Introduction
Multiple myeloma (MM), or myelomatosis, is a rare
type of hematological malignancy that comprises ~10% of all
hematological malignancies. It is a neoplastic proliferation
characterized by the uncontrolled proliferation of plasma cells in
the bone marrow that leads to bone osteolytic destruction, anemia,
recurrent infections and renal impairment. The incidence of MM is
~3–4 per 100,000 individuals (1).
Common presenting features of MM include bone pain and bone
fractures, anemia, increased susceptibility to infections,
hypercalcemia, neurological manifestations, hyperviscosity syndrome
and renal failure (1,2).
Although MM is usually confined to the bone marrow,
it may occasionally infiltrate into other tissues (3,4), and this
is known as extramedullary plasmacytoma (EMP). To the best of our
knowledge, there are no recommended guidelines for the treatment of
EMP. Treatment options include surgery, chemotherapy and
radiotherapy, either alone or combination (5). Local radiotherapy is the preferred
therapeutic modality for EMP owing to its documented
radiosensitivity (6). However,
previous studies indicated that a combination treatment may provide
the best results (7). The majority of
EMPs involve the head and neck regions (8), although different anatomical sites,
including the gastrointestinal tract, central nervous system,
thyroid gland and breast may also be affected (7). However, it is rare that EMPs present
initially with simultaneous intracranial and renal
infiltration.
The current study reports a case of primary
intracranial and renal plasmacytoma in a 76-year-old male patient.
Written informed consent was obtained from the patient's family and
ethical approval was obtained from the committee of Cangzhou
Central Hosptial (Cangzhou, China).
Case report
The patient presented to the Cangzhou Central
Hospital in March 2014, complaining of swelling over the right side
of the forehead, which had been slowly progressing during the 3
months prior to the date of admission, and was associated with
dizziness and weakness. The patient did not present bone pain or a
tendency for abnormal bleeding, and physical examination excluded
lymphadenopathy and organomegally. A tense globular swelling of
5.0–6.5 cm in size was observed over the right frontal area,
adhered to the underlying skull and skin. Contrast magnetic
resonance imaging (MRI) suggested an osteolytic skull lesion with
intracranial extension (Fig. 1A).
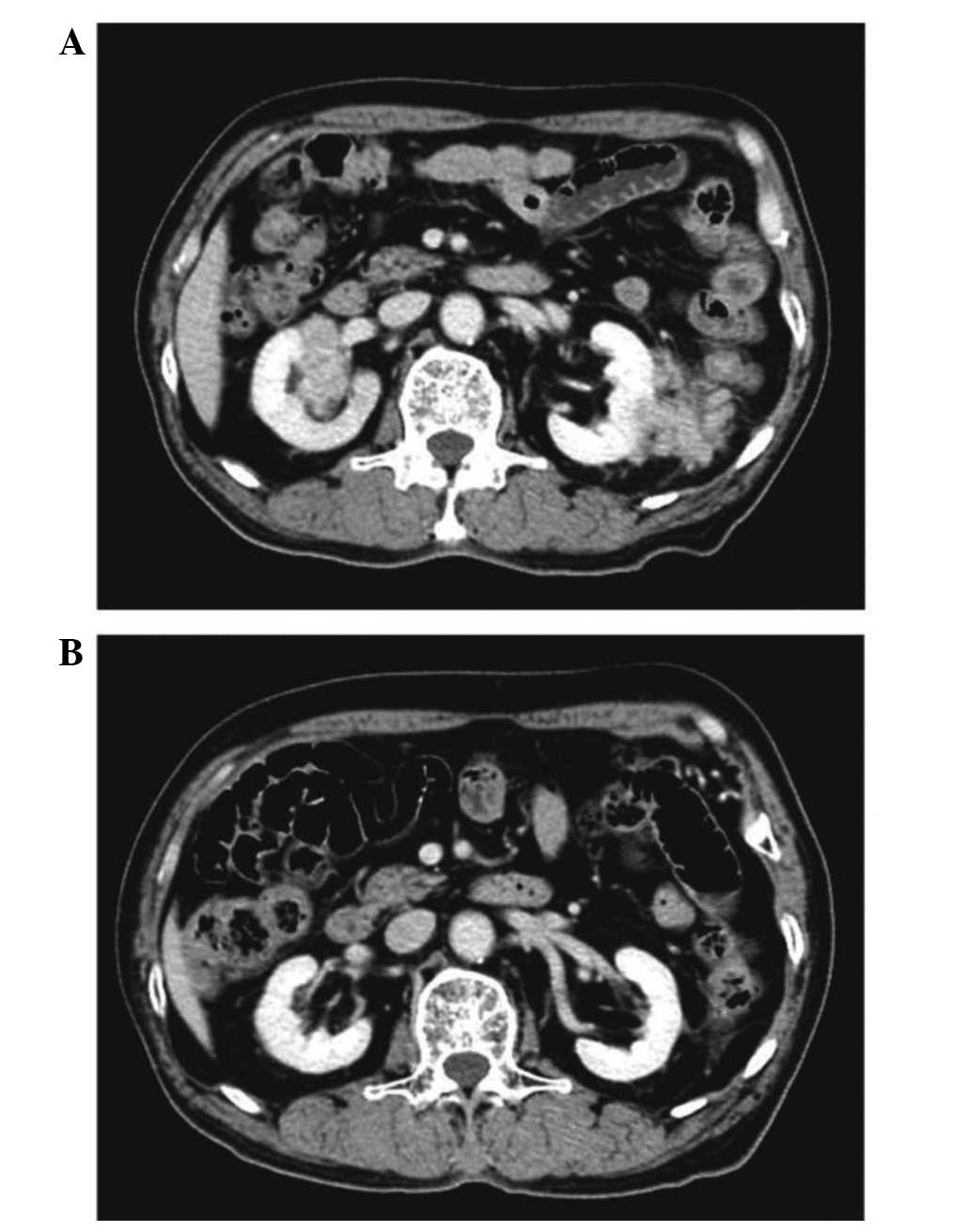
Abdominal enhanced computed tomography (CT) scanning revealed a
large tumor mass extending around and into the kidneys (Fig. 2A). Thus, a right renal biopsy was
performed, and histopathological analysis of the tumor sample
confirmed it to be plasmacytoma. Immunohistochemical staining was
performed using cluster of differentiation (CD)38 and CD138
antibodies purchased from Beijing Xiya Jinqiao Biological
Technology Co., Ltd. (Beijing, China). All stains were completed
using a BenchMark machine (serial no. 815132; Ventana Medical
Systems, Inc., Tucson, AZ, USA) and images were captured with an
Olympus BX41 microscope (Olympus, Tokyo, Japan) and Image-Pro Plus
software (Media Cybernetics, Inc., Rockville, MD, USA).
Immunohistochemistry indicated that the tumor cells were positive
for CD38 and CD138 (Fig. 3). The
blood count demonstrated a hemoglobin concentration of 108 g/l, a
white cell count of 6.07×109 cells/l with no abnormal
cells and a platelet count of 143×109 cells/l. The
levels of serum creatinine, calcium and phosphorus were within the
normal range (NR). The erythrosedimentation rate was 113 mm/h, and
the level of serum β2 microglobulin was 4,499 µmol/l (NR, 0.9–2.7
µmol/l). The total serum protein concentration was 83 g/l (NR,
60–83 g/l), and the levels of immunoglobulin (Ig)G, A and M were
39.25, 3.01 and 0.56 g/l, respectively (NR, 7.0–16.0, 0.7–4.0 and
0.4–2.3 g/l, respectively). Immunoelectrophoresis of serum proteins
indicated the presence of an IgG paraprotein, and urine was
positive for Bence-Jones (monoclonal) protein, indicating a
diagnosis of MM (9). Bone marrow
aspiration revealed 4% restriction of plasma cells, and whole body
bone emission CT demonstrated multiple abnormal distribution of
tracer concentration. Consequently, a diagnosis of MM was
established.
The patient and his relatives refused further
examination, surgical operation and radiotherapy, due to the
patient's age and body condition. Therefore, the patient was
subjected to chemotherapy, and was administered 2 cycles of
cyclophosphamide and thalidomide in combination with dexamethasone.
Follow-up imaging 4 months later revealed nearly complete
disappearance of the intracranial tumor mass (Fig. 1B) and renal infiltration (Fig. 2B). The clinical condition also
improved, and the patient experienced a complete recovery.
Discussion
EMP is a rare malignant neoplasm that develops due
to uncontrolled plasma cell proliferation and monoclonal
plasmacytic infiltration (10). EMPs
may coexist with MM, presenting as the main symptom, developing
during the course of MM, or occasionally occurring as isolated
tumors (11,12). Intracranial extramedullary
plasmacytomas account for 4% of all primary plasma cell tumors
(3). In patients with a diagnosis of
MM, the presence of intracranial EMPs, as a result of the
metastatic spread of MM, is rare, occurring in 1% of all the
reported cases (13,14). To the best of our knowledge, <30
cases of renal plasmacytoma have been reported in the literature
previously (15). In the cases of
renal EMPs, the tumor mass is mostly confined to this anatomical
area, and <10% involve other organs besides the kidney (16,17). Thus,
to the best of our knowledge, the initial presentation of an EMP
displaying intracranial and renal infiltration simultaneously, such
as in the present case, has not been previously described.
The diagnosis of EMP is more complicated than that
of MM, and requires radiological, hematological, biochemical and
histological examinations. Due to the absence of typical clinical
symptoms and evidence from specific laboratory tests, a diagnosis
of EMP may be delayed or missed, with potentially serious
consequences for the patient. In the present case, EMP was
diagnosed based on the clinical symptoms of the patient, alongside
the imaging findings and the results of the serum Ig
electrophoresis and the histopathological analyses of tissue biopsy
and bone marrow aspirate.
To date, there are no specific guidelines for the
treatment of EMP presenting with MM. The current treatment options
for EMP include surgery, chemotherapy and radiotherapy, either
alone or in combination (3,15). If the tumor is located in an area with
restricted surgical access, a complete resection with fractionated
radiotherapy at the tumor site may be a good option for
intracranial plasmacytomas. However, a number of case reports have
highlighted the use of systemic chemotherapy and radiotherapy as
the most important part of the treatment (18,19).
Recent studies on the fundamental molecular mechanisms responsible
for MM cell growth and survival have led to the introduction of
novel classes of pharmacological agents, including immunomodulatory
drugs and proteasome inhibitors (20). In the present case, combined
chemotherapy was selected as the treatment for EMP, due to the
patient's age and body condition. In this context, chemotherapy may
be an attractive option for certain cases, for example when the
treatment is aimed at improving the quality of life of patients
rather than at increasing the survival rate, particularly in
elderly patients.
In conclusion, the simultaneous presentation of EMP
in the kidney and head is rare. Thus, the present case report may
aid in the diagnosis and treatment of future cases of EMPs.
References
|
1
|
Kyle RA, Gertz MA, Witzig TE, Lust JA,
Lacy MQ, Dispenzieri A, Fonseca R, Rajkumar SV, Offord JR, Larson
DR, et al: Review of 1027 patients with newly diagnosed multiple
myeloma. Mayc Clin Proc. 78:21–33. 2003. View Article : Google Scholar
|
|
2
|
Barlogie B, Epstein J, Selvanavagam P and
Alexanian R: Plasma cell myeloma - new biological insights and
advances in therapy. Blood. 73:865–879. 1989.PubMed/NCBI
|
|
3
|
Cerase A, Tarantino A, Gozzetti A, Muccio
CF, Gennari P, Monti L, Di Blasi A and Venturi C: Intracranial
involvement in plasmacytomas and multiple myeloma: A pictorial
essay. Neuroradiology. 50:665–674. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Turhal N, Henehan MD and Kaplan KL:
Multiple myeloma: A patient with unusual features including
intracranial and meningeal involvement, testicular involvement,
organomegaly, and plasma cell leukemia. Am J Hematol. 57:51–56.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kanoh T, Katoh H, Izumi T, Tsuji M and
Okuma M: Renal plasmacytoma. Rinsho Ketsueki. 34:1470–1473. 199.(In
Japanese).
|
|
6
|
Chao MV, Gibbs P, Wirth A, et al:
Radiotherapy in the management of solitary extramedullary
plasmacytoma. Inter Med J. 35:211–215. 2005. View Article : Google Scholar
|
|
7
|
Alexiou C, Kau RJ, Dietzfelbinger H,
Kremer M, Spiess JC, Schratzenstaller B and Arnold W:
Extramedullary plasmacytoma: Tumor occurrence and therapeutic
concepts. Cancer. 85:2305–2314. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Reed V, Shah J, Medeiros LJ, Ha CS,
Mazloom A, Weber DM, Arzu IY, Orlowski RZ, Thomas SK, Shihadeh F,
et al: Solitary plasmacytomas: outcome and prognostic factors after
definitive radiation therapy. Cancer. 117:4468–4474. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kyle RA, Larson DR, Therneau TM,
Dispenzieri A, Melton LJ III, Benson JT, Kumar S and Rajkumar SV:
Clinical course of light-chain smouldering multiple myeloma
(idiopathic Bence Jones proteinuria): A retrospective cohort study.
Lancet Haematol. 1:e28–e36. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Laso FJ, Tabernero MD and Iglesias-Osma
MC: Extramedullary plasmacytoma: A localized or systemic disease?
Ann Intern Med. 128:1561998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jancelwicz Z, Takatsuki K, Sugai S and
Pruzanski W: IgD multiple myeloma. Review of 133 cases. Arch Intern
Med. 135:87–93. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dimopoulos MA, Kiamouris C and Moulopoulos
LA: Solitary plasmacytoma of bone and extramedullary plasmacytoma.
Hematol Oncol Clin North Am. 13:1249–1257. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fassas AB, Muwalla F, Berryman, Benramdane
R, Joseph L, Anaissie E, Sethi R, Desikan R, Siegel D, Badros A, et
al: Myeloma of the central nervous system: Association with
high-risk chromosomal abnormalities, plasmablastic morphology and
extramedullary manifestations. Br J Haematol. 117:103–108. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nieuwenhuizen L and Biesma DH: Central
nervous system myelomatosis: Review of the literature. Eur J
Haematol. 80:1–9. 2008.PubMed/NCBI
|
|
15
|
Zhang SQ, Dong P, Zhang ZL, Wu S, Guo SJ,
Yao K, Li YH, Liu ZW, Han H, Qin ZK, et al: Renal plasmacytoma:
Report of a rare case and review of the literature. Oncol Lett.
5:1839–1843. 2013.PubMed/NCBI
|
|
16
|
Solomito VL and Grise J: Angiographic
findings in renal (extramedullary) plasmacytoma. Case report.
Radiology. 102:559–560. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Catalona WJ and Biles JD III: Therapeutic
considerations in renal plasmacytoma. J Urol. 111:582–598.
1974.PubMed/NCBI
|
|
18
|
Bindal AK, Bindal RK, van Loveren H and
Sawaya R: Management of intracranial plasmacytoma. J Neurosurg.
83:218–221. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gozzetti A, Cerase A, Lotti F, Rossi D,
Palumbo A, Petrucci MT, Patriarca F, Nozzoli C, Cavo M, Offidani M,
et al: GIMEMA (Gruppo Italiano Malattie Ematologiche dell'Adulto)
Myeloma Working Party: Extramedullary intracranial localization of
multiple myeloma and treatment with novel agents: A retrospective
survey of 50 patients. Cancer. 118:1574–1584. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Raab MS, Podar K, Breitkreutz I,
Richardson PG and Anderson KC: Multiple myeloma. Lancet.
374:324–339. 2009. View Article : Google Scholar : PubMed/NCBI
|