Introduction
POEMS syndrome, a term coined by Bardwick in 1980
(1), is a rare multisystem disorder
associated with the clinical signs of polyneuropathy, organomegaly,
endocrinopathy, monoclonal gammopathy and skin changes (2). However, there is often a delay in
diagnosis due to a lack of overall consideration of the symptoms
(3). Early diagnosis is critical for
POEMS patients to increase survival and reduce the morbidity rate.
However, POEMS syndrome is frequently mistaken for other diseases
due to its rarity and complex multisystemic manifestations, such as
chronic inflammatory demyelinating polyneuropathy (CIDP); it has
been reported that ~60% of patients were misdiagnosed as CIDP
(4). POEMS treatment is similar to
that administered for patients with suspected myeloma. Radiation
therapy is administered for isolated plasma cell tumors. At
present, no placebo-controlled studies investigating POEM
treatments have been performed, however, systemic treatment may be
effective. Currently, the main treatments for POEMS syndrome are
limited to the administration of alkylating agents, such as
cyclophosphamide, in combination with peripheral blood stem cell
transplantation or lenalidomide combined with dexamethasone
(4). The estimated median survival
time of patients with POEMS syndrome is 14 years (4).
Vascular transformation of the lymph node sinuses
(VTS) is a histopathological entity first described by Haferkamp
et al (5) in 1971. Obstruction
of the efferent lymph node vessel or lymph node venous flow is
believed to play an important pathogenetic role in the development
of VTS (6). The present study reports
the case of a patient with enlarged cervical lymph nodes, initially
misdiagnosed as local hemangioma. The clinical manifestations,
diagnostic procedure, auxiliary examinations and reason for
misdiagnosis are also discussed.
Case report
On July 29th, 2013, a 40-year-old female presented
to Tianshi Shangke Hospital (Lishui, China) with a cervical lump,
which was soft without tenderness. An enhanced computed tomography
scan of the neck revealed multiple enlarged venous blood vessel
masses in the right side of supraclavicular area and upper
mediastinum. On September 28th, 2013, the patient was admitted to
Changhai Hospital (Shanghai, China) with progressive lack of
strength in the lower limbs and a unilateral cervical lump which
had been apparent for 8 months. Prior to admission to Changhai
Hospital, the patient had experienced thigh numbness. However, as
walking, urination, squatting and standing without assistance were
unaffected, no special treatment had been offered. The symptoms
persisted and subsequently progressed; 4 months after the onset of
thigh numbness, the patient could no longer walk unaided. No
headaches, photophobia, incontinence or coughing were reported
throughout. The patient's medical history included no underlying
health problems. Upon neurophysical examination on September 28th,
2013, motor strength and deep tendon reflexes were weak. Motor
strength was rated at grade 4 (according to the Medical Research
Council's Scale for Muscle Strength) (7) in the lower extremities, and soft pitting
edema was observed in the ankles. Atrophy of the calf and thenar
muscles and steppage gait were also present. On September 30th,
2013, possible metastases with a rich blood supply were observed on
an enhanced magnetic resonance imaging scan of the region (Fig. 1). However, an ultrasound scan
performed on the same day showed enlargement of the cervical lymph
nodes. Subsequently, local hemangioma was misdiagnosed. On October
11th, 2013, a lumbar puncture was performed for a presumed
diagnosis of peripheral neuropathy. Cerebral spinal fluid analysis
showed an elevated protein level of 1.68 g/l (normal range,
0.15–0.45 g/l), a normal white blood cell count of 1/µl (normal,
≤5/µl), no malignant cells and a normal glucose level. A suspected
diagnosis of CIDP was concluded. However, on October 12th, 2013,
the patient's husband reported that the patient's skin color had
become deeper as the disease had progressed.
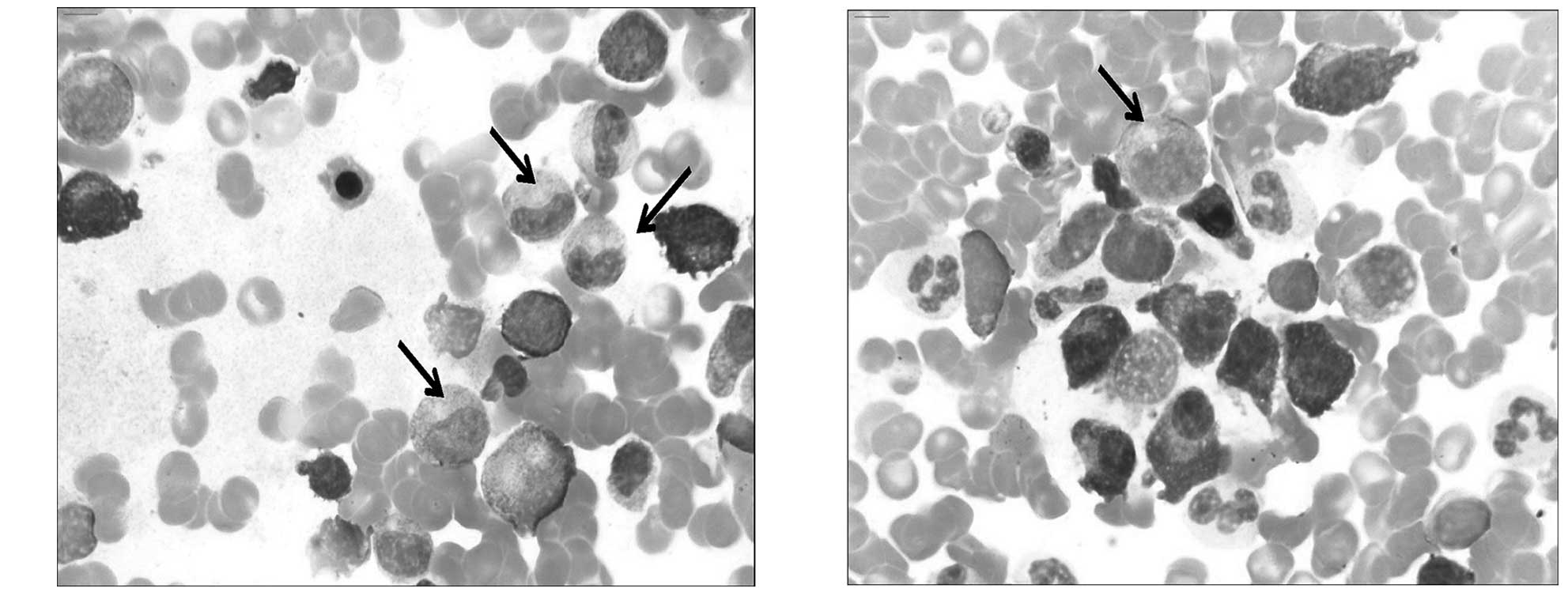
Consequently, a series of auxiliary examinations
were performed on the same day, concentrating on symptoms
associated with POEMS syndrome, was performed. Table I shows the POEMS syndrome-related
symptoms identified in the present patient. This included a
predominance of lymphocytes observed on a bone marrow smear
(Fig. 2).
 | Table I.Symptoms relevant to POEMS in the
present patient. |
Table I.
Symptoms relevant to POEMS in the
present patient.
| Symptom | Evidence |
|---|
| Polyneuropathy | Progressive lack of
strength and numbness in the lower limbs |
| Organomegaly | Lymph node
enlargement |
| Endocrinopathy | Pitting edema in the
anklesa. Prolactin level
of 38.44 µg/l (normal range, 1.39–24.20 µg/l) and
adrenocorticotropic hormone level of 75.78 pmol/ml (normal range,
4.00–22.00 pmol/ml) |
| Monoclonal
gammopathy | Bone marrow puncture
revealed a predominance of lymphocytes |
| Skin changes | Skin color of the
patient deepened as the disease progressed |
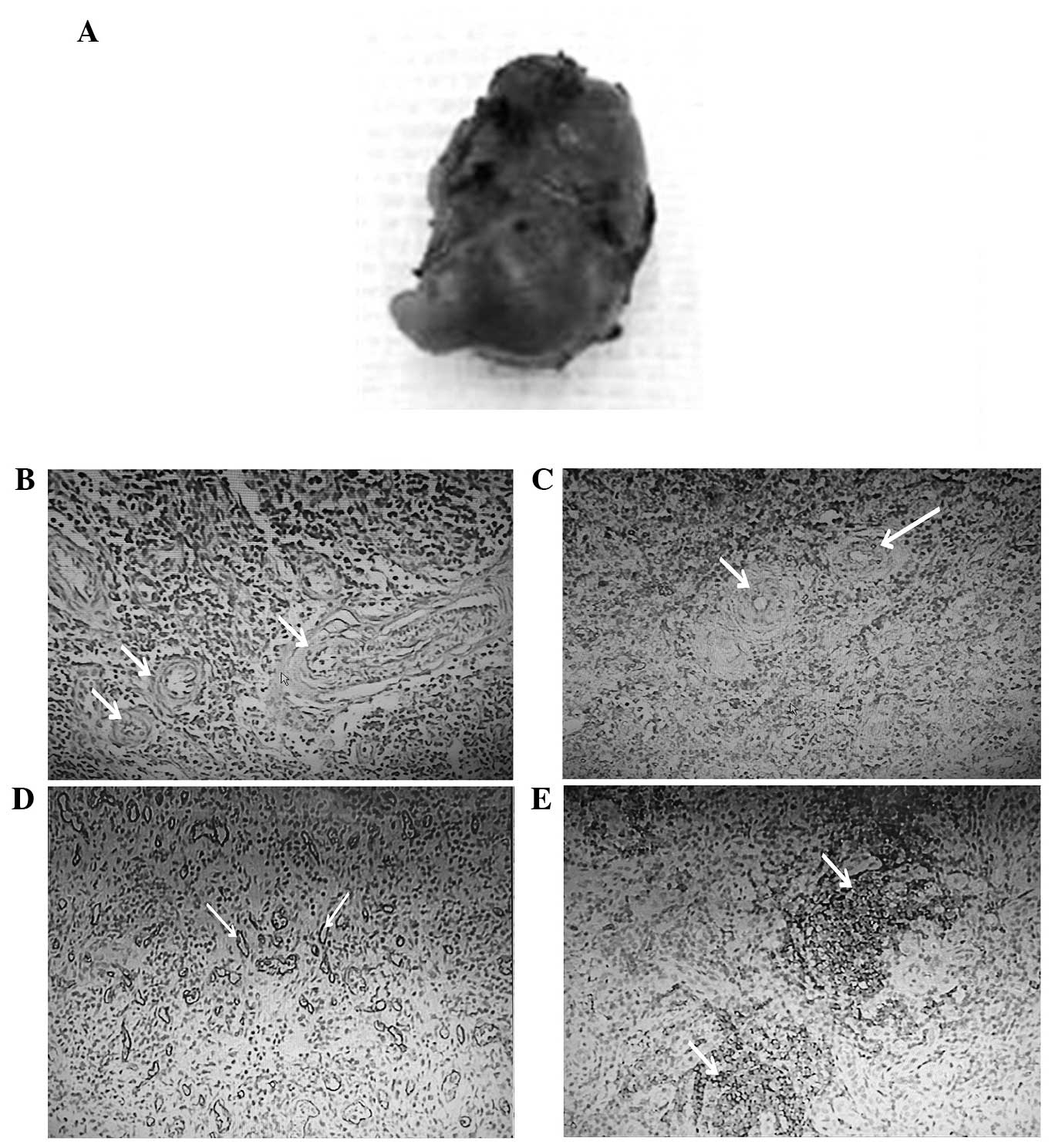
To clarify the characteristics of the mass, a biopsy
of the superficial lymph node was performed on October 23rd, 2013
(Fig. 3A). This was diagnosed as VTS
(Fig. 3B and C) by hematoxylin and
eosin staining and CD31 immunostaining as CD31 staining was
observed in the blood vessels of the lymph node sinuses (Fig. 3D and E). However, the biopsy result
did not account for all the symptoms that the patient possessed,
such as the weakness in the lower limbs. The patient was
administered glucocorticoids (20 mg prednisone acetate, daily). At
the most recent follow-up examination, in December 2014, a slight
improvement in the patient's symptoms was observed and at the time
of writing the patient remained alive.
Discussion
POEMS syndrome is a rare condition characterized by
polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy
and skin lesions (8). The diagnosis
is based on a combination of clinical and laboratory features, and
misdiagnosis may occur if the symptoms are not considered
collectively. In the present study, the patient's clinical
characteristics supported the diagnosis of POEMS syndrome based on
the evidence described in Table I. It
is often challenging to correctly diagnose this condition
initially, as all of the typical features may not appear
concurrently.
The mechanism of POEMS syndrome remains unclear
(9), however, it has been reported
that overproduction of vascular endothelial growth factor (VEGF)
may be of great importance in the pathogenesis of polyneuropathy,
due to the induction of angiogenesis. It has also been demonstrated
that VEGF levels are higher in patients with POEMS syndrome
compared with normal controls (10).
Theoretically, these angiogenic factors may enter the regional
lymph nodes and induce the changes associated with VTS.
VTS is a benign lymph node vascular hyperplastic
lesion; although it is not a true tumor, it may be confused with
cancerous tumors or metastases. VTS is considered to occur
secondary to obstruction of the lymph node venous or efferent
vessels (11,12). In the present case, abnormal clonal
plasma cell proliferation, characteristic of POEMS, was identified
in the bone marrow, suggesting a potentially severe outflow problem
in the lymph circulation.
From a diagnostic perspective, a lump in the neck
region may not appear to be associated with POEMS syndrome, a
systemic disease; therefore, the monistic nature of this case was
not initially apparent. When the case was considered as a whole,
together with the local aspects, in the current patient, it was
deduced that VTS of the bilateral cervical region was a regional
lesion induced by the pathological changes associated with POEMS
syndrome.
In conclusion, the current study presents a rare
association of cervical lymph node enlargement due to VTS in a
patient with POEMS syndrome which, to the best of our knowledge,
has not previously been reported. This case highlights the
importance of detecting VEGF expression in patients with POEMS
syndrome and we recommend that patients are followed up
closely.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundations of China (nos. 81200924 and 81230027),
the Natural Science Foundations of Shanghai (no. 12ZR1427400), the
Outstanding Subject Leaders Project of Shanghai (no. 14XD1403400)
and the Technology Support Project of Shanghai (no.
14140903300).
References
|
1
|
Bardwick PA, Zvaifler NJ, Gill GN, Newman
D, Greenway GD and Resnick DL: Plasma cell dyscrasia with
polyneuropathy, organomegaly, endocrinopathy, M protein, and skin
changes: The POEMS syndrome. Report on two cases and a review of
the literature. Medicine (Baltimore). 59:311–322. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Piradov MA, Suponeva NA, Ginzberg MA,
Nikitin SS, Varlamova EIu, Ryzhko VV, Semochkin SV and Merkulova
DM: POEMS-syndrome: A literature review and case reports. Zh Nevrol
Psikhiatr Im S S Korsakova. 114:4–10. 2014.(In Russian). PubMed/NCBI
|
|
3
|
Briani C, Dalla Torre C, Lessi F,
Cavallaro T, Scarlato M, Ferrari S, Campagnolo M, Lucchetta M,
Cabrini I, Morbin M, Lauria G, Adami F and Manfredi AA: Pentraxin-3
and VEGF in POEMS syndrome: A 2-year longitudinal study. J
Neuroimmunol. 277:189–192. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Latov N: Diagnosis and treatment of
chronic acquired demyelinating polyneuropathies. Nat Rev Neurol.
10:435–446. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Haferkamp O, Rosenau W and Lennert K:
Vascular transformation of lymph node sinuses due to venous
obstruction. Arch Pathol. 92:81–83. 1971.PubMed/NCBI
|
|
6
|
Ostrowski ML, Siddiqui T, Barnes RE and
Howton MJ: Vascular transformation of lymph node sinuses. A process
displaying a spectrum of histologic features. Arch Pathol Lab Med.
114:656–660. 1990.PubMed/NCBI
|
|
7
|
Kim GW, Won YH, Park SH, Seo JH and Ko MH:
Can motor evoked potentials be an objective parameter to assess
extremity function at the acute or subacute stroke stage? Ann
Rehabil Med. 39:253–261. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li J and Zhou DB: New advances in the
diagnosis and treatment of POEMS syndrome. Br J Haematol.
161:303–315. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang X, Chen K, Shi S, Liu Z, Jin Y and
Hu J: A rare case of POEMS syndrome initially presenting with
trigeminal neuralgia. Clin Neurol Neurosurg. 115:89–90. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dispenzieri A: POEMS syndrome: 2014 update
on diagnosis, risk-stratification, and management. Am J Hematol.
89:214–223. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Meysman M, Diltoer M, Raeve HD, Monsieur I
and Huyghens L: Chronic thromboembolic pulmonary hypertension and
vascular transformation of the lymph node sinuses. Eur Resp J.
10:1191–1193. 1997. View Article : Google Scholar
|
|
12
|
Pirola S, Shenjere P and Nonaka D:
Combined usual and nodular types of vascular transformation of
sinuses in the same lymph node. Int J Surg Pathol. 20:175–177.
2012. View Article : Google Scholar : PubMed/NCBI
|