Introduction
Gestational trophoblastic disease (GTD) describes
various neoplastic disorders originating from the trophoblastic
epithelium of the placenta, which are characterized by the distinct
tumor marker β-human chorionic gonadotropin (HCG). Gestational
trophoblastic neoplasia (GTN) is the malignant form of GTD, which
includes invasive moles, choriocarcinoma, placental site
trophoblastic tumors (PSTTs) and epithelioid trophoblastic tumors
(1). Choriocarcinoma is a highly
malignant tumor that may occur during or following any type of
pregnancy, including a hydatidiform mole, normal or ectopic
pregnancy and abortion (2,3). An accurate and prompt diagnosis of
gestational choriocarcinoma is crucial as it is a highly
chemosensitive tumor type and thus, the disease exhibits a good
prognosis, even in advanced stages (4,5). However,
a number of choriocarcinoma cases are often misdiagnosed due to the
atypical symptoms of the disease and a lack of clear radiographical
evidence. Metastasis to the brain is considered a poor prognostic
indicator of choriocarcinoma (6). The
aim of the current study was to present the case of a 29-year-old
female with International Federation of Gynecology and Obstetrics
(FIGO) (7) stage IV gestational
choriocarcinoma that was initially misdiagnosed as pulmonary
tuberculosis, and to discuss the management of gestational
choriocarcinoma with pulmonary and cerebral metastasis.
Case report
On August 15, 2013, a 29-year old female presented
to the local hospital with right-sided chest congestion and pain,
which had lasted for 4 months, accompanied by a mild fever,
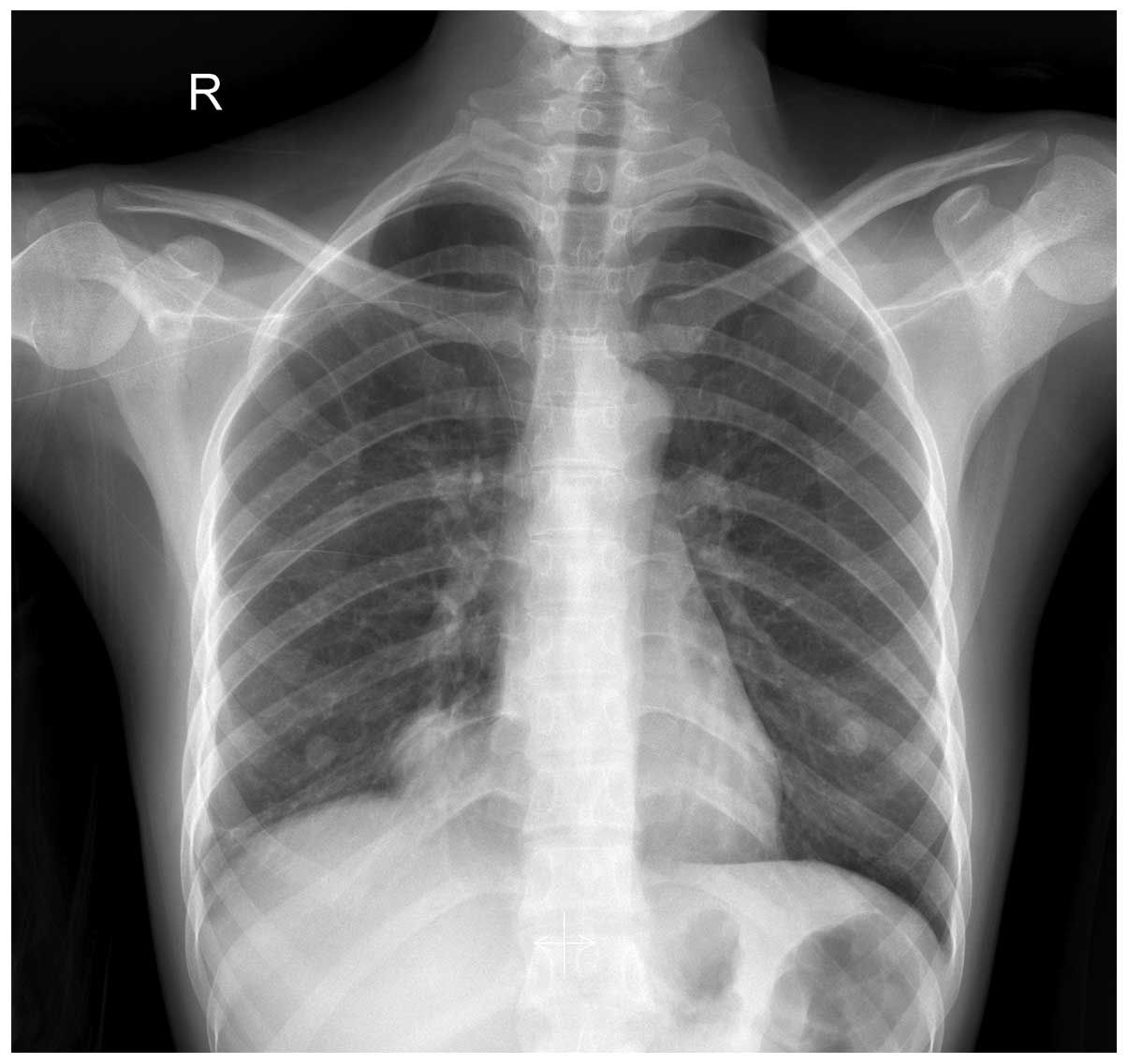
coughing, heavy breathing and palpitations. X-ray examination of
the chest revealed an increased number of lung markings, multiple
bilateral pulmonary nodules and massive right pleural effusion, and
cytopathology revealed hemorrhagic pleural fluid. At the
respiratory clinic of the local hospital, pulmonary tuberculosis
was diagnosed based on the patient's respiratory symptoms and
radiological findings. Subsequently, an anti-tuberculosis regimen
of isoniazid (300 mg, daily), rifampicin (450 mg, daily) and
ethambutol (750 mg, daily) was administered for 3 months. However,
the anti-tuberculosis treatment failed to alleviate the patient's
symptoms and 4 months later, the patient experienced neurological
disturbances, including severe headaches, dizziness and
uncontrolled vomiting.
On December 24, 2013, the patient was transferred to
West China Second Hospital (Chengdu, China). Upon obtaining a
complete clinical history, the patient reported that the date of
her last pregnancy, which was terminated by artificial abortion,
was 3 years ago, with two previous full-term vaginal deliveries.
The patient's menstrual cycle was regular (28–30 days; 4–6 days
duration) with no cessation of menstruation or irregular uterine
bleeding reported. A routine laboratory examination was performed.
Chest radiography showed increased lung markings, diffuse
infiltrates in each lung and a massive right pleural effusion
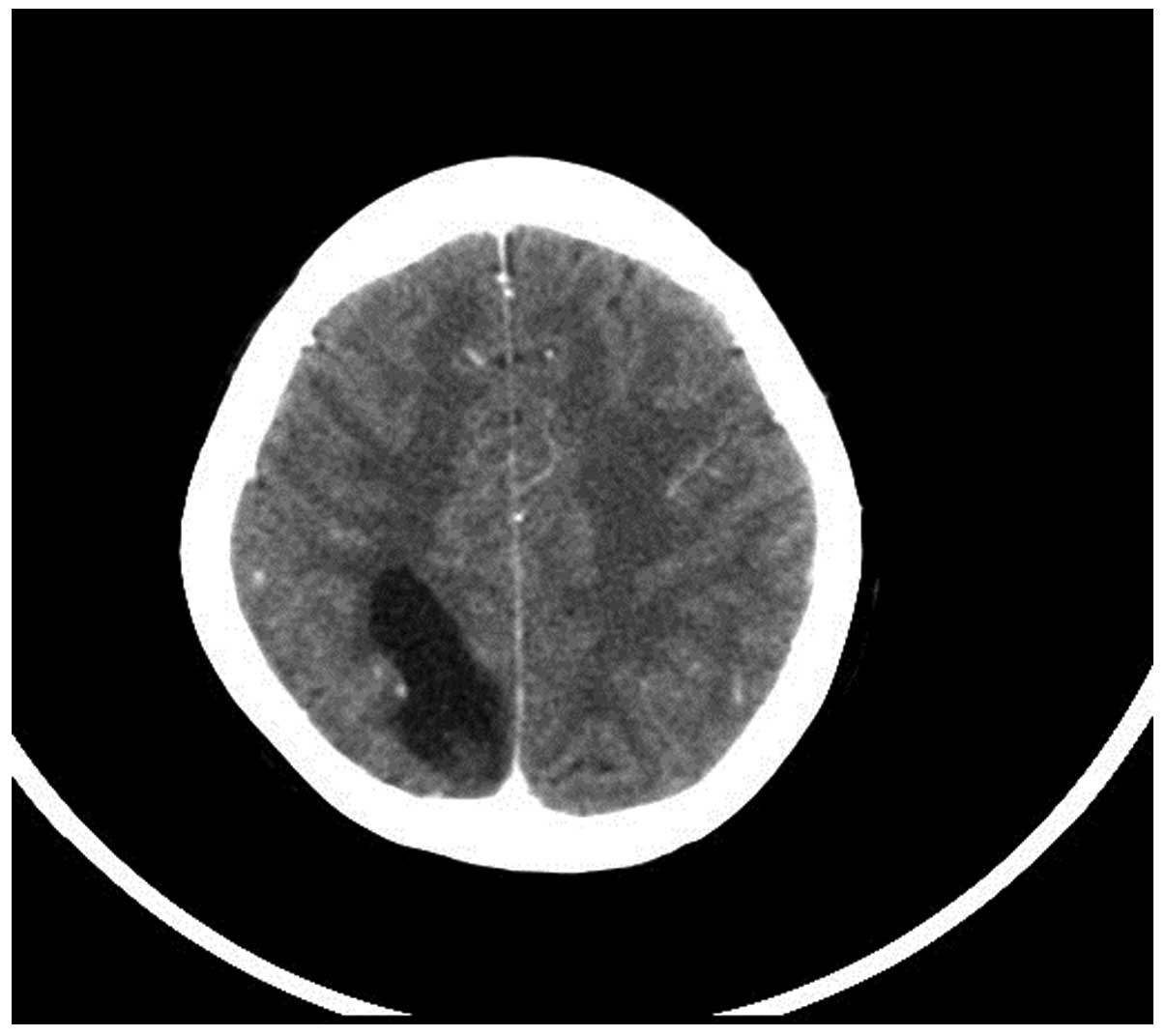
(Fig. 1). Computed tomography (CT)
scans of the lungs and brain revealed irregular multiple bilateral
pulmonary nodules with a maximum diameter of 29 mm, right pleural
effusion and a cystic mass, 43×35×27 mm in size, in the parietal
lobe of the right cerebrum (Fig. 2).
The serum β-HCG level was 655,011.2 mIU/ml (normal level, <2.0
mIU/ml), while other tumor markers, including α-fetoprotein,
carcinoembryonic antigen, carbohydrate antigen 19-9 and cancer
antigen 125, were all within the normal ranges. Transvaginal
sonogram and sonohysterography examination were also performed,
however the results were unremarkable. Following a consultation,
gestational choriocarcinoma with pulmonary and cerebral metastasis
[FIGO stage IV; World Health Organization score, 15 (8)] was diagnosed, which had been
misdiagnosed as pulmonary tuberculosis previously at the local
hospital. After written informed consent was obtained, systemic
multi-agent chemotherapy was administered (Table I). Additionally, the patient underwent
whole-brain irradiation and neurological surgery. The patient's
recovery was monitored by a series of blood or cerebrospinal fluid
(CSF) β-HCG measurements (Table I),
chest X-ray examination, CT and magnetic resonance imaging scans.
After 11 cycles of chemotherapy, the β-HCG level was within the
normal range. The post-chemotherapy period was excellent, without
any major complications. The patient achieved complete remission
with a good outcome and follow-up is ongoing.
 | Table I.Chemotherapeutic regimens and serial
blood or CSF β-HCG levels. |
Table I.
Chemotherapeutic regimens and serial
blood or CSF β-HCG levels.
| Course | Chemotherapy
regimen | Blood β-HCG level,
mIU/ml | CSF β-HCG level,
mIU/ml |
|---|
| 1 | 5-FUa | 65011.2 | 1753.7 |
|
| Act Db |
|
|
|
| MTXc |
|
|
| 2 | 5-FUa |
1420.0 | 14.6 |
|
| Act Db |
|
|
|
| MTXc |
|
|
| 3 | 5-FUa | 63.7 | 7.2 |
|
| Act Db |
|
|
|
| MTXc |
|
|
| 4 | 5-FUa | 15.7 | 4.7 |
|
| Act Db |
|
|
|
| MTXc |
|
|
| 5 | 5-FUa | 9.3 |
|
|
| Act Db |
|
|
| 6 | 5-FUa | 3.7 |
|
|
| Act Db |
|
|
| 7 | 5-FUa | 2.9 |
|
|
| Act Db |
|
|
| 8 | EMA/COd,e | 7.7 |
|
| 9 | EMA/COd | <2.0 |
|
| 10 | EMA/COd | <2.0 |
|
| 11 | EMA/COd | <2.0 |
|
Discussion
Choriocarcinoma is a rare, highly malignant neoplasm
of the gestational trophoblast of the placenta, which usually
presents as abnormal uterine bleeding. This tumor often
demonstrates rapid hematogenous spread to multiple organs, and is
associated with high β-HCG levels and a good response to
chemotherapy (4,5,9).
Approximately 30% of choriocarcinoma patients exhibit metastasis at
the time of diagnosis, which may be attributable to the high
affinity exhibited by trophoblastic cells for blood vessels
(10,11). The most common metastatic sites of
choriocarcinoma are the lungs (80%), vagina (30%), pelvis (20%) and
liver (10%). Cerebral metastases occur in ~10% of cases. Despite
the aggressive nature of the disease, a cure remains possible if it
is treated at an early stage, in accordance with well-established
guidelines (12). Notably, following
treatment with multi-agent chemotherapy regimens, ~75% of
choriocarcinoma patients (FIGO stage IV) are expected to achieve
complete or prolonged remission (5,7).
Consequently, an accurate and prompt diagnosis is crucial. In
addition, the early diagnosis of GTN and the timely administration
of chemotherapy may decrease the number of chemotherapy courses
required for treatment.
In the present study, the patient presented with
right-sided chest congestion and pain that had lasted for 4 months,
and was accompanied with a mild fever, coughing, heavy breathing
and palpitations. Notably, the patient's menstrual cycle was
regular without cessation of menstruation or irregular vaginal
bleeding. The patient exhibited no typical symptoms of
choriocarcinoma, and the respiratory symptoms and radiological
findings were similar to that of pulmonary tuberculosis, resulting
in a misdiagnosis and subsequent delay to treatment. The major
failure in the diagnosis of this case was that the patient's serum
β-HCG levels were initially ignored. Therefore, in young females
with symptoms such as pulmonary bleeding or neurological
disturbances following a hydatidiform mole or a normal pregnancy,
even in the absence of abnormal uterine bleeding, serum β-HCG
levels must analyzed and a diagnosis of choriocarcinoma must be
considered.
Multi-agent chemotherapy is the standard treatment
for high-risk choriocarcinoma. At present, the most commonly used
multi-agent treatment regimens are the 5-fluorouracil (5-FU) plus
actinomycin D (Act D) (FA regimen) and the etoposide, methotrexate,
Act D, vincristin and cyclophosphamide (EMA/CO) regimen. The FA
regimen is effective in low- and high-risk GTN patients, but not in
PSTT patients. Additionally, it may be administered as a primary
chemotherapy regimen for the treatment of high-risk GTN patients
(13,14). It is reported that the EMA/CO regimen
is considered to be highly effective for the treatment of high-risk
GTN, as it exhibits good efficacy and is well-tolerated by
patients. In a previous study by Bolis et al (15), the survival rate of high-risk patients
treated with the EMA/CO regimen was 88%, and 76% of these patients
were alive with no evidence of disease after 5.5 months. Patient
survival and complete response to the EMA/CO regimen are affected
by a number of factors, such as liver metastasis, antecedent
pregnancy and the histopathological diagnosis of choriocarcinoma.
The most severe reported toxicity associated with EMA/CO treatment
was grade 3–4 leukopenia and febrile neutropenia (16). Brain metastases with or without
oncotic aneurysms may be rapidly controlled by the administration
of immediate whole-brain irradiation and intrathecal chemotherapy.
Furthermore, surgical intervention may be required in cases of life
threatening hemorrhage. The levels of HCG in the serum and CSF are
good markers for determining the effect of therapy. However, HCG
levels in the CSF may decrease slowly without affecting prognosis
(17–19).
In the present study, the patient achieved complete
remission following combined treatment with systematic multi-agent
chemotherapy, whole-brain radiation therapy and gross total
resection of the brain lesion. This case demonstrates the
importance of rapidly initiating chemo- and radiotherapy for FIGO
stage IV gestational choriocarcinoma following diagnosis.
References
|
1
|
May T, Goldstein DP and Berkowitz RS:
Current chemotherapeutic management of patients with gestational
trophoblastic neoplasia. Chemother Res Pract.
2011:8062562011.PubMed/NCBI
|
|
2
|
Berkowitz RS and Goldstein DP: Chorionic
tumors. N Engl J Med. 335:1740–1748. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Monchek R and Wiedaseck S: Gestational
trophoblastic disease: An overview. J Midwifery Womens Health.
57:255–259. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Berkowitz RS and Goldstein DP: Current
advances in the management of gestational trophoblastic disease.
Gynecol Oncol. 128:3–5. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Oranratanaphan S and Lertkhachonsuk R:
Treatment of extremely high risk and resistant gestational
trophoblastic neoplasia patients in King Chulalongkorn Memorial
Hospital. Asian Pac J Cancer Prev. 15:925–928. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Han SN, Amant F, Leunen K, Devi UK, Neven
P, Berteloot P and Vergote I: Treatment of high-risk gestational
trophoblastic neoplasia with weekly high-dose
methotrexate-etoposide. Gynecol Oncol. 127:47–50. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
FIGO Committee on Gynecologic Oncology, .
Current FIGO staging for cancer of the vagina, fallopian tube,
ovary and gestational trophoblastic neoplasia. Int J Gynaecol
Obstet. 105:3–4. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shrivastava S, Kataki AC, Barmon D, et al:
Gestational trophoblastic neoplasia: A 6 year retrospective study.
South Asian J Cancer. 3:33–37. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cole LA, Khanlian SA, Muller CY, Giddings
A, Kohorn E and Berkowitz R: Gestational trophoblastic diseases: 3.
Human chorionic gonadotropin-free beta-subunit, a reliable marker
of placental site trophoblastic tumors. Gynecol Oncol. 102:160–164.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morgan JM and Lurain JR: Gestational
trophoblastic neoplasia: An update. Curr Oncol Rep. 10:497–504.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sierra-Bergua B, Sánchez-Marteles M,
Cabrerizo-García JL and Sanjoaquin-Conde I: Choriocarcinoma with
pulmonary and cerebral metastases. Singapore Med J. 49:e286–e288.
2008.PubMed/NCBI
|
|
12
|
Soper JT, Mutch DG and Schink JCAmerican
College of Obstetricians and Gynecologists: Diagnosis and treatment
of gestational trophoblastic disease: ACOG Practice Bulletin No.
53. Gynecol Oncol. 93:575–585. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhao Y, Zhang W and Duan W: Management of
gestational trophoblastic neoplasia with 5-fluorouracil and
actinomycin D in northern China. J Reprod Med. 54:88–94.
2009.PubMed/NCBI
|
|
14
|
Manopunya M and Suprasert P: Resistant
gestational trophoblastic neoplasia patients treated with
5-fluorouracil plus actinomycin D. Asian Pac J Cancer Prev.
13:387–390. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bolis G, Bonazzi C, Landoni F, Mangili G,
Vergadoro F, Zanaboni F and Mangioni C: EMA/CO regimen in high-risk
gestational trophoblastic tumor (GTT). Gynecol Oncol. 31:439–444.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Turan T, Karacay O, Tulunay G, Boran N,
Koc S, Bozok S and Kose MF: Results with EMA/CO (etoposide,
methotrexate, actinomycin D, cyclophosphamide, vincristine)
chemotherapy in gestational trophoblastic neoplasia. Int J Gynecol
Cancer. 16:1432–1438. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Baertschi E, Notter M, Mironov A, Wernli M
and Bargetzi MJ: Cerebral metastasis in choriocarcinoma a case
report. Praxis. 92:763–768. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Milenković V, Lazović B, Mirković L,
Grujicić D and Sparić R: Brain metastases of choriocarcinoma-a
report on two cases. Vojnosanit Pregl. 70:968–971. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Milenković V, Lazović B, Mačvanski M,
Jeremić K and Hrgović Z: Clinical outcome of a FIGO stage IV
gestational choriocarcinoma. Case Rep Oncol. 6:504–507. 2013.
View Article : Google Scholar : PubMed/NCBI
|