Introduction
Transitional cell carcinoma (TCC) of the ovary, in
contrast to that of the bladder, is a rare entity and therefore,
studies of recurrence are few in number. The true incidence of TCC
of the ovary remains unclear. TCCs represent a small percentage of
ovarian cancers, and have been demonstrated to be a distinct group,
with differing histological and immunohistological aspects.
However, the clinical presentation of TCC is similar to that of
other types of ovarian carcinoma (1).
Its typical symptoms include abdominal pain, abdominal distension
and pelvic masses, and serum CA-125 is usually positive. The
primary therapeutic approach for TCC is surgery and chemotherapy,
and the consequent patient outcomes are an improvement on those of
other types of common epithelial ovarian cancers (2).
Case report
In 2004, a 55-year-old female was diagnosed with
International Federation of Gynecology and Obstetrics stage IIIc
(3) TCC of the ovary in the
Department of Gynecology in The Affiliated First Hospital of Harbin
Medical University (Harbin, Heilongjiang, China) and underwent
satisfactory cytoreductive surgery consisting of hysterectomy,
bilateral salpingo-oophorectomy, appendectomy and partial
omentectomy. The post-surgical pathological evaluation revealed
that the the ovarian tumor was TCC, grade 3, with involvement of
the appendix. Subsequently, seven cycles of chemotherapy were
administered, consisting of paclitaxel (175 mg/m2;
intravenously over 3 h) followed by carboplatin [area under the
curve (AUC), 5–7.5 mg/ml/min; intravenously over 1 h] on day 1 of a
three-week cycle, and a complete clinical response was achieved.
Thereafter, the patient was followed up without any further
treatment. Nearly two years after the initial therapy, the patient
returned to hospital due to a two-month history of shapeless stool.
The patient's cancer antigen (CA)-125 levels were within the normal
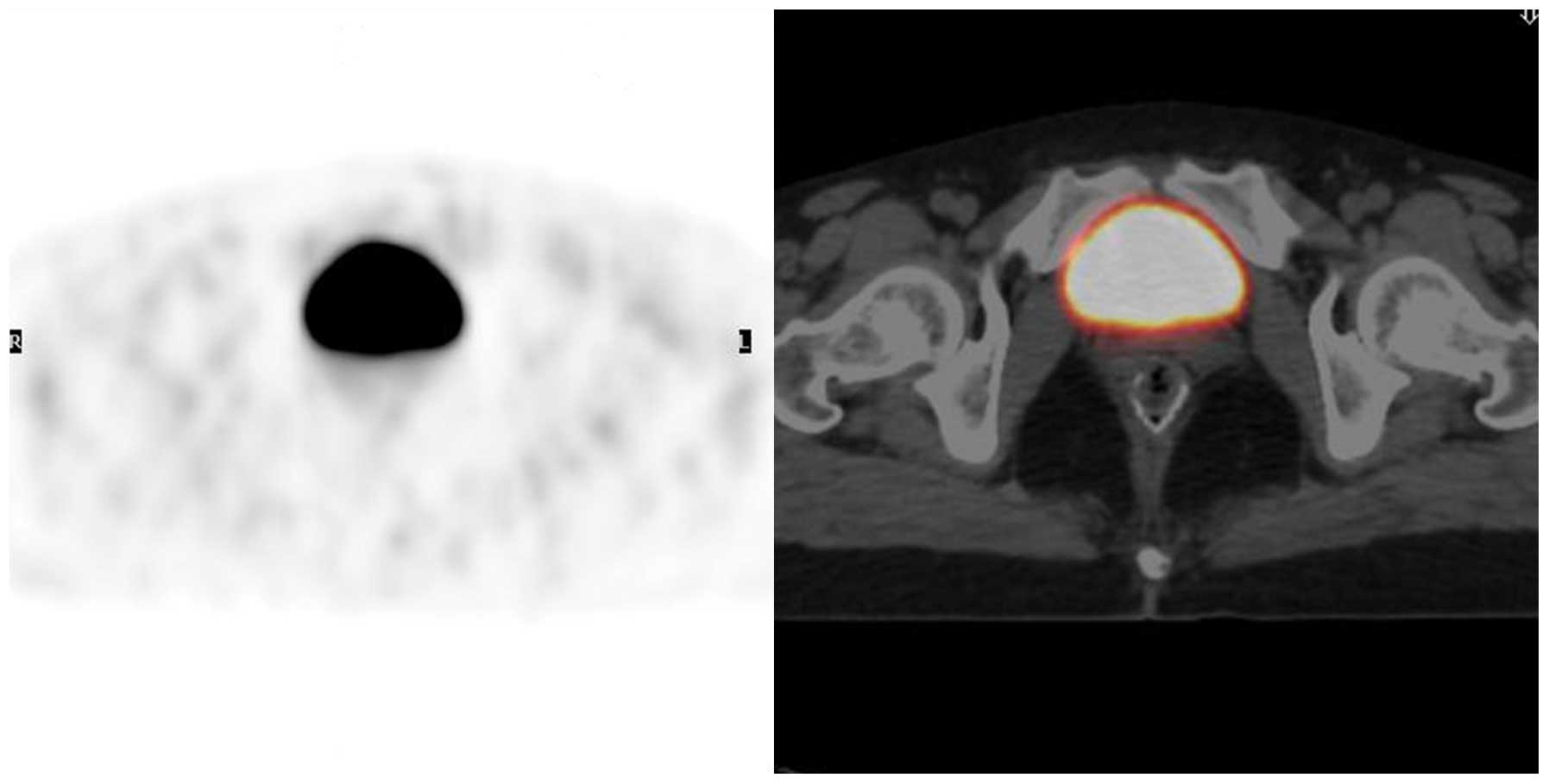
range (normal range, <35 U/ml), and positron emission
tomography-computed tomography (PET-CT) detected metastases of the
rectum, with no other positive sites (Fig. 1). Review of the initial histopathology
using immunohistochemistry revealed a grade 3 (poorly
differentiated) TCC, and involvement of the appendix (stage IIIc,
pT3cNxM0), therefore, recurrent disease accompanied by rectal
metastases was diagnosed nearly two years after the initial therapy
for stage IIIc TCC of the ovary. The patient underwent a partial
resection of the rectum, and the metastatic tumors were completely
resected. Histologically, the tumor of the rectum was a
poorly-differentiated adenocarcinoma that originated from the ovary
and was consistent with a metastasis. Post-operatively, the patient
was administered 3 cycles of paclitaxel and carboplatin-based
cyclic chemotherapy, with the same schedule as used in the initial
treatment. After the three cycles, the symptom of shapeless stool
disappeared and there was no residual tumor site on PET-CT
(Fig. 2). Imaging of the abdomen and
pelvis was normal, and the CA-125 level was also normal. The
patient is currently being followed up by PET-CT examination once
every year, and has been in clinical remission for >8 years
without any additional therapy.
Discussion
TCC of the ovary is a recently recognized subtype of
ovarian cancer that has been described as a primary ovarian
carcinoma with definite urothelial features, but no presence of
benign, metaplastic and/or proliferating Brenner tumors. TCC of the
ovary resembles urothelium rather than ovarian surface epithelium
(mesothelium) (4,5). TCC of the ovary can occur as a component
of a mixed cell type surface epithelial carcinoma, but usually
occurs in pure form (6).
The clinical presentation of TCC and other types of
ovarian carcinoma are indistinguishable (6). Although elevated levels of CA-125 are
clinically useful as a serum marker of tumor progression and
recurrence, CA-125 exhibits high sensitivity but low specificity
for ovarian TCC (1). This was
supported by the present case, where a recurrent normal level of
CA-125 was present. Recent findings (7,8) have
indicated that the p63 antigen is a marker for the differential
diagnosis of TCCs and malignant Brenner tumors, as it was not found
to be expressed in TCCs of the ovary.
A survival benefit may be generated using optimal
surgical resection followed by cisplatin-based chemotherapy
(9–11). In a previous study, the estimated
5-year survival rate following surgery in the entire group of 88
patients was 37%, whereas for patients who received chemotherapy
following resection (76 patients), the survival rate was 41%
(11). Clinical stage, the TCC
component percentage in the primary tumor and the results of
secondary surgery are all factors associated with the survival of
patients who receive chemotherapy. A study by Gershenson et
al (12) indicated that, compared
with poorly-differentiated serous carcinoma, advanced-stage ovarian
TCC was significantly more chemosensitive and was associated with a
better prognosis. In the present case, the advanced-stage patient
underwent successful surgery for a recurrence of TCC with rectal
metastases and experienced an 8-year disease-free survival period,
thus demonstrating the benefits of secondary cytoreductive surgery.
Kommoss et al (9) also
recorded a better prognosis in patients with TCC compared with
those with all other ovarian carcinoma types following standardized
chemotherapy.
18F-fluorodeoxyglucose PET-CT is
increasingly being used in the follow-up of patients with
gynecological malignancies and suspected recurrent disease
(13). In comparison to serum CA-125
assays and conventional imaging (ultrasound/CT/magnetic resonance
imaging), PET-CT has been proven to be more efficient in detecting
ovarian cancer recurrence (14).
PET-CT is useful for the selection of patients for cytoreductive
surgery from those with recurrent ovarian cancer (15). In the present case, TCC with rectal
metastases was detected by PET-CT and proven pathologically.
Thereafter, the patient was followed up by PET-CT annually.
TCC of the ovary is a rare subtype of epithelial
ovarian cancer. Surgery followed by chemotherapy is the primary
therapeutic approach. Although TCCs of the ovary are often of an
advanced stage and recur following initial treatment, patients may
experience a good survival outcome after successful secondary
surgery. Furthermore, PET-CT plays a significant role in detection
and follow-up.
References
|
1
|
Ichigo S, Takagi H, Matsunami K, Murase T,
Ikeda T and Imai A: Transitional cell carcinoma of the ovary
(Review). Oncol Lett. 3:3–6. 2012.PubMed/NCBI
|
|
2
|
Lin CH, Liu FS and Ho ES: Transitional
cell carcinoma of the ovary. Taiwan J Obstet Gynecol. 45:268–271.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Robinson G: XX FIGO World Congress of
Gynecology and Obstetrics, Rome, Italy, 7–12 October 2012. J Fam
Plann Reprod Health Care. 39:502013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cannistra SA: Cancer of the ovary. N Engl
J Med. 351:2519–2529. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gadducci A, Cosio S, Zola P, Landoni F,
Maggino T and Sartori E: Surveillance procedures for patients
treated for epithelial ovarian cancer: A review of the literature.
Int J Gynecol Cancer. 17:21–31. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Eichhorn JH and Young RH: Transitional
cell carcinoma of the ovary: A morphologic study of 100 cases with
emphasis on differential diagnosis. Am J Surg Pathol. 28:453–463.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ceauşu M, Terzea D, Georgescu A, Dobrea C,
Mihai M, Iosif C, Vasilescu F and Ardeleanu C: Transitional cell
tumors of the ovary: A compact group with a heterogeneous
histological and immunophenotypical pattern. Rom J Morphol Embryol.
49:513–516. 2008.PubMed/NCBI
|
|
8
|
Liao XY, Xue WC, Shen DH, Ngan HY, Siu MK
and Cheung AN: p63 expression in ovarian tumours: A marker for
Brenner tumours but not transitional cell carcinomas.
Histopathology. 51:477–483. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kommoss F, Kommoss S, Schmidt D, Trunk MJ,
Pfisterer J and du Bois A: Arbeitsgemeinschaft Gynaekologische
Onkologie Studiengruppe Ovarialkarzinom: Survival benefit for
patients with advanced-stage transitional cell carcinomas vs. other
subtypes of ovarian carcinoma after chemotherapy with platinum and
paclitaxel. Gynecol Oncol. 97:195–199. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tazi EM, Lalya I, Tazi MF, Ahellal Y,
M'rabti H and Errihani H: Transitional cell carcinoma of the ovary:
A rare case and review of literature. World J Surg Oncol. 8:982010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Silva EG, Robey-Cafferty SS, Smith TL and
Gershenson DM: Ovarian carcinomas with transitional cell carcinoma
pattern. Am J Clin Pathol. 93:457–465. 1990.PubMed/NCBI
|
|
12
|
Gershenson DM, Morris M, Burke TW,
Levenback C, Kavanagh JJ, Fromm GL, Silva EG, Warner D and Wharton
JT: Combined cisplatin and carboplatin chemotherapy for treatment
of advanced epithelial ovarian cancer. Gynecol Oncol. 58:349–355.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Musto A, Rampin L, Nanni C, Marzola MC,
Fanti S and Rubello D: Present and future of PET and PET/CT in
gynaecologic malignancies. Eur J Radiol. 78:12–20. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Antunovic L, Cimitan M, Borsatti E,
Baresic T, Sorio R, Giorda G, Steffan A, Balestreri L, Tatta R,
Pepe G, et al: Revisiting the clinical value of 18F-FDG PET/CT in
detection of recurrent epithelial ovarian carcinomas: Correlation
with histology, serum CA-125 assay, and conventional radiological
modalities. Clin Nucl Med. 37:e184–e188. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ebina Y, Watari H, Kaneuchi M, Takeda M,
Hosaka M, Kudo M, Yamada H and Sakuragi N: Impact of FDG PET in
optimizing patient selection for cytoreductive surgery in recurrent
ovarian cancer. Eur J Nucl Med Mol Imaging. 41:446–451. 2014.
View Article : Google Scholar : PubMed/NCBI
|