Introduction
Since improvements in cancer management have
increased the life expectancy of patients, bone metastases have
become an increasing oncological problem. Patients with bone
metastases of the spine present with pain, spinal cord compression
with neurological deficits and pathological fractures (1). External beam radiation therapy (RT) is a
widely accepted and effective modality for the treatment of spine
metastases, achieving symptom palliation in 50–80% of patients
(2).
Conventional two-dimensional (2D) RT techniques for
spine metastases utilize a single posteroanterior (PA) field or
anteroposterior/posteroanterior (AP/PA) parallel-opposed fields for
thoracic-lumbar-sacral spines or parallel-opposed lateral fields
for cervical spines (3). These
methods are simple and may be readily practiced; however, these
methods do not spare adjacent healthy organs from the harmful
effects of irradiation. Since the survival of patients with spine
metastases continues to improve, a greater number of patients are
at risk of radiation toxicity (4).
Novel advanced RT technologies, including stereotactic body RT and
intensity-modulated RT, provide highly conformal and accurate
irradiation, permitting an increased target dose while reducing the
unnecessary irradiation of normal structures. However, these
technologies are primarily used for selected non-metastatic
patients; in addition, the costs of equipment and treatment limit
their general use (5).
Three-dimensional conformal RT (3DCRT) is positioned
between traditional and recent sophisticated technologies. The
number of patients with metastatic cancer who receive 3DCRT has
increased gradually; however, the beam placement process remains
similar to that of 2DRT (5). Few
studies have aimed to improve dose distribution using 3DCRT in
palliative RT for spine metastases; therefore, the present study
aimed to analyze the dosimetric advantages of 3DCRT plans for
mid-to-low thoracic spine (T-spine) metastases in terms of sparing
adjacent critical organs.
Materials and methods
RT planning data of 10 patients with mid-to-low
T-spine metastases were used for the present dosimetric analysis.
The patients were aged between 50 and 81 years old (median, 73
years old); in total, there were six males and four females.
Patient characteristics, including the primary tumor type and
involved T-spine levels, are presented in Table I. Written informed consent was
obtained from all patients.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Patient no. | Age,
years/gender | Primary tumor | Involved
vertebra |
|---|
| 1 | 50/F | Non-Hodgkin's
lymphoma | T7 |
| 2 | 59/F | Uterine cervix
cancer | T10 |
| 3 | 74/M | Non-small cell lung
cancer | T9 |
| 4 | 69/M | Prostate cancer | T6-7 |
| 5 | 74/M | Non-small cell lung
cancer | T8 |
| 6 | 54/M | Thymic cancer | T7 |
| 7 | 75/M | Gall bladder
cancer | T9-10 |
| 8 | 78/M | Prostate cancer | T8–10 |
| 9 | 81/F | Breast cancer | T8 |
| 10 | 73/F | Non-small cell lung
cancer | T8-9 |
All patients underwent computed tomography (CT)
simulation in the supine position with the arms placed above the
head. A 16-slice CT scanner with a 0.3-cm slice thickness was used
(Brilliance CT Big Bore; Philips Medical Systems, Cleveland, OH,
USA). The clinical target volume included the entire vertebra of
the involved index spine plus one vertebra superior and inferior to
the index spine. The planning target volume was established by
adding a 0.5-cm isotropic set-up margin around the clinical target
volume. The superior and inferior borders of the planning target
volume (PTV) were limited to inter-vertebral spaces. The critical
organs at risk (OARs), including the heart, esophagus, whole lungs
and spinal cord, were delineated. The heart was outlined along with
the pericardial sac; the superior aspect began at the level of the
inferior aspect of the pulmonary artery and extended inferiorly to
the apex of the heart. The contour of the esophagus and spinal cord
was 5 cm above and below the extent of the PTV.
All RT plans were created using the Eclipse
treatment planning system (Varian Medical Systems, Palo Alto, CA,
USA) and 6- or 15-MV photon beams, taking into account
inhomogeneity corrections. A 3DCRT plan composed of one PA field
plus two posterior oblique (mainly 130° and 230°) wedged fields on
each side. The relative contributions of the three fields and the
wedge angle were optimized in order to achieve the most homogeneous
dose distribution in the PTV. For the purpose of the present study,
two 2D plans were retrospectively generated for each patient using
previously registered planning CT data. The 2D plans consisted of a
single PA field or parallel-opposed AP/PA fields. Unequal weighting
(AP:PA, 1:2) was used in the AP/PA plan. The dose normalization
point was the center of the PTV in the 3DCRT and AP/PA plans. This
point was set at the middle of the vertebral body in the single PA
plan based on the International Bone Metastases Consensus Working
Party reference points (3). The
prescription dose was delivered to the PTV margin, so that ≥95% of
the PTV received the prescribed dose. The prescription dose was 30
Gy at 3 Gy per fraction. Representative plans of a typical case are
illustrated in Fig. 1. Actual
treatments used a 3DCRT plan and were performed using a Novalis Tx
system (Varian Medical Systems and BrainLab, Feldkirchen,
Germany).
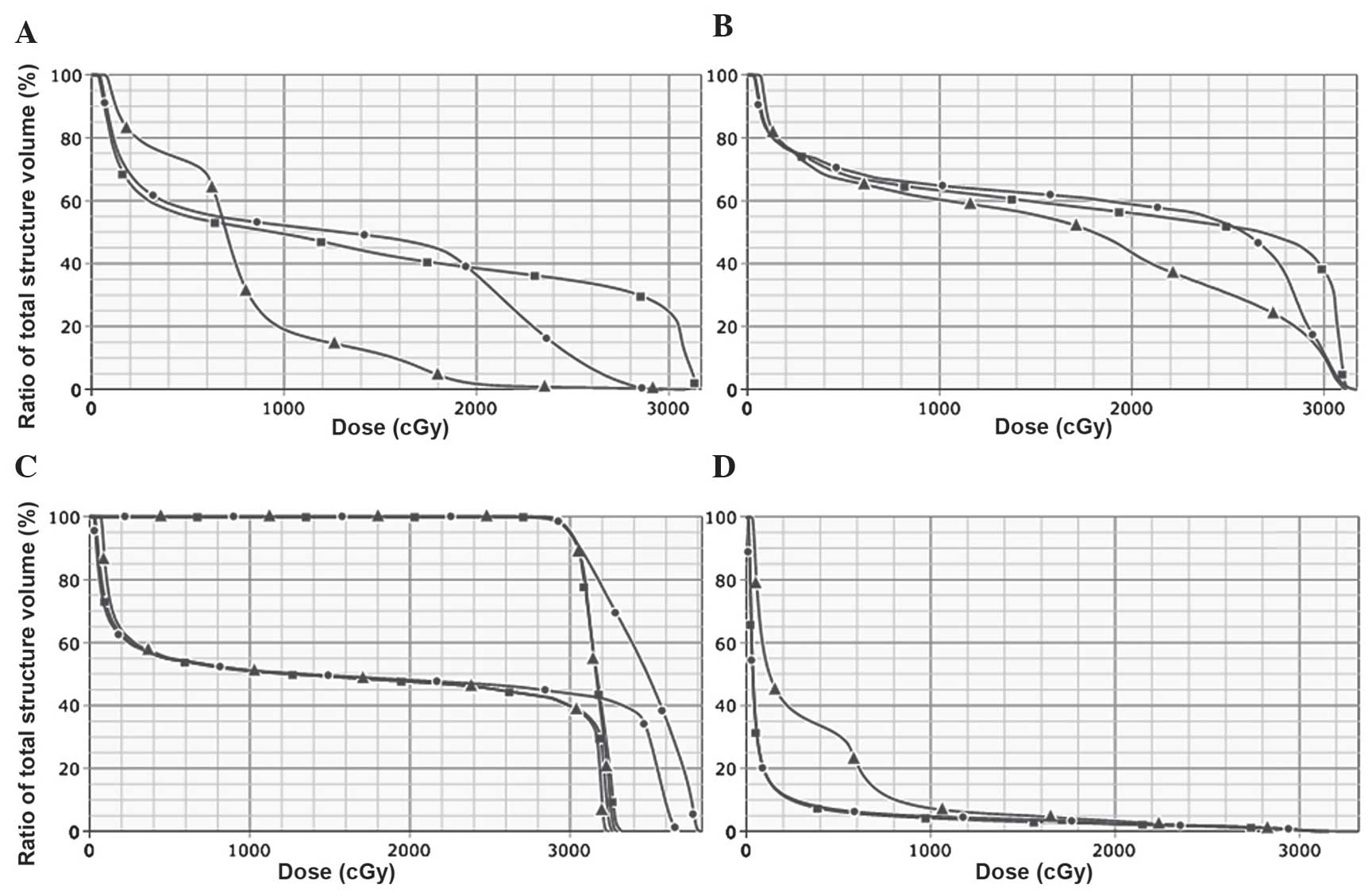
In total, 30 cumulative dose-volume histograms
(DVHs) were generated (three different plans for each of the 10
patients). The maximum and mean doses to the heart, esophagus,
spinal cord, lung and PTV were calculated. The Wilcoxon signed-rank
test was used to analyze the mean differences. Statistical tests
were two-sided and performed using SPSS software version 14.0 (SPSS
Inc., Chicago, IL, USA). A P-value of <0.05 was used to indicate
a statistically significant difference between values.
Results
The comparative DVHs of the three RT plans are shown
in Fig. 2. The calculated maximum or
mean doses administered to the PTV and OARs are listed in Table II. Statistically significant
differences were evident for all of the parameters (single PA vs.
AP/PA; single PA vs. 3DCRT; AP/PA vs. 3DCRT; P<0.05), with the
exception of the mean esophageal dose between the single PA vs.
AP/PA plan (P=0.285).
 | Table II.Calculated doses to the PTV and organs
at risk according to three radiotherapy plans. |
Table II.
Calculated doses to the PTV and organs
at risk according to three radiotherapy plans.
|
|
| Mean dose ± standard
deviation (range), Gy |
|---|
|
|
|
|
|---|
| Region | Dose | Single PA | AP/PA | 3DCRT |
|---|
| PTV | Maximum |
38.8±0.5
(37.9–39.3) |
33.8±0.8
(33.1–35.7) |
32.9±0.6
(32.3–34.3) |
| Heart | Mean |
15.0±3.1
(11.1–19.7) |
17.3±4.3
(12.3–24.5) |
8.5±1.7
(6.6–12.1) |
| Esophagus | Mean |
17.9±2.3
(15.6–23.0) |
18.2±2.2
(15.6–22.5) |
15.3±1.9
(12.6–18.6) |
| Spinal cord | Maximum |
37.5±0.6
(36.8–38.5) |
33.0±0.6
(32.3–34.2) |
32.3±0.4
(31.7–32.9) |
| Lung | Mean |
2.7±0.7
(1.7–4.0) |
2.6±0.7
(1.6–3.9) |
5.1±1.0
(3.6–6.8) |
The reduction in the OAR dose using 3DCRT was most
prominent for the heart; the mean heart dose was 15.0±3.1 Gy in
single PA, 17.3±4.3 Gy in AP/PA and 8.5±1.7 Gy in 3DCRT. When using
3DCRT, the median percentage reduction rate in the mean heart dose
was 38.9% (range, 29.4–58.5%) compared with the single PA plan and
47.5% (range, 34.5–67.1%) compared with the AP/PA plan. In
addition, the median percentage reduction rate in the mean
esophageal dose was 12.8% (range, 4.7–27.9%) compared with the
single PA and 15.6% (range, 5.3–29.1%) compared with the AP/PA
plan. The median percentage reduction rate in the maximum spinal
cord dose was 13.7% (range, 12.1–15.6%) compared with the single PA
plan and 1.9% (range, 0.7–4.0%) compared with the AP/PA plan.
Furthermore, the median percentage reduction rate in the maximum
PTV dose was similar to that of the spinal cord; 14.7% (range,
12.3–17.6%) compared with the single PA plan and 2.9% (range,
1.2–4.0%) compared with the AP/PA plan.
Discussion
Palliative RT for spine metastases has long been
performed using a 2D technique with an X-ray simulator and portal
films; this simple method has advantages in terms of the rapid
initiation of treatment for symptom control (5). However, this technique is suboptimal for
reducing unnecessary radiation exposure to neighboring healthy
tissues (5). The 2D technique is used
as these patients have little prospect for long-term survival;
therefore, late-manifesting complications do not need to be taken
into consideration and the prescribed dose is relatively low when
RT is used for palliative reasons (4). However, prolonged survival is possible
for certain patients with spine metastases, including those with an
oligometastatic status (6,7) or patients with a primary tumor type of
favorable histology, such as breast or prostate (1).
The latest and most sophisticated RT technologies,
including intensity-modulated RT and stereotactic body RT, are
increasingly used by radiation oncology departments (8,9). However,
these techniques are primarily indicated for non-metastatic
cancers. A survey performed in the United States reported that, in
2007, these technologies were used in <5% of metastatic cancer
cases (5). 3DCRT is currently
classified as intermediate in terms of RT technology advancement.
3DCRT is based upon CT simulation, the visualization of tumors and
surrounding anatomy, and an accurate dose-volume calculation
(5). To the best of our knowledge,
limited data exists concerning the use of 3DCRT for patients with
spine metastases and how to optimize beam arrangements and maximize
its ability to spare OARs. A study by Soyfer et al (4) reported that the 3DCRT plan for lumbar
spine metastases was more effective in terms of bowel and spinal
cord exposure compared with the 2D single PA or AP/PA plan. The
present study analyzed cases of T-spine metastases and revealed a
similar dosimetric advantage of 3DCRT in terms of sparing the heart
and esophagus; a reduction in spinal cord exposure was also
demonstrated.
Types of radiation-induced cardiac disease include
pericarditis, congestive heart failure, cardiomyopathy, valve
damage, conduction abnormality, coronary artery disease and
myocardial infarction (10). In
breast cancer, mortality from RT-associated heart disease was
reported to offset the improvement of cancer-specific survival due
to adjuvant RT (11,12). A clear quantitative dose-volume
dependence for the majority of cardiac toxicities remains to be
determined (10). A recent study,
however, suggested that the rates of major coronary events increase
linearly with the mean heart dose by 7.4% per Gy, with no apparent
threshold (13). In addition, it has
been established that various clinical parameters may aggravate the
risk of radiation-induced heart injury; these include age, diabetes
mellitus, smoking, hypertension and the use of cardiotoxic
anthracycline-containing chemotherapy (10,12).
Re-irradiation for painful spine metastases may be required in
patients who achieve no pain relief following initial RT or those
who outlive the duration of the first RT response. A recent
systematic review indicated that the palliative efficacy of
re-irradiation is comparable to that of initial RT (14). The 3DCRT approach used in the present
study reduced the mean heart dose by 40–50% compared with the 2DRT
plans. Minimizing the irradiation dose-volume to the heart may
therefore assist in the prevention of radiation-induced cardiac
toxicities, including mortality. 3DCRT has also been reported to
result in a significant dose reduction to the esophagus (15) and spinal cord (16), although the degree of reduction was
less than that to the heart.
A 2D plan with a single PA field is frequently used
in palliative RT for thoracic and lumbar spine metastases.
Regarding the prescription point in this method, opinions in the
guidelines from the International Bone Metastases Consensus Working
Party were split between the mid-vertebral body and anterior
vertebral body, although concerns regarding toxicity were raised
for the latter (3). A survey
regarding the practice patterns for this RT method concluded that a
significantly higher number of respondents used dose prescription
to the mid-vertebral body (17).
Irrespective of these prescription points, the single PA field is
inferior to AP/PA fields in terms of accomplishing homogeneous
target dose distribution (18). The
International Commission on Radiation Units and Measurements Report
50 recommend a homogeneous dose within 95–107% of the prescribed
dose for the target volume (19). As
expected, the present study revealed that the PTV maximum dose was
higher with the single PA plan than with the AP/PA plan. In
addition, it was demonstrated that 3DCRT could further decrease the
PTV maximum dose compared with the AP/PA plan. The PTV maximum dose
was also associated with a dose to the spinal cord, as it is
located within the target volume.
The mean lung dose was negatively affected by the
use of posterior oblique fields in 3DCRT in the present study;
however, this increase in lung dose was minimal and appeared
insufficient to cause clinical effects (20). 2D plans are performed without CT
simulation, and the dose is usually calculated on a single
transverse contour taken through the center of the target (21). The actual differences between 2D and
3DCRT plans with regard to dose to the PTV and OARs may be greater
than those reported in the present study.
In conclusion, the present study established that,
compared with conventional 2DRT plans, 3DCRT for mid-to-low T-spine
metastases has dosimetric advantages in terms of reducing
unnecessary irradiation to OARs, particularly the heart, and in
achieving a homogeneous target dose. Although the radiation doses
prescribed for palliative treatments are relatively low,
improvements in RT plans are required due to the presence of
diverse clinical factors that may lead to aggravation of
radiation-induced complications.
Acknowledgements
The present study was supported by a grant from the
Soonchunhyang University Research Fund.
References
|
1
|
Coleman RE: Clinical features of
metastatic bone disease and risk of skeletal morbidity. Clin Cancer
Res. 12:6243s–6249s. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lutz S, Berk L, Chang E, Chow E, Hahn C,
Hoskin P, Howell D, Konski A, Kachnic L, Lo S, Sahgal A, et al:
Palliative radiotherapy for bone metastases: An ASTRO
evidence-based guideline. Int J Radiat Oncol Biol Phys. 79:965–976.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chow E, Hoskin P, Mitera G, Zeng L, Lutz
S, Roos D, Hahn C, van der Linden Y, Hartsell W and Kumar E:
International Bone Metastases Consensus Working Party: Update of
the international consensus on palliative radiotherapy endpoints
for future clinical trials in bone metastases. Int J Radiat Oncol
Biol Phys. 82:1730–1737. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Soyfer V, Corn BW, Shtraus N, Schifter D
and Tempelhof H: The advantage of 3D conformal treatment of lumbar
spine metastases in comparison to traditional PA or AP-PA
techniques: Restoring an intermediate niche of therapeutic
sophistication. Radiat Oncol. 8:342013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Guadagnolo BA, Huo J, Liao KP, Buchholz TA
and Das P: Changing trends in radiation therapy technologies in the
last year of life for patients diagnosed with metastatic cancer in
the United States. Cancer. 119:1089–1097. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Badakhshi H, Grün A, Stromberger C, Budach
V and Boehmer D: Oligometastases: The new paradigm and options for
radiotherapy. A critical review. Strahlenther Onkol. 189:357–362.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yeo SG, Kim DY, Kim TH, Jung KH, Hong YS,
Kim SY, Park JW, Choi HS and Oh JH: Curative chemoradiotherapy for
isolated retroperitoneal lymph node recurrence of colorectal
cancer. Radiother Oncol. 97:307–311. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim MJ, Yeo SG, Kim ES, Min CK and Se An
P: Intensity-modulated stereotactic body radiotherapy for stage I
non-small cell lung cancer. Oncol Lett. 5:840–844. 2013.PubMed/NCBI
|
|
9
|
Kim ES and Yeo SG: Volumetric modulated
arc radiotherapy sparing the thyroid gland for early-stage glottic
cancer: A dosimetrical analysis. Oncol Lett. 7:1987–1991.
2014.PubMed/NCBI
|
|
10
|
Gagliardi G, Constine LS, Moiseenko V,
Correa C, Pierce LJ, Allen AM and Marks LB: Radiation dose-volume
effects in the heart. Int J Radiat Oncol Biol Phys. 76:(3 Suppl).
S77–S85. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Darby SC, McGale P, Taylor CW and Peto R:
Long-term mortality from heart disease and lung cancer after
radiotherapy for early breast cancer: Prospective cohort study of
about 300,000 women in US SEER cancer registries. Lancet Oncol.
6:557–565. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sung K, Lee KC, Lee SH, Ahn SH, Lee SH and
Choi J: Cardiac dose reduction with breathing adapted radiotherapy
using self respiration monitoring system for left-sided breast
cancer. Radiat Oncol J. 32:84–94. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Darby SC, Ewertz M, McGale P, Bennet AM,
Blom-Goldman U, Brønnum D, Correa C, Cutter D, Gagliardi G, Gigante
B, Jensen MB, et al: Risk of ischemic heart disease in women after
radiotherapy for breast cancer. N Engl J Med. 368:987–998. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wong E, Hoskin P, Bedard G, Poon M, Zeng
L, Lam H, Vulpe H, Tsao M, Pulenzas N and Chow E: Re-irradiation
for painful bone metastases - a systematic review. Radiother Oncol.
110:61–70. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Werner-Wasik M, Yorke E, Deasy J, Nam J
and Marks LB: Radiation dose-volume effects in the esophagus. Int J
Radiat Oncol Biol Phys. 76:(3 Suppl). S86–S93. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kirkpatrick JP, van der Kogel AJ and
Schultheiss TE: Radiation dose-volume effects in the spinal cord.
Int J Radiat Oncol Biol Phys. 76:(3 Suppl). S42–S49. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nakamura N, Shikama N, Wada H, Harada H,
Nozaki M, Nagakura H, Tago M, Oguchi M and Uchida N: Variability in
the point to which single direct field irradiation is prescribed
for spinal bone metastases: A survey of practice patterns in Japan.
J Radiat Res. 54:1065–1068. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Andic F, Baz Cifci S, Ors Y, Niang U,
Dirier A and Adli M: A dosimetric comparison of different treatment
plans of palliative spinal bone irradiation: analysis of dose
coverage with respect to ICRU 50 Report. J Exp Clin Cancer Res.
28:22009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
International Commission on Radiation
Units and Measurements (ICRU), . ICRU 50: Prescribing, Recording
and Reporting Photon Beam Therapy. ICRU Press; Bethesda, MD:
1993
|
|
20
|
Marks LB, Bentzen SM, Deasy JO, Kong FM,
Bradley JD, Vogelius IS, El Naqa I, Hubbs JL, Lebesque JV,
Timmerman RD, Martel MK and Jackson A: Radiation dose-volume
effects in the lung. Int J Radiat Oncol Biol Phys. 76:(3 Suppl).
S70–S76. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Parker W and Patrocinio H: Clinical
treatment planning in external photon beam radiotherapyRadiation
Oncology Physics: A Handbook for Teachers and Students. Podgoršak
EB: International Atomic Energy Agency; Vienna: pp. 219–272.
2005
|