Introduction
Esophageal squamous cell carcinoma (ESCC) is one of
the most common digestive tract cancers, and accounts for
approximately one-sixth of all cancer-associated mortalities
worldwide. There are ~300,000 cases of esophageal cancer
(EC)-associated mortalities annually worldwide (1). The incidence of ESCC is characterized by
distinctive geographic distribution, with half of all cases
worldwide occurring in China. Approximately 70% of patients present
with advanced ESCC at the time of diagnosis and treatment consists
of radiotherapy and chemotherapy, in addition to palliative care
for terminally ill patients. The prognosis for EC is poor, with a
5-year survival rate of ≤20% (2) and
therefore, ESCC continues to result in high mortality rates.
Although various refinements of the conventional therapies for EC,
including surgery, radiotherapy, chemotherapy and their
multidisciplinary applications have been attempted, improvements in
the overall survival rate remain unsatisfactory (3). Therefore, the development of novel
therapies to treat EC are urgently required.
The epidermal growth factor receptor (EGFR) is
involved in multiple signaling pathways, a number of which are
associated with esophageal cancer progression. EGFR is a major
regulator in a variety of physiological processes, including cell
growth, differentiation, apoptosis and cell death (4). In the development of tolerance to
irradiation, an intracellular phosphorylation cascade initiated by
auto-phosphorylation of transmembrane tyrosine kinase receptors,
and of EGFR (also known as HER-1) in particular, has been
recognized as a signaling pathway associated with cell survival
(5). The high expression and mutation
rate of EGFR may result in radiotherapy resistance, leading to a
reduction in radiosensitivity. EGFR is currently being studied as a
potential ESCC therapeutic target (6).
RNA interference (RNAi) is a highly specific method
of gene silencing that utilizes small interfering RNA (siRNA)
molecules complementary to the target sequence (7). These siRNAs bind to gene transcripts,
targeting them for early destruction prior to translation (7). RNAi techniques are already extensively
used in research but also have promising potential for the
development of drugs capable of targeting specific proteins
(8,9),
including EGFR (10). In the present
study, siRNA technology was used to reduce EGFR expression in ESCC
cells, and its effects on cell proliferation and radiosensitivity
were assessed. The results of the present study may provide the
theoretical basis on which to develop novel treatments for
ESCC.
Materials and methods
Cell culture and major reagents
Human ESCC Eca109 cells were purchased from the
Shanghai Institute of Cell Biology (Shanghai, China). The cells
were cultured in RPMI-1640 supplemented with 10% fetal calf serum
(Gibco Life Technologies, Carlsbad, CA, USA) and maintained at 37°C
under a humidified atmosphere of 5% CO2. TRIzol reagent,
liposomes and Lipofectamine 2000 were purchased from Invitrogen
Life Technologies (Carlsbad, CA, USA). The RevertAid First Strand
cDNA Synthesis Kit was purchased from Thermo Fisher Scientific,
Inc. (Pittsburgh, PA, USA) and the Fast HiFidelity PCR kit was
purchased from Tiangen Biotech Co., Ltd. (Beijing, China). The EGFR
primer sequences were designed and synthesized by Invitrogen Life
Technologies, the EGFR primary antibody was purchased from Abcam
(Cambridge, UK), the secondary antibody and the Micro Bicinchoninic
Acid (BCA) Protein Assay Kit were purchased from Thermo Fisher
Scientific, Inc. (Waltham, MA, USA), and the
radioimmunoprecipitation assay (RIPA) protein lysis buffer and Cell
Counting Kit-8 (CCK-8) kit were purchased from Beyotime Institute
of Biotechnology (Guangzhou, China).
Design and synthesis of siRNAs
A total of three siRNA pairs targeting the EGFR gene
were designed and synthesized by Invitrogen Life Technologies. The
sequences used were as follows: EGFR-siRNA1 sense, UGA UCU GUC ACC
ACA UAA UUA CGG and antisense, CCC GUA AUU AUG UGG UGA CAG AUCA;
EGFR-siRNA2 sense, UUA GAU AAG ACU GCU AAG GCA UAGG and antisense,
CCU AUG CCU UAG CAG UCU UAU CUAA; EGFR-siRNA3 sense, UUU AAA UUC
ACC AAU ACC UAU UCCG and antisense, CGG AAU AGG UAU UGG UGA AUU
UAAA.
Cell transfection
The cells were divided into 4 groups: The
EGFR-siRNA-treated group, the positive siRNA control group, the
non-targeting siRNA-treated group (negative control) and the
untreated control group (blank). Eca109 cells were seeded into
six-well plates at a density of 5×105 cells/well. When
the cells reached 80–90% confluency, negative control siRNA
(Guangzhou RiboBio Co., Ltd., Guangzhou, China) or EGFR-siRNA
(final concentration, 50 nmol/l; Guangzhou RiboBio Co., Ltd.) was
transfected according to the Lipofectamine 2000 transfection
instructions. The transfection efficiency was determined using
fluorescently labeled siRNA and an Olympus IX70 Inverted
Fluorescent Microscope (Olympus Corporation, Tokyo, Japan). The
cells were irradiated prior to harvest for RNA and protein
measurements, following transfection for 48 h.
Reverse transcription-polymerase chain
reaction (RT-PCR) to detect EGFR mRNA expression
The total RNA was extracted using TRIzol reagent and
then reverse transcribed into cDNA using the RevertAid First Strand
cDNA Synthesis Kit. β-actin was selected as an internal reference
gene (1). The EGFR primers
(Invitrogen Life Technologies) were as follows: Forward (F), 5′-AAA
GAC CTG TAC GCC AAC ACAG-3′; and reverse (R), 5′-TTT TAG GAT GGC
AAG GGA CTTC-3′, which amplified a fragment of 244 base pairs (bp).
The cycling conditions consisted of 94°C pre-incubation for 4 min,
followed by 30 cycles of denaturation at 94°C for 30 sec, annealing
at 60°C for 30 sec and extension at 72°C for 1 min, followed by a
final extension at 72°C for 10 min (2). The internal reference (β-actin) gene
primers were F 5′-AAA GAC CTG TAC GCC AAC ACAG-3′ and R 5′-TTT TAG
GAT GGC AAG GGA CTTC-3′, which amplified a fragment of 556 bp.
Equal volumes of the PCR products were subjected to electrophoresis
on 2% agarose gels and fragments were visualized by ethidium
bromide staining. The grayscale images of the PCR amplification
products were analyzed using a gel imaging system (ChemiDoc XRS+
system) and Quantity One 1-D Analysis software (Bio-Rad
Laboratories, Inc., Hercules, CA, USA).
CCK-8 assay
Eca109 cells were seeded in 96-well plates at a
density of 6×103 cells/well. All experiments were
repeated three times, and the mean results were recorded. The
culture plates were incubated at 37°C with 5% CO2 in a
humidified air incubator. Following treatment with EGFR-siRNA3, the
cells were cultured for a further 24 h, prior to the addition of 10
µl CCK-8 solution (10 µg/l) to every well in the dark. The cells
were incubated for a further 2 h. ELISA was then performed and the
absorbance of each well was measured at 490 nm (OD, optical
density). The cell proliferation inhibition rate was calculated
using the following formula: Cell proliferation inhibition rate (%)
= [(1-treated group OD value)/control group OD value] × 100%.
Western blot analysis
The total protein was extracted from the Eca109
cells using RIPA lysis buffer and the protein concentration was
determined using a Micro BCA Protein Assay Kit. The cell lysates
were centrifuged at 8,000 × g for 5 min. The total proteins (50 µg)
were separated by 10% SDS-PAGE (Invitrogen Life Technologies) and
transferred to a nitrocellulose membrane (Yubo Biology Co., Ltd.,
Shanghai, China). The membrane was blocked for 1 h at room
temperature in phosphate-buffered saline with Tween-20 (PBST; 0.05%
Tween-20; Thermo Fisher Scientific, Inc.) containing 5% skimmed
milk. The membranes were washed three times with PBST, and then
incubated overnight at 4°C with the primary monoclonal rabbit
anti-human EGFR (1:1,000; cat. no. ab76153; Abcam) and rabbit
anti-human β-tubulin (1:500; cat. no. ab179513; Abcam) antibodies
diluted in PBST. Following three washes with PBST, the membranes
were incubated with polyclonal goat anti-rabbit secondary antibody
(1:500; cat. no. 32260; Thermo Fisher Scientific, Inc.) for 1 h at
room temperature. The membranes were washed 4 times with PBST, and
detection was performed using 3,3′-diaminobenzidine (Pierce DAB
Substrate Kit; Thermo Fisher Scientific, Inc.). The band intensity
was digitized and analyzed using Quantity One 1-D software.
Irradiation and clonogenic assay
Cells (~300) that had been treated with EGFR-siRNA3
or a non-targeting siRNA as the control were seeded into 60-mm
diameter culture dishes. Each group was irradiated at six different
doses: 0, 1, 2, 4, 6 and 8 Gy, using the 6MV-X Synergy linear
accelerator (Elekta, Stockholm, Sweden) with a 1-cm filter and a
source-skin distance of 100 cm, at a dose rate of 3 Gy/min. The
radiation field was 40×40 cm. Following 10 days of incubation, the
colonies were fixed with methanol and stained with Giemsa (Beijing
Dingguo Changsheng Biotechnology Co., Ltd., Beijing, China) for 30
min. Colonies consisting of ≥50 cells were scored as viable
colonies. The colony formation rate was estimated from the planting
efficiency (PE; number of clones/inoculated cells × 100%) and the
surviving fraction (SF; colony formation rate of irradiated
cells/colony formation rate of control cells × 100%). The data were
fit to the multi-target model, and a survival curve of each group
was established using Prism software, version 5.0 (GraphPad
Software Inc., La Jolla, CA, USA). The radiobiological parameters,
including D0, Dq, and SF2 (survival fraction at 2 Gy) were
calculated according to the survival curves, in which logN=Dq/D0.
The sensitization enhancement ratio was calculated as the SF2 of
the control group/SF2 of the EGFR-siRNA3-treated group. The results
are based on ≥3 independent experiments.
Statistical analysis
The data are expressed as the mean ± standard error
of the mean, and the one-way analysis of variance (ANOVA) was
performed using SPSS software version 17.0 (SPSS, Inc., Chicago,
IL, USA), in addition to the Least Significant Difference test. A
P-value of <0.05 was considered to indicate a statistically
significant difference.
Results
Eca109 cells are successfully
transfected with siRNA
The siRNA was successfully transfected into Eca109
cells using Lipofectamine 2000, in a transient manner. Based on the
expression of the red fluorescent Cy3 reporter (Fig. 1), it was demonstrated that EGFR-siRNA
at 50 nmol/l yielded the highest transfection efficiency (≤85%),
and was therefore adopted for all subsequent experiments.
EGFR-siRNA treatment reduces EGFR mRNA
expression
The EGFR mRNA relative expression levels were
26.74±3.40, 9.52±1.09 and 4.61±10.5% following transfection with
EGFR siRNA1, 2 and 3, respectively; EGFR mRNA expression was
significantly reduced, compared with the relative expression rate
of 42.44% in the control group (P<0.0001; Fig. 2). The inhibition efficiency of the
three EGFR-siRNAs on EGFR mRNA expression was 22, 70 and 85%,
respectively. As the EGFR mRNA levels were most significantly
reduced in the EGFR-siRNA3 group, the EGFR-siRNA3 was selected for
use in the subsequent proliferation and clonogenic assays.
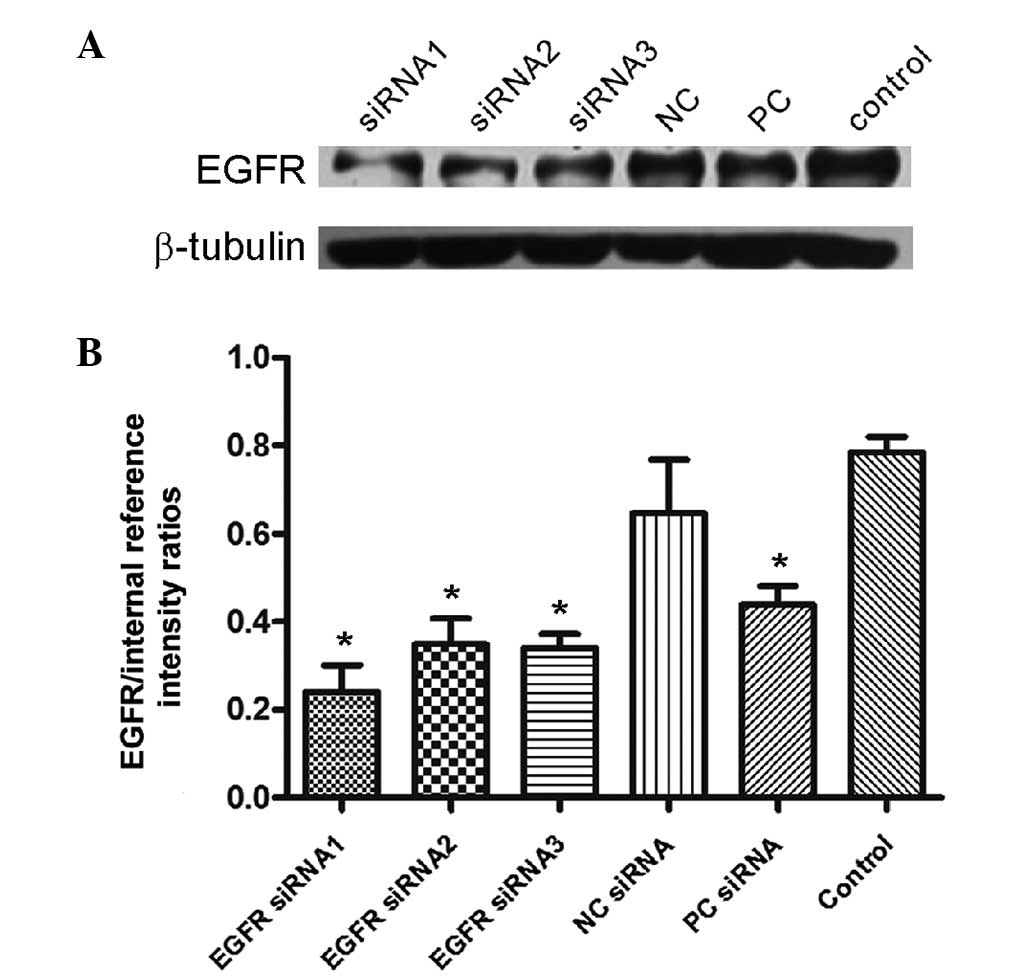
EGFR-siRNA treatment reduces EGFR
protein expression
The EGFR protein relative expression rate was
24.05±6.01, 34.91±5.78 and 34.14±3.08% (Fig. 3) following transfection with
EGFR-siRNA1, 2 and 3, respectively, compared with 78.57% in the
control group. This reduction in EGFR protein level was significant
(P<0.0001). The inhibition efficiencies of the three types of
EGFR-siRNA on EGFR protein expression were 72.84, 53.01 and 56.21%
(Fig. 3).
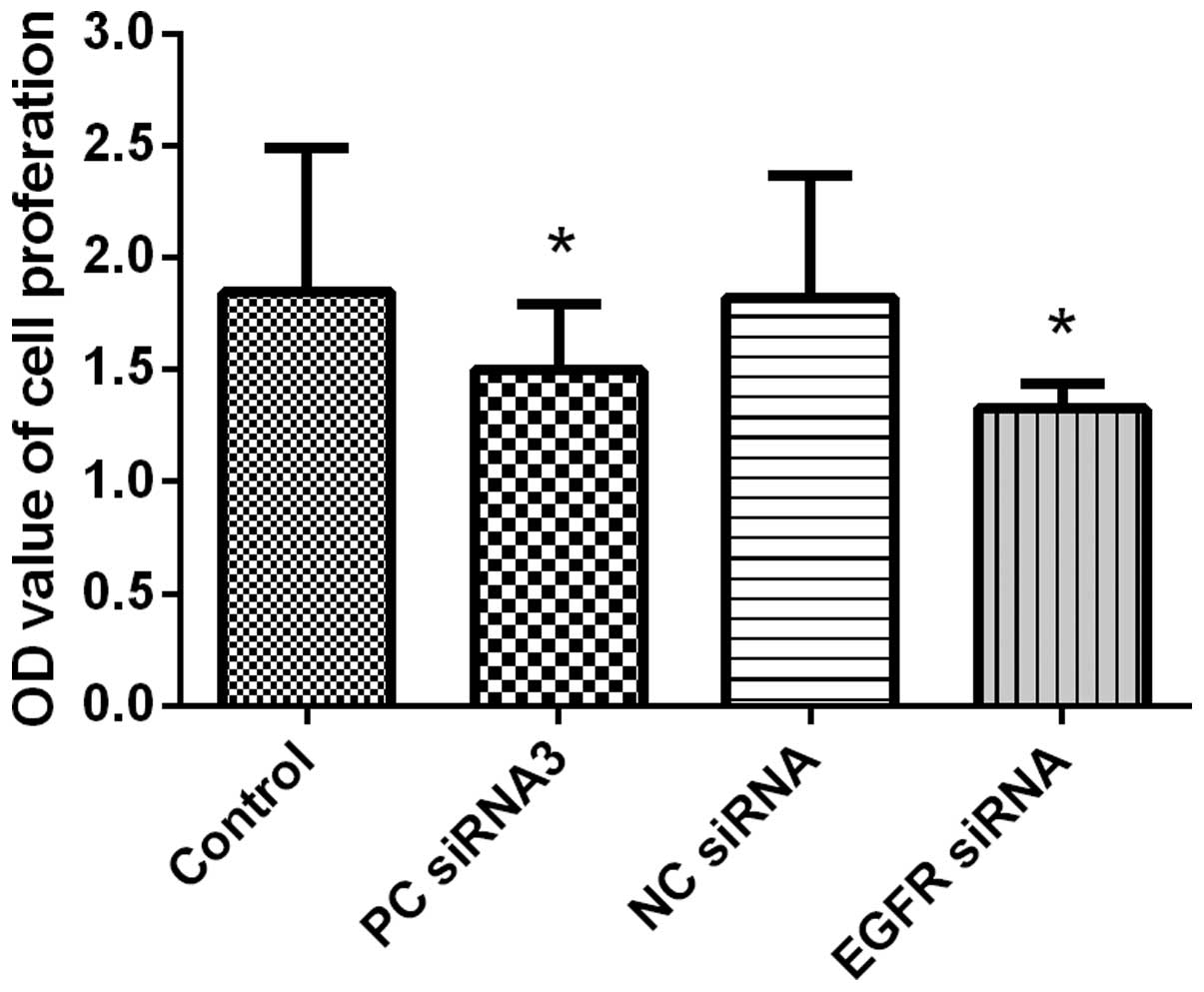
Downregulation of EGFR expression
inhibits the growth of Eca109 cells
EGFR-siRNA-treated cells demonstrated notable growth
retardation at 48 h following transfection, with an inhibition rate
of 28.2%, compared with the rate of growth in the blank control
group (Fig. 4; Table I). This inhibition rate was greater
than that observed at 24 h (data not shown), and therefore, this
time-period was selected as the detection time for mRNA and protein
expression of EGFR.
 | Table I.OD values for Eca109 cell
proliferation following transfection with EGFR-siRNA3 (n=3). |
Table I.
OD values for Eca109 cell
proliferation following transfection with EGFR-siRNA3 (n=3).
| Group | OD value |
|---|
| Blank control
group | 1.847±0.641 |
| Positive interference
siRNA control |
1.499±0.2974a |
| Negative interference
siRNA control | 1.820±0.548 |
| EGFR-siRNA |
1.326±0.110a |
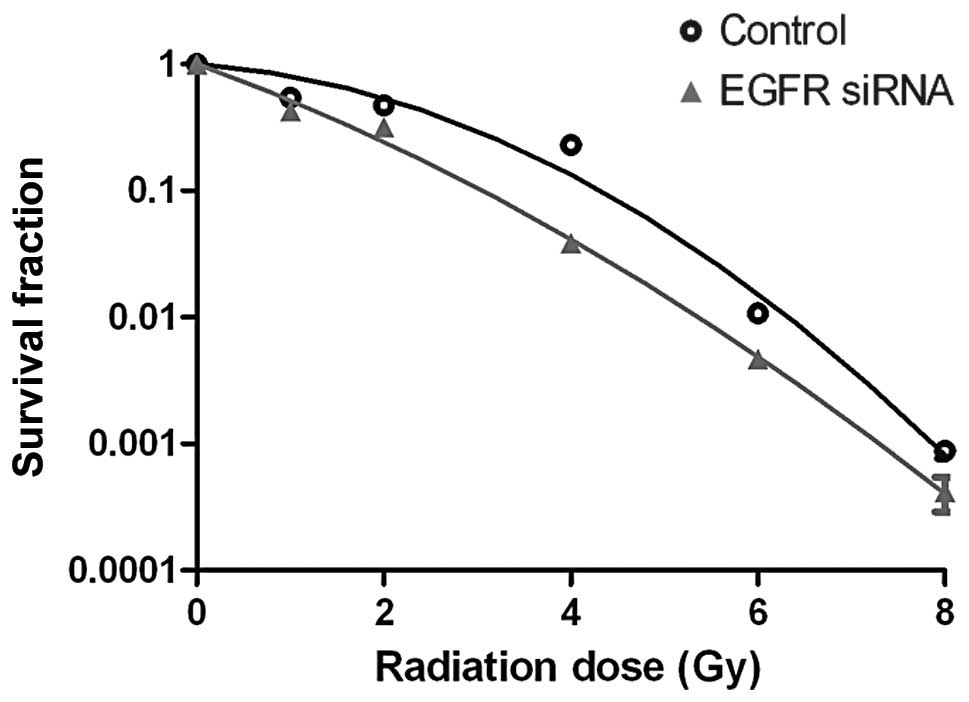
EGFR-siRNA increases the
radiosensitivity of Eca109 cells
The survival curve for the Eca109 cells in the
EGFR-siRNA group was significantly reduced following exposure to
various doses of X-ray radiation, compared with that of the control
group (Fig. 5). The radiobiological
parameters are presented in Table
II, with notable differences between the D0 and Dq values of
the two groups. These results indicated that transfection with
EGFR-siRNA reduced the ability of the Eca109 cells to repair
X-ray-induced damage, and therefore, increases the radiosensitivity
of the Eca109 cells.
 | Table II.Radiobiological parameters fitted
using the multi-target model. |
Table II.
Radiobiological parameters fitted
using the multi-target model.
| Group | D0 | Dq | SF2 | SER |
|---|
| Blank control | 2.86 | 0.88 | 0.48 |
|
| EGFR-siRNA | 1.84 | 0.65 | 0.32 | 1.5 |
Discussion
Binding of a ligand to the extracellular domain of
the EGFR results in dimerization of the EGFR molecules in the cell
membrane and induction of intracellular tyrosine kinase activity.
Autophosphorylation of specific tyrosine residues in the tyrosine
kinase domain results in a series of intracellular signal cascade
amplifications and transmissions, which ultimately regulate nuclear
gene expression resulting in cell proliferation and differentiation
(11). Previous studies have
demonstrated that EGFR is involved in the development and
progression of numerous types of tumor, thus making it an important
target for anticancer drug design (12). In the present study, the role of EGFR
was examined in the Eca109 ESCC cell line, in which EGFR is highly
expressed.
Overexpression or mutation of EGFR is one of the
main mechanisms underlying tumor cell resistance to radiotherapy,
which results in poor prognosis (13). Akimoto et al (5) demonstrated that the expression of EGFR
and radiosensitivity of solid tumors was negatively correlated, in
in vitro experiments. Tumors expressing high levels of EGFR
were more resistant to radiation compared with tumors expressing
low levels of EGFR (13). Therefore,
EGFR may represent an effective target for radiosensitization. The
EGFR inhibitor cetuximab (IMC-c225) and EGFR tyrosine kinase
inhibitors, including gefitinib and erlotinib, have previously been
comprehensively investigated (14),
and a proportion of these drugs have also been tested in phase I to
phase III clinical trials for the treatment of ESCC (14–18).
However, as these drugs are only effective in a small number of
patients, novel methods of inhibiting the EGFR pathway are
required.
RNAi is a mechanism of post-transcriptional gene
silencing, which has been observed in a number of eukaryotes.
siRNAs targeting specific genes in tumor cells may be used to
inhibit tumor cell growth, induce apoptosis and enhance sensitivity
to radiotherapy and chemotherapy; thus, they possess significant
potential as novel cancer drugs (19). Zhang et al (20) synthesized a combined double-stranded
RNA with a specific EGFR sequence by chemical methods in
vitro, transfected it into A549 cells with Lipofectamine 2000
and observed that EGFR expression was reduced by >70%, as
measured by western blot analysis and flow cytometry, while the
cell growth inhibition rate was >70%. Huo et al (21) transfected Eca109 cells with an
extracellular signal regulated kinase-specific siRNA to inhibit the
mitogen-activated protein kinase signaling pathway. This pathway
functions downstream of EGFR signaling. The authors demonstrated
that interference with this pathway inhibited tumor cell growth,
induced apoptosis, arrested cell cycle progression and enhanced the
radiosensitivity of EC cells. In the present study, EGFR expression
was successfully reduced in ESCC Eca109 cells by transfection with
EGFR-siRNA using Lipofectamine 2000. Following transfection with
EGFR-siRNA, the inhibition rate of EGFR mRNA was as high as 85% and
EGFR protein inhibition was as high as 72.84%, following EGFR
knockdown in Eca109 cells. In addition, the CCK-8 assay
demonstrated that Eca109 cell growth was inhibited as a result of
EGFR downregulation, with an inhibition rate of 28.2%. These
results indicated that the EGFR gene is important in the
proliferation and health of ESCC cells. A previous study indicated
that the use of RNAi technology can enhance the radiosensitivity of
tumor cells (22). In the present
study, a clonogenic assay was used to determine whether suppression
of EGFR affected the radiosensitivity of Eca109 cells. The observed
decline in the cell survival curve of EGFR-siRNA-treated cells
compared with that of the control cells indicated that
downregulation of EGFR increased cell radiosensitivity by up to
1.5-fold. As RNAi technology continues to improve, it may be
developed into a significant technique for the study of oncogene
function.
In conclusion, the results of the present study
indicated that RNAi technology successfully reduced EGFR mRNA and
protein levels in ESCC cells, which subsequently resulted in
inhibition of tumor cell proliferation in addition to an
improvement in the sensitivity of tumor cells to radiation. These
results provide a rationale for combining siRNA and radiotherapy in
the treatment of human epithelial cancers, which express EGFR.
Radiotherapy combined with siRNA may improve the therapeutic effect
and reduce the total radiation dose required in a clinical setting,
which is of potential clinical interest.
Acknowledgements
The present study was funded by the National Natural
Science Foundation of China (grant nos. 81402518 and 81472920), the
Jiangsu Provincial Special Program of Medical Science (no.
BL2012046) and the Changzhou Scientific Program (nos. ZD201315 and
CY20130017).
References
|
1
|
Parkin DM, Bray FI and Devesa SS: Cancer
burden in the year 2000. The global picture. Eur J Cancer. 37
(Suppl 8):S4–S66. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Stoner GD, Wang LS and Chen T:
Chemoprevention of esophageal squamous cell carcinoma. Toxicol Appl
Pharmacol. 224:337–349. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tatematsu N, Ezoe Y, Tanaka E, Muto M,
Sakai Y and Tsuboyama T: Impact of neoadjuvant chemotherapy on
physical fitness, physical activity and health-related quality of
life of patients with resectable esophageal cancer. Am J Clin
Oncol. 36:53–56. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ayyappan S, Prabhakar D and Sharma N:
Epidermal growth factor receptor (EGFR)-targeted therapies in
esophagogastric cancer. Anticancer Res. 33:4139–4155.
2013.PubMed/NCBI
|
|
5
|
Akimoto T, Hunter NR, Buchmiller L, Mason
K, Ang KK and Milas L: Inverse relationship between epidermal
growth factor receptor expression and radiocurability of murine
carcinomas. Clin Cancer Res. 5:2884–2890. 1999.PubMed/NCBI
|
|
6
|
Lammering G: Molecular predictor and
promising target: Will EGFR now become a star in radiotherapy?
Radiother Oncol. 74:89–91. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pai SI, Lin YY, Macaes B, Meneshian A,
Hung CF and Wu TC: Prospects of RNA interference therapy for
cancer. Gene Ther. 13:464–477. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Davis ME, Zuckerman JE, Choi CH, Seligson
D, Tolcher A, Alabi CA, Yen Y, Heidel JD and Ribas A: Evidence of
RNAi in humans from systemically administered siRNA via targeted
nanoparticles. Nature. 464:1067–1070. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dorsett Y and Tuschl T: siRNAs:
Applications in functional genomics and potential as therapeutics.
Nat Rev Drug Discov. 3:318–329. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nozawa H, Tadakuma T, Ono T, Sato M, Hiroi
S, Masumoto K and Sato Y: Small interfering RNA targeting epidermal
growth factor receptor enhances chemosensitivity to cisplatin,
5-fluorouracil and docetaxel in head and neck squamous cell
carcinoma. Cancer Sci. 97:1115–1124. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rodemann HP, Dittmann K and Toulany M:
Radiation-induced EGFR-signaling and control of DNA-damage repair.
Int J Radiat Biol. 83:781–791. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pal SK and Pegram M: Epidermal growth
factor receptor and signal transduction: Potential targets for
anti-cancer therapy. Anticancer Drugs. 16:483–494. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Krause M, Prager J, Zhou X, Yaromina A,
Dörfler A, Eicheler W and Baumann M: EGFR-TK inhibition before
radiotherapy reduces tumour volume but does not improve local
control: Differential response of cancer stem cells and
nontumourigenic cells? Radiother Oncol. 83:316–325. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sunpaweravong P, Sunpaweravong S,
Sangthawan D, et al: Combination of gefitinib, cisplatin and 5-FU
chemotherapy and radiation therapy (RT) in newly-diagnosed patients
with esophageal carcinoma. J Clin Oncol. 25:46052007.
|
|
15
|
Safran H, Suntharalingam M, Dipetrillo T,
et al: Cetuximab with concurrent chemoradiation for esophagogastric
cancer: Assessment of toxicity. Int J Radiat Oncol Biol Phys.
70:391–395. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ruhstaller T, Pless M, Dietrich D, et al:
Cetuximab in combination with chemoradiotherapy before surgery in
patients with resectable, locally advanced esophageal carcinoma: A
prospective, multicenter phase lB/II Trial (SAKK 75/06). J Clin
Oncol. 29:626–631. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Suntharalingam M, Dipetrillo T, Akerman P,
et al: Cetuximab, paclitaxel, carboplatin, and radiation for
esophageal and gastric cancer. J Clin Oncol. 24:40292006.PubMed/NCBI
|
|
18
|
Tomblyn MB, Goldman BH, Thomas CR Jr, et
al SWOG GI Committee: Cetuximab plus cisplatin, irinotecan, and
thoracic radiotherapy as definitive treatment for locally advanced,
unresectable esophageal cancer: A phase-II study of the SWOG
(S0414). J Thorac Oncol. 7:906–912. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Izquierdo M: Short interfering RNAs as a
tool for cancer gene therapy. Cancer Gene Ther. 12:217–227. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhang M, Zhang X, Bai CX, Chen J and Wei
MQ: Inhibition of epidermal growth factor receptor expression by
RNA interference in A549 cells. Acta Pharmacol Sin. 25:61–67.
2004.PubMed/NCBI
|
|
21
|
Huo Q, Zheng ST, Tuersun A, et al: shRNA
interference for extracellular signal-regulated kinase 2 can
inhibit the growth of esophageal cancer cell line Eca109. J Recept
Signal Transduct Res. 30:170–177. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vandersickel V, Maneini M, Marras E, et
al: Lentivirus-mediated RNA interference of Ku70 to enhance
radiosensitivity of human mammary epithelial cells. Int J Rediat
Biol. 86:114–124. 2010. View Article : Google Scholar
|