Introduction
Clear cell carcinoma, which is common amongst males
aged 50–60 years, accounts for 80–85% of adult renal malignant
tumors. The 5-year survival rate following surgery is 50%, and
reduces to <5% in patients with distant metastases. Renal cell
carcinoma (RCC) is associated with a high metastatic potential, and
the most frequent sites of RCC metastasis include the lungs, bone,
liver and skin (1). RCC metastases to
the head and neck region are less common, comprising 8–14% of
metastatic cases. Within the head and neck region, the thyroid
gland is the most common site of RCC metastasis, while parotid
gland metastasis is particularly rare. To the best of our
knowledge, no similar case has previously been reported in
English-language literature. The present study comprises a case
report to investigate the clinical features and treatment
experience of a patient with renal clear cell carcinoma with
thyroid and parotid metastases. Written informed consent was
provided by the patient.
Case report
A 56-year-old female, with a right preauricular
painless mass present for six months, was referred to the
Department of Otorhinolaryngology Head and Neck Surgery (now two
separate departments), Renji Hospital, Shanghai Jiaotong University
School of Medicine (Shanghai, China). Physical examination revealed
a mass of 3×3 cm, which was smooth, firm, immobile and non-tender.
There was no facial weakness, and no enlarged cervical lymph nodes
or submandibular lymph nodes were detected. Laboratory tests
revealed that blood, liver and kidney function were normal. Parotid
ultrasonography identified a hypoechoic mass within the right
parotid gland, and a potential diagnosis of parotid mixed tumor was
suggested. In July 2011, the patient underwent an superficial
parotidectomy with preservation of the facial nerve. A 2-cm
diameter, easy bleeding, encapsulated tumor with a clear border was
identified in the right superficial lobe of the parotid gland. The
border of the tumor remained clear, without adhesion of the facial
nerve. Pathology confirmed the tumor to be right parotid clear cell
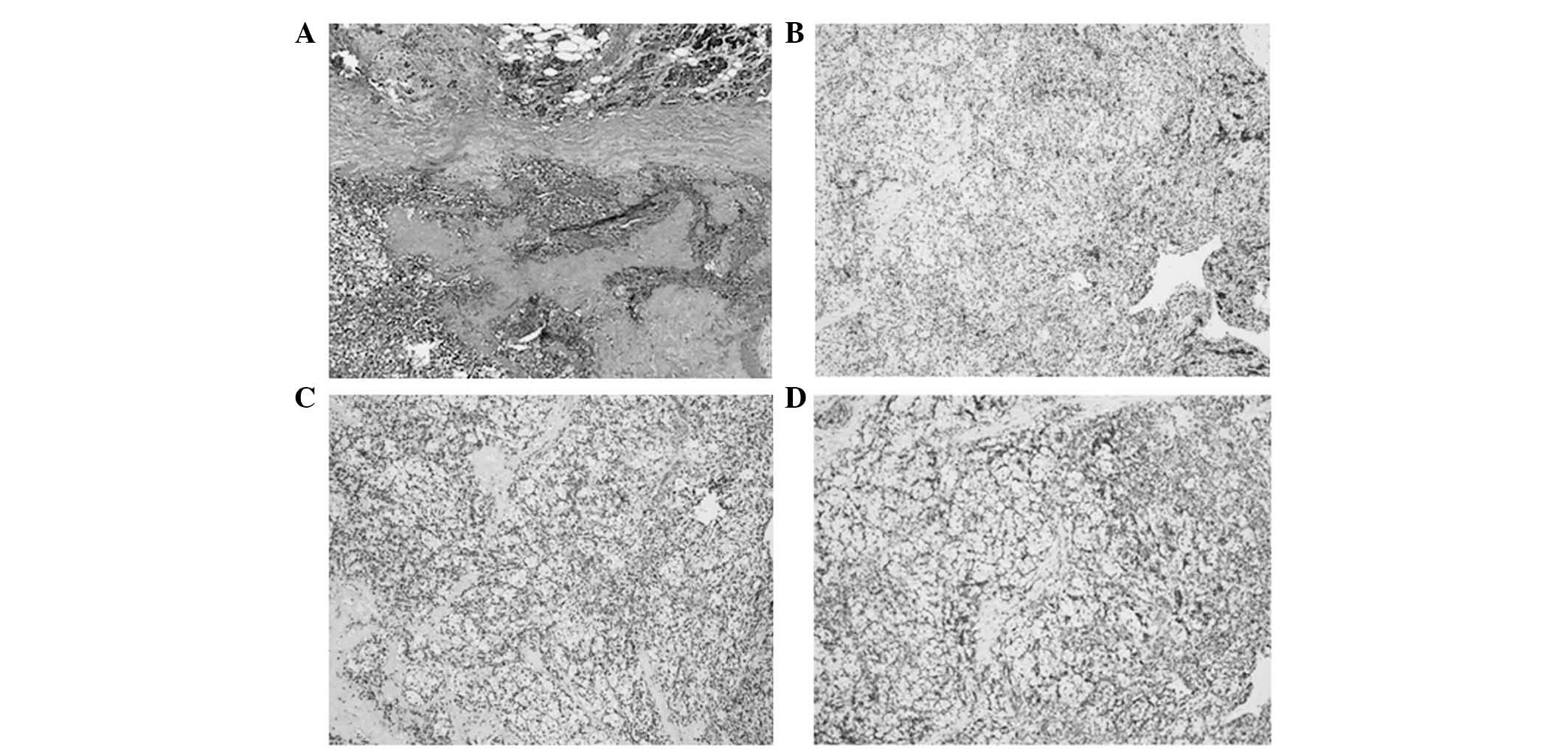
carcinoma (metastasis). Immunohistochemical analysis revealed
positive reactions for cytokeratin (CK), vimentin, CK8 and Rcc,
whereas stains for CD10, von Hippel-Lindau tumor suppressor, E3
ubiquitin protein ligase, Ki-67 and actin were negative (Fig. 1).
The patient's relevant medical history included a
radical right nephrectomy for renal clear cell carcinoma (clinical
stage III) in 2004. Immunohistochemical examination of the renal
tumor indicated: CK8 (+), vimentin (+), CD10 (+), CK19 (−), CK7 (−)
and α-methylacyl-CoA racemase (AmACR) (−). The patient received
chemotherapy (5-Fluorourcil + α-interferon + interleukin-2)
following surgery. In addition, the patient underwent a resection
of thyroid metastatic renal cell carcinoma in 2009.
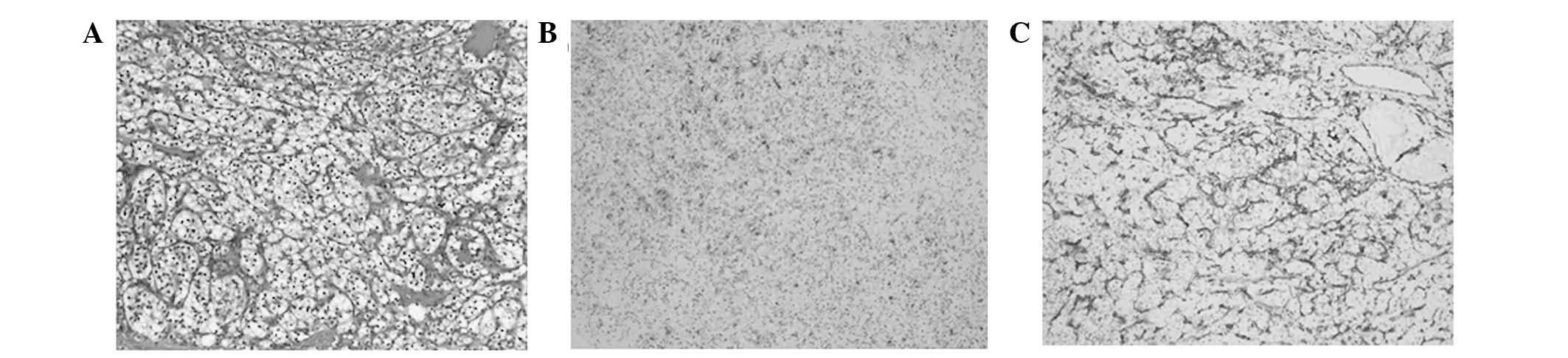
Immunohistochemical examination following surgery indicated the
following: Rcc (+), AmACR (−), vimentin (+++), CK (−), TPO (−),
CK19 (−), galectim-3 (+++) and CD10 (++) (Fig. 2). The patient did not receive
postoperative radiotherapy and/or chemotherapy. The patient was
followed-up for 2 years following surgery, with no tumor metastasis
detected.
Discussion
RCC accounts for ~3% of all malignant tumors
(2). Metastasis is common in patients
with RCC; common sites of RCC metastasis include the lungs, lymph
nodes, bone and liver. However, metastases to the head and neck
region are less common. The thyroid gland is the most common site
of RCC metastasis within the head and neck region, however,
metastasis to the parotid gland is rare. The present study reported
the case of a RCC patient with thyroid and parotid metastases,
which to the best of our knowledge, is the first case to be
reported in the literature. Physical examination 56-year-old female
patient revealed a 3-cm diameter, smooth, high-tension immobile
mass in the right preauricular region. There was no facial
paralysis and no enlarged cervical lymph nodes were detected.
Parotid ultrasonography identified a hypoechoic mass within the
right parotid gland and a potential diagnosis of parotid mixed
tumor was suggested. All other tests were normal. In July 2011, the
patient underwent a superficial parotidectomy with preservation of
the facial nerve. During surgery, a 2-cm diameter, crispy, easy
bleeding, encapsulated tumor was identified in the right
superficial lobe of the parotid gland. To the best of our
knowledge, no similar case has previously been reported.
The thyroid gland has a rich blood supply (3). According to autopsy studies, the
incidence of metastasis to the thyroid is 1.9–24.2% amongst
patients who succumb to malignant tumors of other primary sites
(4,5).
Breast and lung cancer, as well as malignant melanomas, are the
most frequently identified malignant neoplasms, which generate
secondary cancer of the thyroid (6,7). Although
RCCs were previously considered to be another cancer which may
metastasize to the thyroid, this is a rare occurrence in clinical
practice. The present study identified few reports of renal clear
cell carcinoma with thyroid metastases published in the
English-language literature. Thyroid metastasis of renal clear cell
carcinoma must be distinguished from primary thyroid clear cell
carcinoma. Certain scholars have suggested that primary thyroid
carcinoma is a variation of thyroid follicular carcinoma, and the
clear cells in the carcinoma are the result of stimulation by
thyroid-stimulating hormone (8). In
addition to possessing a similar cellular morphology, the tumor
cells, sheets and cords are separated by fibrous tissue. Sections
of tumor tissue exhibit a small follicular structure and glial
nodules. The most appropriate method for the diagnosis of thyroid
metastatic carcinoma is preoperative fine needle aspiration
cytology (9). In addition, the
primary site may be identified using specific immunohistochemical
staining with antibodies against CD10, CK and vimentin, to confirm
metastatic RCC through pathological detection, particularly in the
lung and thyroid (10). Currently,
total thyroidectomy for treatment with combined therapy is
recommended for patients with renal carcinoma metastasis of the
thyroid, particularly those which grow slowly and exhibit no other
evidence of distant metastasis (11).
Salivary gland metastasis of renal clear cell
carcinoma is particularly rare. Malignant parotid gland tumors
account for ~29% of parotid masses. Metastases to the parotid gland
are uncommon, and most frequently originate from head and neck
squamous cell carcinomas or melanomas of the skin (12). Parotid metastasis from RCC is very
rare, accounting for only 0.5% of renal metastases (13). According to the literature, parotid
metastasis may occur prior to or following primary treatment for
RCC (14). The major symptom is often
a painless parotid mass, as observed in the present case.
Currently, ultrasonic examination has become the first choice in
the diagnosis of parotid tumors as it is cheap, non-invasive and
harmless (15). Yu reported that the
correct rate of ultrasound diagnosis of parotid tumor was 78.6%
(16). The ultrasonic characteristics
of the present case were similar to those of a benign tumor, which
indicated the risk of potential misdiagnosis. The present author
suggested that ultrasound-guided fine needle aspiration cytology
and the patient's medical history should be taken into
consideration, particularly when it is difficult to distinguish
between benign and malignant tumors. It is also crucial to
distinguish between parotid metastases and primary cancer.
Pathological examination, immunohistochemistry with antibodies
against CD10, CK and vimentin, as well as systemic examination
revealed that the primary kidney tumor was identifiable. For
parotid metastasis from renal cell carcinoma without other
metastases, the recommended therapy is superficial parotidectomy
with the preservation of the facial nerve (12). When the parotid gland has invaded the
surrounding tissue, the scope of the parallel operation requires
expansion to include elective lymph node dissection (II–V
area).
Thyroid metastasis were identified in the present
patient 4 years following radical nephrectomy and parotid gland
metastasis were subsequently identified 6 years following surgery.
It was therefore suggested that RCC patients require long-term
follow-up, to facilitate early detection of metastasis and early
comprehensive treatment.
References
|
1
|
Dekernion JB, Ramming KP and Smith RB: The
natural history of metastatic renal cell carcinoma: A computer
analysis. J Urol. 120:148–152. 1978.PubMed/NCBI
|
|
2
|
Ohba K, Miyata Y, Mitsunari K, et al: Left
atrial metastasis of renal cell carcinoma: A case report and review
of the literature. BMC Res Notes. 7:5202014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen H, Nicol TL and Udelsman R:
Clinically significant, isolated metastatic disease to the thyroid
gland. World J Surg. 23:177–180. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Abrams HL, Spiro R and Goldstein N:
Metastases in carcinoma: Analysis of 1000 autopsied cases. Cancer.
3:74–85. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shimaoka K, Sokal JE and Pickren JW:
Metastatic neoplasms in the thyroid gland. Pathological and
clinical findings. Cancer. 15:557–565. 1962. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chung AY, Tran TB, Brumund KT, Weisman RA
and Bouvet M: Metastases to the thyroid: A review of the literature
from the last decade. Thyroid. 22:258–268. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lam KY and Lo CY: Metastatic tumors of the
thyroid gland: A study of 79 cases in Chinese patients. Arch Pathol
Lab Med. 122:37–41. 1998.PubMed/NCBI
|
|
8
|
Vatiakojis D, Getz ML, Paloyan E and
Straus FH: Papillary clear cell carcinoma of the thyroid gland. Hun
Pathol. 6:384–390. 1975. View Article : Google Scholar
|
|
9
|
Morgan JL, Serpell JW and Cheng MS:
Fine-needle aspiration cytology of thyroid nodules: How useful is
it? Anz J Surg. 73:480–483. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mrena R, Leivo I, PassadorSantos F,
Hagström J and Mäkitie AA: Histopathological findings in parotid
gland metastases from renal cell carcinoma. Eur Arch
Otorhinolaryngol. 265:1005–1009. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kihara M, Yokomise H and Yamauchi A:
Metastasis of renal cell carcinoma to the thyroid gland 19 years
after nephrectomy: A case report. Auris Nasus Larynx. 31:95–100.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Park YW and Hlivko TJ: Parotid gland
metastasis from renal cell carcinoma. Laryngoscope. 112:453–356.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pisani P, Angeli G, Krangli M and Pia F:
Renal carcinoma metastasis to the parotid gland. J Laryngol Otol.
104:352–354. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Göğüş C, Kiliç O, Tulunay O, Tulunay O and
Bedük Y: Solitary metastasis of renal cell carcinoma to the parotid
gland 10 years after radical nephrectomy. Int J Urol. 11:894–896.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen XY, Long X, Qian SS, et al: The
clinical significance of the use of ultrasonography in the
diagnosis of parotid tumors. J Clin Stomatol. 18:448–449. 2002.(In
Chinese).
|
|
16
|
Yu GY: Salivary Gland Diseases. Beijing
Medical University Press; Beijing: 1994
|