm below the glottis. The mass
resulted in ∼90% central airway obstruction, which prevented the
passage of a flexible bronchofiberscope through the airway
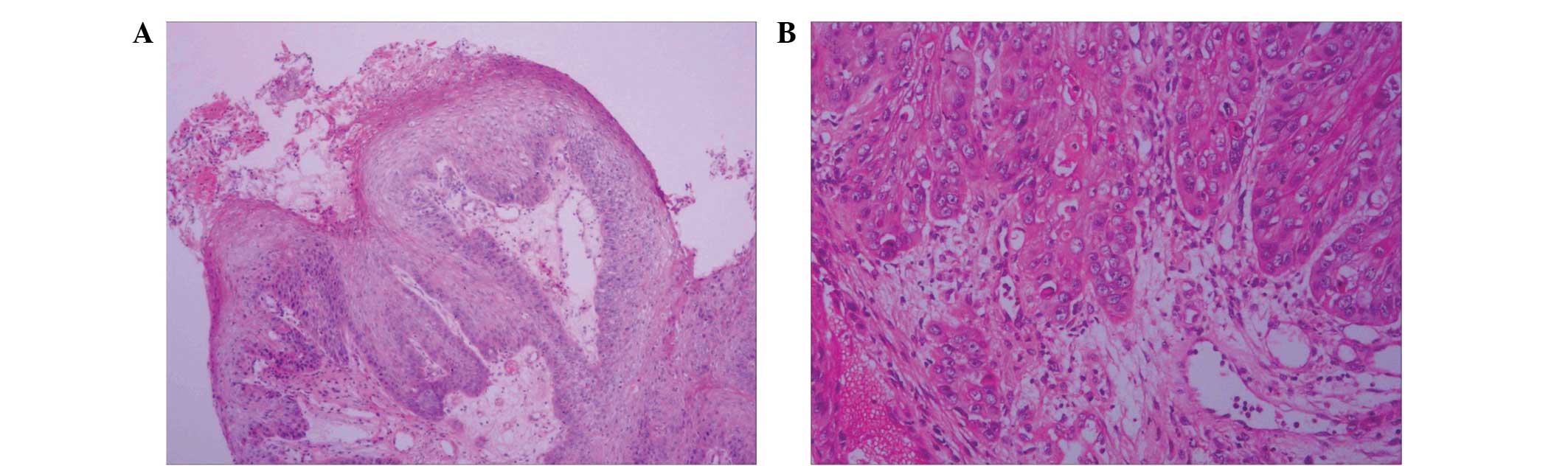
(Fig. 2A). Multiple biopsies of the
tumor identified a squamous cell papilloma with moderate to severe
atypical hyperplasia and squamous cell carcinoma formation
(Fig. 3A and B). The pathological
findings of the specimens were confirmed by the West China Hospital
of Sichuan University (Chengdu, China). Infection with HPV strains
6, 11, 16, 18, 31, 33, 35, 39, 40, 42–45, 51–54, 58, 59, 66, 68, 70
and 81 in the tumor specimens was ruled out by performing
polymerase chain reaction analysis.
The day after admission, the patient's temperature
rose to 39.3°C (102.74°F). In addition, the symptoms of dyspnea
were aggravated upon reclining, and the patient had to be kept
seated. A sputum culture resulted in Klebsiella pneumoniae
growth, and a drug sensitivity analysis revealed that the strain
was sensitive to cefotaxime. Therefore, intravenous cefotaxime (2.0
g) was administered every 12 h and, after six days, the patient's
temperature returned to normal levels.
The case was discussed by a multidisciplinary team
that included anesthesiologists, physicians, oncologists and
thoracic surgeons, who agreed that the tumor could not be resected
successfully due to its invasive growth. Therefore, radiotherapy
was administered four days after diagnosis, on August 24, 2011.
Initially, radiotherapy was performed with the
patient in a sitting position. Following 18 fractions of
radiotherapy (2 Gy/fraction), the symptoms of cough, sputum,
dyspnea and hemoptysis were alleviated, and the patient was able to
receive radiotherapy in the reclined position without any
discomfort. At this time, a CT scan and flexible bronchofiberscopy
indicated a decrease in the size of the tumor to 5.4×2.5×4.5 cm
(Figs. 1B and 2B). Therefore, a radiotherapy regimen using
three-dimensional conformal radiotherapy was administered in the
reclined position for 42 days. The gross tumor volume (GTV) was
defined as the volume of visible tumor as determined using the
mediastinal window setting. The soft-tissue of the mediastinum,
trachea and nodule in the upper right mediastinum were included in
the GTV. The clinical target volume (CTV) included the GTV with
5-mm margins along the x and y axes, and 15-mm margins along the z
axes. The planning target volume (PTV) included the CTV with a 7-mm
margin. The total dose prescription was 60 Gy/30 F for the PTV. The
V20 to the lung was 8%, and the maximal dose to the spinal cord was
4570 cGy. During radiotherapy, the patient experienced moderate
pain when swallowing as a result of radiation-induced
esophagitis.
A CT scan performed two months after the completion
of radiotherapy treatment revealed that the mass in the trachea had
markedly reduced in size. The mediastinal soft-tissue mass and the
nodule in the upper right lung were significantly reduced, but
exhibited slight calcification (Fig.
1C). After four months, routine fiber bronchoscopy indicated no
recurrent papilloma at the same site. However, a CT scan revealed
further evidence of calcification (Figs.
1D and 2C). The patient
demonstrated disease-free survival, with no evidence of recurrence
during a two-year follow-up period. At the time of writing, the
patient remained alive with no symptoms of disease.
Discussion
Tracheal papillomatosis is the manifestation of
recurrent respiratory papillomatosis (RRP), which usually occurs
during early childhood and between the ages of 30 and 40 years
(3). However, only a few cases of RRP
affecting elderly patients have been reported (3). The incidence of adult RRP in the United
States is estimated to be 1.8 cases per 100,000 of the population
(6). Despite this, <50 cases of
solitary endobronchial papillomas have been reported in the English
literature (7). Pathologists classify
solitary papillomas into three types as follows: i) Squamous
papilloma; ii) glandular papilloma; and iii) mixed papilloma.
Squamous papilloma is most commonly diagnosed in smokers, aged
between 26 and 74 years old (8).
Malignant transformation is rare, with a 1% occurrence rate in
cases of juvenile RRP and a 3–7% in cases of adult RRP (9). Malignant transformation may occur at any
location in the respiratory tract; however, transformation in the
trachea is extremely rare (10).
Multiple papillomas of the tracheobronchial tree
with malignant transformation have been first reported by DiMarco
et al (11) in 1978. To the
best of our knowledge, only four cases of malignant transformation
of a solitary papilloma in the trachea had been reported in the
English literature until 2012 (12,13).
The mechanism of transformation from RRP to squamous
cell carcinoma remains unclear. A previous study reported that the
majority of malignant transformation cases are associated with HPV
type, smoking status, performance of irradiation, immunosuppressant
use and exposure to carcinogenic agents (10). The present study described the case of
a heavy smoker who presented no evidence of HPV infection. HPV has
been associated with the pathogenesis of solitary tracheobronchial
papilloma (13). In total, ∼100
different types of HPV have been identified, each associated with
different malignant potentials and symptom severities. HPV 6 and 11
are the most commonly identified types in cases of solitary
tracheobronchial papilloma and are associated with a low risk of
carcinomatous transformation (1,13). In
addition, HPV types 16 and 18, occasionally in combination with
types 31, 33 or 35, are associated with a higher risk of
carcinomatous transformation (13).
Rady et al (14) analyzed the
molecular genetic alterations in a case of squamous cell carcinoma
that had arisen from RRP. Integrated and episomal forms of HPV 11
DNA have been detected in histologically benign tumors. By
contrast, only the integrated form of HPV 11 DNA has been
identified in malignant tumors. Furthermore, an allelic loss of the
interferon-β gene and an endogenous mutation in the p53 tumor
suppressor gene have only been detected in malignant tumors
(14). A study by Go et al
(15), examined the histological and
molecular characteristics of seven cases of malignant
transformation of RRP to squamous cell carcinoma (three of which
demonstrated tracheal involvement). The authors revealed that
spontaneous transformation of RRP to squamous cell carcinoma was
not characterized by a consistent temporal histological progression
from squamous papilloma to severe dysplasia and then to squamous
cell carcinoma. HPV 6 and 11 are the most common types of HPV
associated with RRP. However, the HPV status may be altered during
malignant transformation. HVP types 16, 18, 31, 35 and 51 are
rarely identified in cases of RRP and RRP-associated carcinomas
(15). Furthermore, the p53 status is
not considered to be a molecular marker for malignant
transformation and its expression is variable in papillomas and
carcinomas (15).
The symptoms of tracheal papilloma are usually
attributed to airway obstruction. Patients often present with
wheezing, dyspnea, cough, hemoptysis and obstructive pneumonia.
Occasionally, tracheal papilloma is masked by other respiratory
diseases, such as asthma (16). In
all tracheal papilloma patients, including the patient of the
present study, the disease is diagnosed by bronchoscopy. In
addition, helical CT is a useful tool for determining the location
of the papilloma. Squamous cell carcinoma may be difficult to
distinguish from papillomas with dysplasia on the basis of
cytological specimen findings. Therefore, histopathological
examination is required (13).
Fluorine-18 fluorodeoxyglucose-positron emission tomography
(FDG-PET) is more suitable for determining lung cancer staging, and
particularly nodal staging, compared with CT. However, to the best
of our knowledge, the use of FDG-PET or PET/CT to detect malignant
transformation of squamous cell papilloma in the lungs has not been
previously reported. Szyszko et al (17) and Pipavath et al (18) detected benign RRP tumors in two
patients and identified that benign papilloma and enlarged lymph
nodes may exhibit marked FDG uptake. The standardized uptake value
(SUV) for lungs is 8.4, with a maximum SUV of 13. The SUVs for the
right hilar and precarinal mediastinal lymph nodes are 4.5 and 5,
respectively (17,18).
Since RRP is a rare disease, large-scale trials
concerning RRP-targeted therapies are limited, and the literature
mainly includes case reports. RRP in the trachea is primarily
treated by surgery and resection techniques, including tracheotomy
and bronchoscopy with excision. Other treatments include repeated
laser therapy and photodynamic therapy with photosensitizing
agents, such as intralesional cidofovir, dihematoporphyrin ether,
systemic and intralesional interferon, acyclovir, indole
3-carbinol, cimetidine and retinoic acid (13). In addition, a previous study described
the case of a 32-year-old male with tracheal papilloma who was
treated with the vascular endothelial growth factor inhibitor,
bevacizumab (19). However, the
aforementioned treatments are associated with a high incidence of
recurrence.
The present study described a rare case of malignant
transformation of a solitary squamous cell papilloma in the
trachea. To the best of our knowledge, this is the first reported
study to treat a patient with this indication using radiotherapy.
Following treatment with a radiation dose of 36 Gy, a CT scan
revealed a decrease in the size of the tumor from 5.6×3.0×4.7 cm to
5.4×2.5×4.5 cm. Bronchofiberscopy confirmed the tumor reduction.
Furthermore, the tumor was not detectable by CT one month after
radiotherapy. These observations indicate that this type of tumor
is sensitive to radiation. In addition, the findings of the present
study provide evidence for the treatment of RRP of the lung. Unlike
the findings of previous studies on non-small-cell lung cancer and
RRP of the lung (7,9,18), CT
during the follow-up examination revealed calcification in the
mediastinum where the swollen nodule used to reside.
References
|
1
|
Shibuya H, Kutomi T, Kujime K, et al: An
adult case of multiple squamous papillomas of the trachea
associated with human papilloma virus type 6. Inter Med.
47:1535–1538. 2008. View Article : Google Scholar
|
|
2
|
Popper HH, Wirnsberger G, Jüttner-Smolle
FM, et al: The predictive value of human papilloma virus (HPV)
typing in the prognosis of bronchial squamous cell papillomas.
Histopathology. 21:323–330. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Harris K and Chalhoub M: Tracheal
papillomatosis: what do we know so far? Chron Respir Dis.
8:233–235. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Harman EM and Mosenifar Z: Recurrent
respiratory papillomatosis. http://emedicine.medscape.com/article/302648-overview2003
Accessed. December 28–2013.
|
|
5
|
Lott DG and Krakovitz PR: Squamous cell
carcinoma associated with intralesional injection of cidofovir for
recurrent respiratory papillomatosis. Laryngoscope. 119:567–570.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Armstrong LR, Derkay CS and Reeves WC:
Initial results from the national registry for juvenile-onset
recurrent respiratory papillomatosis. RRP Task Force. Arch
Otolaryngol Head Neck Surg. 125:743–748. 1999. View Article : Google Scholar
|
|
7
|
Paganin F, Prevot M, Noel JB, Frejeville
M, Arvin-Berod C and Bourdin A: A solitary bronchial papilloma with
unusual endoscopic presentation: case study and literature review.
BMC Pulm Med. 9:402009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Flieder DB, Koss MN, Nicholson A, et al:
Solitary pulmonary papillomas in adults: a clinicopathologic and in
situ hybridization study of 14 cases combined with 27 cases in the
literature. Am J Surg Pathol. 22:1328–1342. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hasegawa Y, Sato N, Niikawa H, Kamata S,
Sannohe S, Kurotaki H, Sasaki T and Ebina A: Lung squamous cell
carcinoma arising in a patient with adult-onset recurrent
respiratory papillomatosis. Jpn J Clin Oncol. 43:78–82. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Guillou L, Sahli R, Chaubert P, et al:
Squamous cell carcinoma of the lung in a nonsmoking, nonirradiated
patient with juvenile laryngotracheal papillomatosis. Evidence of
human papillomavirus-11 DNA in both carcinoma and papillomas. Am J
Surg Pathol. 15:891–898. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
DiMarco AF, Montenegro H, Payne CB Jr and
Kwon KH: Papillomas of the tracheobronchial tree with malignant
degeneration. Chest. 74:464–465. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lioulias A, Misthos P, Papagiannakis G, et
al: Malignant conversion of a solitary papilloma in the distal
trachea: report of a case. Can Respir J. 7:375–376. 2008.
|
|
13
|
Lang TU, Khalbuss WE, Monaco SE and
Pantanowitz L: Solitary tracheobronchial papilloma: Cytomorphology
and ancillary studies with histologic correlation. Cytojournal.
8:62011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rady PL, Schnadig VJ, Weiss RL, et al:
Malignant transformation of recurrent respiratory papillomatosis
associated with integrated human papillomavirus type 11 DNA and
mutation of p53. Laryngoscope. 108:735–740. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Go C, Schwartz MR and Donovan DT:
Molecular transformationg of recurrent respiratory papillomatosis:
viral typing and P53 overexpression. Ann Otol Rhinol Laryngol.
112:298–302. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim S, Park JK, Park SJ, et al: Solitary
bronchial squamous papilloma presenting as a plaque-like lesion in
a subject with asthma. Am J Resp Crit Care Med. 183:555–556. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Szyszko T, Gnanasegaran G, Barwick T, et
al: Respiratory papillomatosis of lung and F-18 FDG PET-CT. Clin
Nucl Med. 8:521–522. 2009. View Article : Google Scholar
|
|
18
|
Pipavath SN, Manchanda V, Lewis DH,
Schmidt RA, et al: 18F FDG-PET/CT findings in recurrent respiratory
papillomatosis. Ann Nucl Med. 22:433–436. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nagel S, Busch C, Blankenburg T and
Schütte W: Treatment of respiratory papillomatosis - a case report
on systemic treatment with bevacizumab. Pneumologie. 63:387–389.
2009.[(In German)]. View Article : Google Scholar : PubMed/NCBI
|