Introduction
Squamous cell and adenocarcinoma are the two most
common types of esophageal malignancies, whereas esophageal
leiomyosarcoma is a rare type of tumor, accounting for <1% of
all malignant esophageal tumors (1,2). Since the
first case of esophageal leiomyosarcoma was reported in 1902
(3), >165 cases of esophageal
leiomyosarcoma have been described in the literature (4). Leiomyosarcomas are characterized by slow
growth and late metastases and thus, exhibit a better prognosis
than squamous cell carcinoma of the esophagus (5). The one-, three- and five-year survival
rates of esophageal leiomyosarcoma in the Chinese population are
60.3, 42.8 and 32.1%, respectively (5). The most common symptom observed at
diagnosis is progressive dysphagia which occurs in 64.7–90.0% of
esophageal leiomyosarcoma patients. Other symptoms include
retrosternal/back pain, weight loss and emesis (6,7). The
development of definite treatment strategies is difficult due to
the rarity of these tumors. Currently, surgical resection is the
first-line treatment (6); however,
surgical resection is not suitable for all patients. Although
leiomyosarcoma is not sensitive to radiation, radiotherapy can be
used to control the tumor effectively by appropriately increasing
the radiation dose (8–12). The present study describes a case of
leiomyosarcoma of the esophagus that was treated with radiation,
rather than surgery. In addition, the current study conducted a
review the relevant literature. Written informed consent was
obtained from the patient.
Case report
In May 2009, a 48-year-old woman presented with 6 kg
weight loss in two months and a six-month history of dysphagia to
solids, which had been aggravated for two months, at the Shandong
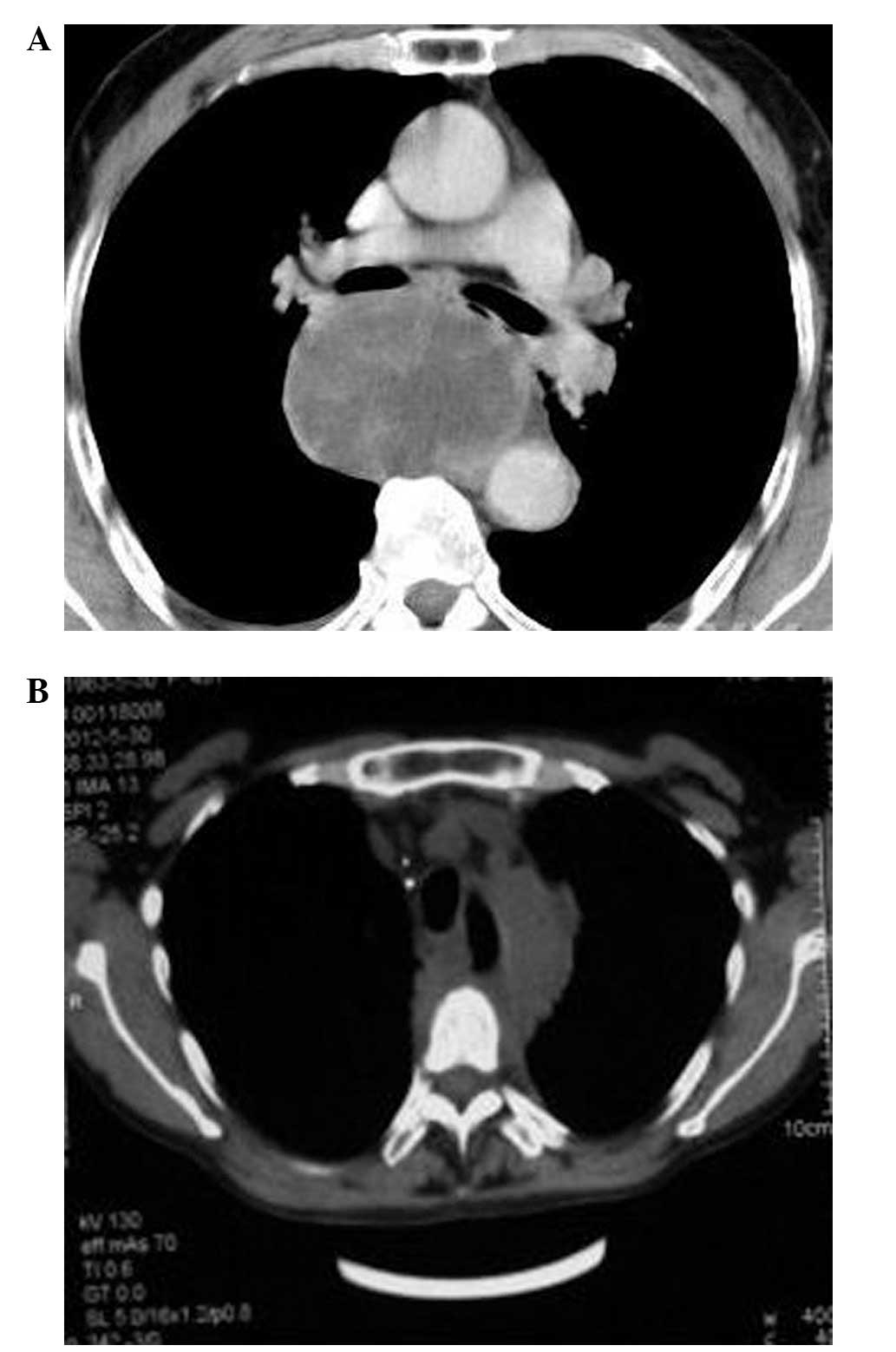
Cancer Hospital and Institute (Jinan, China). Computerized
tomography (CT) scanning of the chest revealed the presence of a
round soft tissue mass with a cross-sectional diameter of 65×40 mm,
located at the posterior wall of the esophagus (Fig. 1A). In addition, upper esophageal
dilation was observed, with a diameter of ∼90 mm between the upper
and lower esophagus. Furthermore, barium studies and esophagoscopy
demonstrated that the lesion was located in the lower esophagus,
15–25 cm from the upper gum margin. A biopsy specimen of the mass
was obtained during esophagoscopy and used to determine a diagnosis
of poorly differentiated esophageal leiomyosarcoma. Histological
examination of the tumor revealed markedly anaplastic spindle cells
with elongated nuclei. On immunohistochemistry, the tumor cells
were positive for vimentin and smooth muscle actin, and negative
for cytokeratin, epithelial membrane antigen, S-100 and C-kit. Due
to the large tumor volume and infiltration of the upper esophagus
resection was not performed. The patient subsequently received
intensity-modulated radiotherapy (IMRT) (60 Gy/30 fractions) at the
Shandong Cancer Hospital and Institute between June 1 and July 20,
2009.
After one month of IMRT, a CT scan revealed that the
lesion was not significantly reduced in size; however, the symptom
of dysphagia was improved. Six months later, the CT scans indicated
that the tumor was significantly reduced in size (Fig. 1B); thus, the patient was able to
consume a normal diet, resulting in a weight increase of 5 kg.
Follow-up examinations were performed for two years, which revealed
that the tumor had significantly decreased in size, and at the
final follow-up the patient was asymptomatic with no identified
tumor recurrences.
Discussion
Esophageal leiomyosarcoma is a rare type of
malignant tumor, accounting for <1% of all esophageal
malignancies (13). Dysphagia is the
predominant clinical manifestation in patients suffering from an
esophageal leiomyosarcoma (4), which
occurs in 64.7–90.0% of patients (7).
Other symptoms include retrosternal/back pain, weight loss and
emesis. Tumor features include infiltration of the esophageal wall
and expansive growth; therefore, foreign invasion is less commonly
identified (7). Furthermore, previous
studies have reported that the obstructive symptoms are
proportional to tumor size; therefore, early symptoms of
obstruction are not evident and the majority of patients presented
significant obstructive symptoms when the tumor was large (14,15). In
addition, the preoperative misdiagnosis rate is as high as 82%. The
majority of cases are finally diagnosed by performing an esophageal
biopsy and immunohistochemical analyses (1). Additionally, esophagogram, computed
tomography (CT), glucose positron emission tomography/CT and
endoscopic ultrasonography may also aid diagnosis (16). However, distinguishing leiomyosarcomas
from other esophageal neoplasms remains difficult (17). Stelow et al (18) recently reported that endoscopic
ultrasound-guided fine-needle aspiration (EUS-FNA) may present a
safe and accurate method for distinguishing the leiomyosarcoma from
other esophageal tumors and may be used to guide therapy. In the
current study, leiomyosarcoma was diagnosed by EUS-FNA.
The detection rate of esophageal leiomyosarcoma
using barium esophagography has been reported to be 64–68%. The
results of barium studies commonly reveal large intramural masses
with a marked exophytic component and often contain areas of
ulceration or tracking (7). Using
endoscopic sonography, previous studies have identified esophageal
leiomyosarcomas as well-defined hyperechoic masses arising from the
muscular layer of the esophageal wall (19). Additionally, these tumors may be
recognized on angiography images as hypervascular masses with tumor
vessels, dilated vascular channels or venous lakes, and early
venous drainage. The development of immunohistochemical detection
methods helped to improve the clinical understanding of esophageal
leiomyosarcomas, as well as differentiate between esophageal
stromal tumors and leiomyosarcomas.
Surgery is a safe and effective procedure for the
treatment of esophageal leiomyosarcomas. As lymph node metastasis
is relatively rare in this disease, esophageal leiomyosarcoma
surgery is associated with longer five-year survival rates and,
thus, improved prognosis compared with the surgical treatment of
esophageal cancer (20). Radiotherapy
may be used as adjuvant treatment, in cases where the risk of local
recurrence is considered to be high, for example, in high-grade
tumors, or when limb preservation is important. Limited surgery may
be used to avoid amputation or the excessive loss of tissue,
followed by radiotherapy in order to sterilize the remaining
malignant cells (21–24). It has been reported that completely
resected low-grade soft-tissue tumors do not require additional
treatment (25). In addition,
radiotherapy alone may be recommended in cases where a tumor is
inoperable, recurrent or metastatic disease has occurred or for
palliation (26). Due to the large
volume of the tumor and infiltration of the esophagus, the patient
of the current study underwent radiotherapy alone and surgery was
not performed. Since leiomyosarcomas exhibit poor sensitivity to
radiation, the radiation dose should be increased from the
conventional dose of 60–65 Gy, which is used to treat other tumor
types (23) to 75 Gy. Therefore, the
current patient underwent IMRT. Considering the large size of the
tumor and the low rate of metastasis to the lymph node, the
clinical target volume did not include the lymphatic drainage
area.
Leiomyosarcoma is typically associated with a good
prognosis due to its slow growth and the late occurrence of
metastasis (27). However, due to its
rarity, it is difficult to determine a pre-operative diagnosis and
appropriate treatment strategy for cases of esophageal
leiomyosarcoma. In previous years, leiomyosarcoma was not
considered to be sensitive to radiation; therefore, radical
radiotherapy treatment was rarely administered and a limited number
of reports regarding the use of radiotherapy in the treatment of
leiomyosarcoma exist in the literature (6,24,28). Although leiomyosarcoma has poor
sensitivity to radiation, the tumor may be effectively controlled
by increasing the radiation dose appropriately. As demonstrated in
the present study, three-dimensional conformal radiotherapy and
IMRT may exhibit a sufficient protective effect on vital organs
adjacent to the tumor and may be an effective topical treatment
strategy for patients unable to undergo surgery.
In conclusion, esophageal leiomyosarcoma has an
excellent prognosis, and radical resection may achieve acceptable
results. However, surgery may not be suitable, depending on the
location of the tumor or the occurrence of distant metastases.
Previously, leiomyosarcoma was considered to be insensitive to
radiation and thus, radical radiotherapy treatment was rarely
administered and only a limited number of reports regarding the use
of radiotherapy in the treatment of leiomyosarcoma exist in the
literature. Although leiomyosarcoma exhibits poor sensitivity to
radiation, the tumor may be effectively controlled by increasing
the radiation dose appropriately. In the present study, surgery was
unsuitable for the patient due to the size and location of tumor.
However, the tumor was successfully treated with radiotherapy and
the patient has an excellent prognosis. Radiotherapy should also be
recommended for the treatment of metastatic tumors to prolong
survival in cases exhibiting extensive or unresectable
metastases.
References
|
1
|
Choh JH, Khazei AH and Ihm HJ:
Leiomyosarcoma of the esophagus: report of a case and review of the
literature. J Surg Oncol. 32:223–226. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weinstein EC, Kim YS, Young GJ and
Kasimian D: Leiomyosarcoma of the esophagus. Mil Med. 153:206–209.
1988.PubMed/NCBI
|
|
3
|
Howard WT: Primary sarcoma of the
esophagus and stomach. JAMA. 38:392–399. 1902. View Article : Google Scholar
|
|
4
|
Hatch GF III, Wertheimer-Hatch L, Hatch
KF, et al: Tumors of the esophagus. World J Surg. 24:401–411. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Koga H, Iida M, Suekane H, et al: Rapidly
growing esophageal leiomyosarcoma: case report and review of the
literature. Abdom Imaging. 20:15–19. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rocco G, Trastek VF, Deschamps C, et al:
Leiomyosarcoma of the esophagus: results of surgical treatment. Ann
Thorac Surg. 66:894–896; discussion 897. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Levine MS, Buck JL, Pantongrag-Brown L, et
al: Leiomyosarcoma of the esophagus: radiographic findings in 10
patients. AJR Am J Roentgenol. 167:27–32. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pramesh CS, Pantvaidya GH, Moonim MT, et
al: Leiomyosarcoma of the esophagus. Dis Esophagus. 16:142–144.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gao Y, Wang L and Zhang D: Surgical
treatment of esophageal leiomyosarcoma: a review of the literature
and report of 11 cases. Zhonghua Zhong Liu Za Zhi. 21:470–472.
1999.[(In Chinese)]. PubMed/NCBI
|
|
10
|
Shiraishi M, Takahashi T, Yamashiro M, et
al: A report of leiomyosarcoma of the esophagus. Nihon Ronen
Igakkai Zasshi. 32:286–291. 1995.[(In Japanese)]. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mutrie CJ, Donahue DM, Wain JC, et al:
Esophageal leiomyoma: a 40-year experience. Ann Thorac Surg.
79:1122–1125. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang WX, Gaurav D, Wen L, et al: Pediatric
esophageal leiomyosarcoma: a case report. J Pediatr Surg.
46:1646–1650. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Galandiuk S, Hermann RE, Cosgrove DM and
Gassman JJ: Cancer of the esophagus. The Cleveland Clinic
experience. Ann Surg. 203:101–108. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang Q, Ye T, Jiang W and Lin ZW:
Video-assisted thoracoscopic surgery in the treatment of esophageal
leiomyoma: a report of 39 cases. Zhonghua Wei Chang Wai Ke Za Zhi.
13:145–147. 2010.PubMed/NCBI
|
|
15
|
Lee LS, Singhal S, Brinster CJ, et al:
Current management of esophageal leiomyoma. J Am Coll Surg.
198:136–146. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kimura H, Konishi K, Kawamura T, et al:
Smooth muscle tumors of the esophagus: clinicopathological findings
in six patients. Dis Esophagus. 12:77–81. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Aimoto T, Sasajima K, Kyono S, et al:
Leiomyosarcoma of the esophagus: report of a case and preoperative
evaluation by CT scan, endoscopic ultrasonography and angiography.
Gastroenterol Jpn. 27:773–779. 1992.PubMed/NCBI
|
|
18
|
Stelow EB, Jones DR and Shami VM:
Esophageal leiomyosarcoma diagnosed by endoscopic ultrasound-guided
fine-needle aspiration. Diagn Cytopathol. 35:167–170. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Puli SR, Reddy JB, Bechtold ML, et al:
Staging accuracy of esophageal cancer by endoscopic ultrasound: a
meta-analysis and systematic review. World J Gastroenterol.
14:1479–1490. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Takayama T, Kato H, Tachimori Y, et al:
Treatment of rupture of a liver metastasis from esophageal
leiomyosarcoma. Jpn J Clin Oncol. 26:248–251. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Franklin GO, Antler AS, Thelmo WL and
Rosenthal WS: Esophageal leiomyosarcoma. NY State J Med.
82:1100–1103. 1982.
|
|
22
|
Lin SH, Wang L, Myles B, et al: Propensity
score-based comparison of long-term outcomes with 3-dimensional
conformal radiotherapy vs intensity-modulated radiotherapy for
esophageal cancer. Int J Radiat Oncol Biol Phys. 84:1078–1085.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang J, Han C, Li XN, et al: Short-term
efficacy of intensity-modulated radiotherapy on esophageal
carcinoma. Ai Zheng. 28:1138–1142. 2009.[(In Chinese)]. PubMed/NCBI
|
|
24
|
Perch SJ, Soffen EM, Whittington R and
Brooks JJ: Esophageal sarcomas. J Surg Oncol. 48:194–198. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Markhede G, Angervall L and Sterner B: A
multivariate analysis of the prognosis after surgical treatment of
malignant soft-tissue tumours. Cancer. 49:1721–1733. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Athanasoulis CA and Aral IM:
Leiomyosarcoma of the esophagus. Gastroenterology. 54:271–274.
1968.PubMed/NCBI
|
|
27
|
Zhang BH, Zhang HT and Wang YG: Esophageal
leiomyosarcoma: clinical analysis and surgical treatment of 12
cases. Dis Esophagus. 27:547–551. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Futuri S, Donohoe K, Spaccavento C and
Yudelman I: Rectal leiomyosarcoma: a rare and long-term
complication of radiation therapy. BMJ Case Rep. Oct 14–2014.(Epub
ahead of print). View Article : Google Scholar : PubMed/NCBI
|