Introduction
Renal angiomyolipoma (AML) is a benign tumor
containing elements of fat cells, smooth muscle and vascular
tissue. There are two variants of this tumor; one is associated
with tuberous sclerosis complex (TSC) and the other is sporadic.
TSC is a multisystem, autosomal disease with various presentations,
such as mental retardation, epilepsy, dermatological manifestation,
renal AML and pulmonary lymphangiomyomatosis (1,2).
Approximately 20% of renal AML cases are associated with TSC, in
which 70–90% are bilateral (3,4).
Early studies summarized the clinical management of
renal AML and established that renal-preserving treatments,
including selective angiographic embolization (SAE) and
nephron-sparing surgery (NSS), are preferred (5,6). SAE is
considered to be an effective and durable treatment for preventing
bleeding in large renal AML, particularly for patients with an
aneurysm. Recent studies demonstrated that 91–93% of renal AML
cases are successfully embolized, however, the cost of surveillance
and the morbidity of re-embolization were not negligible (7,8). Although,
NSS has been widely performed in the past two decades with good
results, the majority of results are for sporadic renal AML cases,
and the tumors are typically are unilateral and small (9,10).
In the current report, a case of giant bilateral
renal AML without TSC is presented. The patient underwent a total
nephrectomy for a right AML measuring 28×20×14 cm and NSS was
performed for 3 AMLs in the left kidney, the largest of which had a
diameter of 12 cm. The patient provided written informed consent to
participate in the study and the study was approved by the Ethics
Review Committee of the Third Xiangya Hosiptal of Central South
University (Changsha, China).
Case report
In April 2013, a 50-year-old female presented to the
Department of Urology at the Third Xiangya Hospital of Central
South University with a flank mass and abdominal fullness, which
were confirmed by palpation. The patient did not present with any
additional symptoms that met the diagnostic criteria for TSC. The
serum creatinine level was 0.93 mg/dl (normal range, 0.51–1.19
mg/dl), and the hemoglobin level was 131 g/l (normal range, 115–150
g/l). The results of coagulation function and biochemistry were
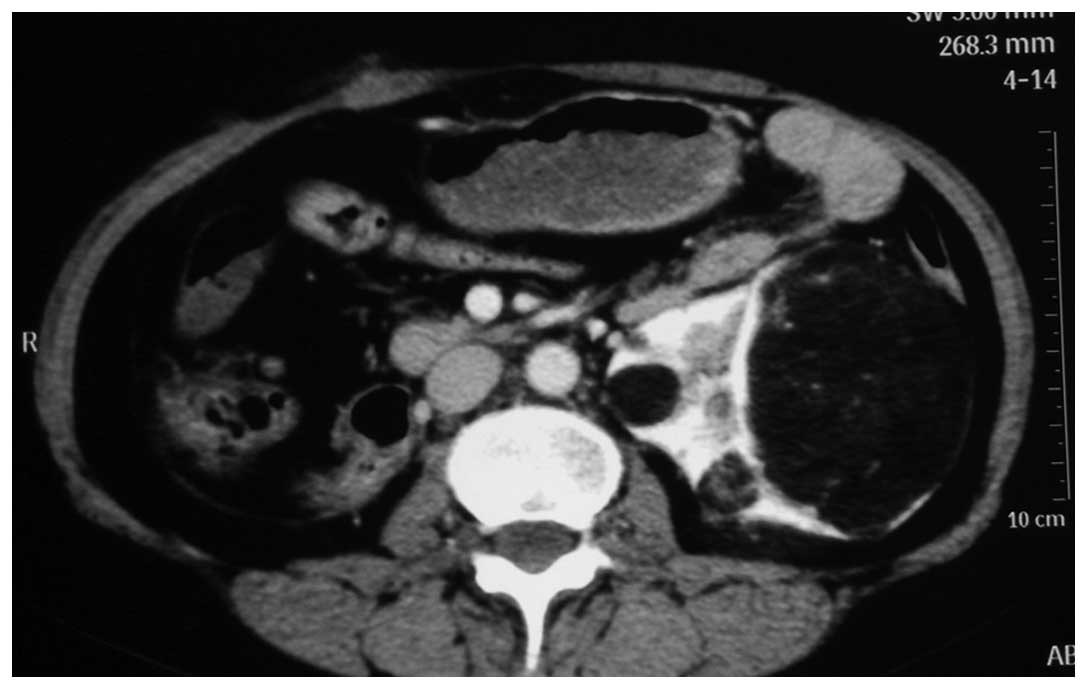
within the normal limits. Abdominal computed tomography (CT)
revealed a large AML measuring 28×20×14 cm (Fig. 1) arising from the right kidney and
deviating the rest of the abdominal contents across the midline,
and a 12×9×6 cm AML arising from the upper pole of the left kidney.
Several small AMLs were also observed in the left kidney (Fig. 2). The glomerular filtration rate (GFR)
was evaluated using a technetium 99 m-diethylenetriminepentaacetic
acid (DTPA) nuclear renal scan, revealing that the right renal
function was severely impaired, with a right kidney GFR of 12.57
ml/min. A right total nephrectomy was performed, and the
postoperative serum creatinine and hemoglobin was 0.97 mg/dl, 120
g/l, respectively. Histopathological analysis revealed that the
renal mass was composed of fat, vascular structures and smooth
muscle, indicating a diagnosis of AML. Upon immunohistochemical
analysis, the tumor cells stained positive for smooth muscle actin,
human melanoma black 45 and vimentin, and negative for cluster of
differentiation 34, desmin and S-100. Furthermore, the Ki-67
proliferation rate was <3%. Based on the histopathological and
immunohistochemical findings, a diagnosis of a renal AML was
determined.
NSS for the AML present in the left kidney was
performed 3 months after the right total nephrectomy. A CT scan was
conducted prior to NSS to evaluate the tumor size in the left
kidney and for the follow-up investigation, and demonstrated
several AMLs (Fig. 3). NSS was
performed using a flank incision in the eleventh intercostal space.
Following careful dissection, renal vessel occlusion was
identified. A total of 3 AMLs were resected: The largest tumor
(diameter, 12 cm)was resected and the other two tumors were
enucleated. The total ischemia time was 24 min. Histopathological
analysis revealed that the 3 masses were composed of fat, vascular
structures and smooth muscle, consistent with a diagnosis of AML.
Upon immunohistochemical analysis, the tumor cells stained positive
for smooth muscle actin and vimentin, and negative for human
melanoma black 45, desmin and S-100. In addition, the Ki-67
proliferation rate was ~5%. The preoperative and postoperative
serum creatinine and hemoglobin levels were 0.93 mg/dl and 129 g/l,
and 1.27 mg/dl and 102 g/l, respectively. The estimated
intraoperative bleeding volume was 500 ml and 2 units of blood
transfusion was performed.
Regular routine blood tests, biochemistry,
ultrasonographic and/or CT scan were evaluated for follow-up
investigation. No local recurrence was observed and no dialysis was
required.
Discussion
The incidence of renal AMLs is rare and a proportion
of AMLs are asymptomatic. Indications for intervention include
dimensions >4 cm, associated symptoms, including spontaneous
hemorrhage, pain and hematuria and the suspicion of malignancy
(11). Asymptomatic AML and lesions
that result in minor symptoms may be managed conservatively.
However, the 4 cm threshold is not a definite criteria. Cavicchioli
et al (12) reported a
50-year-old man with bilateral renal AML that was 27.5×19.5×21 cm
on the left kidney and 28.5×19.6×27.5 cm on the right. The patient
was asymptomatic and underwent a strict surveillance with magnetic
resonance imaging every 4–5 months. At the last follow-up, the
patient was asymptomatic and serum creatinine was normal.
AML has been reported to have the potential to
increase in size by up to 4 cm per year (13,14). Given
this nature, the majority of giant renal AML are symptomatic and
treatments for renal AML are aimed at preserving renal function.
SAE and NSS are indicated as effective renal function-preserving
approaches. Ramon et al (7)
analyzed the outcomes of 41 patients who received SAE for renal AML
with a mean follow-up period of 4.8 years. SAE was performed
through an artery using angiographic catheters. Digital subtraction
angiographic examinations were used for diagnosis, followed by an
aortogram for evaluation of renal arterial feeders to the tumor.
Then, embolization was performed with different materials, such as
absolute alcohol and metal coils. Successful SAE was achieved in
40/41 patients (91%) and avoidance of surgery was achieved for
79/82 (96%) of the kidneys. No retroperitoneal hemorrhage was noted
and 80/82 (98%) of the kidneys were preserved during follow-up.
Boorjian et al (15) analyzed
the outcomes of 58 patients who recieved NSS for renal AML, with a
median follow-up of 8-years. The analysis demonstrated that NSS for
renal AML results in preservation of renal function with acceptable
rates of complication and low local recurrence rates.
For large renal AML, preoperative SAE is recommended
to reduce excessive blood loss during surgery. Singla et al
(16) reported a case of giant renal
AML measuring 26×22 cm that was treated with preoperative
embolization followed by partial nephrectomy without complications.
Similarly, Luo et al (17)
presented a 44-year-old man with bilateral giant AMLs with a
diameter of 38.2 cm in the left kidney and 9.5 cm in the right
kidney. The patient was treated successfully with preoperative SAE
and NSS without hilar clamping. However, postembolization syndrome,
the reduction of tumor volume and the optimal time window for NSS
following SAE should be taken into consideration. Postembolization
syndrome is a side effect of embolization procedures and consists
of one or more of the following symptoms: Flank pain, fever, nausea
and vomiting attributable to inflammatory mediators (18,19).
In the current report, the patient's symptoms, the
tumor size and the damaged renal function were the main reasons for
the decision to undertake a right total nephrectomy. As the patient
had a solitary kidney when she was hospitalized for the second
time, preoperative SAE was not performed in order to reduce the
additional burden on the remaining renal function. Without
preoperative SAE, the intraoperative bleeding volume was acceptable
and the renal function was stable.
In conclusion, the management of giant bilateral
renal AML is challenging and complex. A strict assessment,
including the patient's symptoms, the tumor size and renal
function, should be taken in choosing an effective and safe
treatment approach. The present case demonstrates that NSS without
preoperative SAE was effectively used to treat a solitary kidney.
The strategy of treatment undertaken in this report may be
considered when treating similar tumors.
Acknowledgements
The present study was supported by the Fundamental
Research Funds for the Central Universities of Central South
University (grant no. 2014zzts370).
References
|
1
|
Crino PB, Nathanson KL and Henske EP: The
tuberous sclerosis complex. N Engl J Med. 355:1345–1356. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Curatolo P, Bombardieri R and Jozwiak S:
Tuberous sclerosis. Lancet. 372:657–68. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
O'Callaghan FJ, Noakes MJ, Martyn CN and
Osborne JP: An epidemiological study of renal pathology in tuberous
sclerosis complex. BJU Int. 94:853–857. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rakowski SK, Winterkorn EB, Paul E, Steele
DJ, Halpern EF and Thiele EA: Renal manifestations of tuberous
sclerosis complex: Incidence, prognosis and predictive factors.
Kidney Int. 70:1777–1782. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nelson CP and Sanda MG: Contemporary
diagnosis and management of renal angiomyolipoma. J Urol.
168:13152002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sivalingam S and Nakada SY: Contemporary
Minimally Invasive Treatment Options for Renal Angiomyolipomas.
Curr Urol Rep. 14:147–153. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ramon J, Rimon U, Garniek A, Golan G,
Bensaid P, Kitrey ND, Nadu A and Dotan ZA: Renal angiomyolipoma:
Long-term results following selective arterial embolization. Eur
Urol. 55:1155–1162. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chan CK, Yu S, Yip S and Lee P: The
efficacy, safety and durability of selective renal arterial
embolization in treating symptomatic and asymptomatic renal
angiomyolipoma. Urology. 77:642–648. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Heidenreich A, Hegele A, Varga Z, von
Knobloch R and Hofmann R: Nephron-sparing surgery for renal
angiomyolipoma. Eur Urol. 41:267–273. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
FazeliMatin S and Novick AC:
Nephron-sparing surgery for renal angiomyolipoma. Urology.
52:577–583. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nelson CP and Sanda MG: Contemporary
diagnosis and management of renal angiomyolipoma. J Urol.
168:1315–1325. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cavicchioli FM, D'Elia C, Cerruto MA and
Artibani W: Giant bilateral renal angiomyolipomas: A case report.
Urol Int. 92:366–368. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Seyam RM, Bissada NK, Kattan SA, Mokhtar
AA, Aslam M, Fahmy WE, Mourad WA, Binmahfouz AA, Alzahrani HM and
Hanash KA: Changing trends in presentation, diagnosis and
management of renal angiomyolipoma: Comparison of sporadic and
tuberous sclerosis complex-associated forms. Urology. 72:1077–1082.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ewalt DH, Sheffield E, Sparagana SP,
Delgado MR and Roach ES: Renal lesion growth in children with
tuberous sclerosis complex. J Urol. 160:141–145. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Boorjian SA, Frank I, Inman B, Lohse CM,
Cheville JC, Leibovich BC and Blute ML: The role of partial
nephrectomy for the management of sporadic renal angiomyolipoma.
Urology. 70:1064–1068. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Singla A, Chaitanya Arudra SK and Bharti
N: Giant sporadic renal angiomyolipoma treated with nephron-sparing
surgery. Urology. 74:294–295. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Luo Y, Hou GL, Lu MH, Chen MK, Hu C and Di
JM: Unclamped nephron-sparing surgery with preoperative selective
arterial embolization for the management of bilateral giant renal
angiomyolipomas. Clin Genitourin Cancer. 12:e111–e114. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Halpenny D, Snow A, McNeill G and
Torreggiani WC: The radiological diagnosis and treatment of renal
angiomyolipoma - current status. Clin Radiol. 65:99–108. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bissler JJ, Racadio J, Donnelly LF and
Johnson ND: Reduction of postembolization syndrome after ablation
of renal angiomyolipoma. Am J Kidney Dis. 39:966–971. 2002.
View Article : Google Scholar : PubMed/NCBI
|